Abstract
The term "respiratory disease" is used to describe a wide range of conditions that may affect the lungs, bronchi, trachea, and other tissues involved in breathing. The reasons for these conditions might range from infections and allergies to environmental pollutants and genetic predisposition. The purpose of this research is to explain what causes respiratory problems and how to treat them. Some of the respiratory diseases that will be studied include asthma, COPD, pneumonia, tuberculosis, and lung cancer. Part one of this project will provide an overview of the respiratory system and how it functions, while Part two will zero in on the root causes and preventative measures for common respiratory problems. What follows is a detailed explanation of the most common respiratory illnesses, including their symptoms, causes, and diagnosis. The project's final stage will include the pharmaceutical and non-pharmaceutical management of respiratory illnesses. Topics include recent advances in the field such as targeted medications and immunotherapy. The main objective is to provide a comprehensive overview of respiratory illnesses that may be used as a resource by clinicians, researchers, and patients alike.
Keywords
Respiratory Diseases, Lung, COPD, Asthma, TB, Allergy
Introduction
Respiratory infections affect the respiratory system, which consists of the organs and tissues necessary for breathing. The respiratory system consists of the lungs, the trachea, the bronchi, and other parts of the airways(1). Respiratory problems may have a wide variety of causes, including infections, environmental factors, allergies, and heredity. Diseases of the respiratory system include a wide range of conditions, including the most common ones such as asthma, COPD, pneumonia, bronchitis, emphysema, and lung cancer(2). Some of the numerous symptoms of a respiratory disease include coughing, wheezing, shortness of breath, chest tightness, fatigue, and fever. Patients with respiratory disorders may benefit by altering their surroundings and behaviors in addition to medicinal procedures such as bronchodilators, steroids, and antibiotics. Sometimes the only option is hospitalization or surgery for respiratory disorders. (3)
Types of Respiratory Diseases
Among the many respiratory system illnesses, including but not limited to Inflammation and narrowing of the airways are the root causes of asthma's breathing difficulties(4). Chronic obstructive pulmonary disease (COPD) is an umbrella term for a group of lung diseases that cause airflow limitation and include chronic bronchitis and emphysema. Pneumonia is an infection of the lungs caused by bacteria, viruses, or other microbes. The lungs are the most common site of infection for tuberculosis (TB), a bacterial illness. The flu virus may produce a respiratory infection that manifests as aches and pains in addition to the typical fever and cough. In pulmonary fibrosis, lung tissue becomes scarred and thickened, making it hard to breathe. Lung cancer is the malignant enlargement of lung tissue and Allergy(5).
ASTHMA:
Asthma is a respiratory condition characterized by inflammation and swelling of the bronchial airways. Wheezing, coughing, and a tight sensation in the chest are only some of the symptoms of this disorder, which is characterized by inflammation and constriction of the airways and makes it difficult to breathe. Asthma may be triggered in several ways and at varied rates, depending on the individual and their exposure to allergens, air pollution, exercise, stress, or respiratory infections (6). Asthma is often identified in kids; however, it may affect people of any age. Despite the lack of a cure, asthma may be managed using medication, adjustments to one's lifestyle, and the avoidance of asthma triggers. Asthma is often treated with inhaled bronchodilators (which relax the muscles around the airways) and inhaled corticosteroids (which reduce inflammation in the airways). To effectively manage your asthma, you and your doctor must collaborate on a personalized treatment plan that addresses your unique needs, identifies and avoids anxiety triggers, and ensures that, with proper care, you can lead a normal, healthy life.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE:
Breathing becomes more difficult with the progressive decline of chronic obstructive pulmonary disease (COPD). Smoking cigarettes, breathing polluted air, and being exposed to chemicals and dust at work are all potential triggers for COPD (7). The two most frequent types of COPD are chronic bronchitis and emphysema. Chronic bronchitis is characterized by a persistent cough with mucus formation, whereas emphysema is characterized by a loss of the small air sacs in the lungs, reducing the lungs' ability to take in oxygen and expel carbon dioxide. Breathlessness, wheezing, chest tightness, a persistent cough, and frequent respiratory infections are all symptoms of chronic obstructive pulmonary disease (COPD). A person's quality of life might be severely diminished by chronic obstructive pulmonary disease (COPD). The most effective treatment for chronic obstructive pulmonary disease (COPD) is a multifaceted approach that includes medication (such as bronchodilators or steroids) to open airways and decrease inflammation, as well as behavioral changes (such as giving up smoking, reducing exposure to lung-irritating chemicals, and participating in pulmonary rehabilitation) to improve lung function and general health. In extreme cases, a lung transplant may be necessary(2).
PNEUMONIA:
Pneumonia is an inflammatory disease affecting the lung tissue, and it may be caused by bacteria, viruses, fungi, or parasites. Infants, the elderly, and people with weakened immune systems are the most in danger, but anybody may become infected (8). These symptoms, together with fever, chest pain, shortness of breath, tiredness, and weakness, are classic indicators of pneumonia. Symptoms may range in intensity from barely perceptible to lethal. Bacterial pneumonia is often treated with antibiotics, whereas viral pneumonia is treated with antiviral drugs. Rest, plenty of water, and over-the-counter pain and fever relievers may help alleviate symptoms. Oxygen therapy, intravenous fluids, and mechanical ventilation are all possible treatments that may be necessary in the hospital. Regular hand washing, avoiding contact with people who are sick with respiratory infections, and vaccination against the most common bacterial and viral agents that cause pneumonia are all effective ways to avoid getting pneumonia. Avoiding risk factors for pneumonia includes not smoking and managing chronic conditions like asthma and chronic obstructive pulmonary disease.
TUBERCULOSIS:
Bacterium Tuberculosis (TB) is an infectious illness caused by Mycobacterium tuberculosis. Damage occurs most often in the lungs but may also occur in other organs and systems such as the kidneys, spine, and brain. The TB virus is spread when a person breathes in the airborne particles that are produced when an infected person coughs, sneezes, or talks (9). Tuberculosis is characterized by a prolonged cough (lasting more than three weeks), chest pain, coughing up bloody or sputum-like mucus, fatigue, fever, and night sweats. There may be no symptoms at all in some people with tuberculosis. A complete medical history, physical examination, sputum culture, and nucleic acid amplification tests may all aid in diagnosing TB. Drugs for tuberculosis therapy must be used daily for six to nine months, under close medical monitoring to guarantee efficacy(10). The Bacille Calmette-Guérin (BCG) vaccination is widely used to protect children against tuberculosis in regions where the disease is prevalent. People may lessen their chances of getting TB by taking medicines, maintaining strict cleanliness, and staying away from infected people. Latent tuberculosis infection may be kept from developing into active TB disease with the use of medication. (11)
INFLUENZA:
The flu virus is responsible for a highly contagious respiratory illness that often presents as a sore throat, cough, and sometimes pneumonia. Multiple strains of the influenza virus may produce symptoms ranging from mild discomfort to life-threatening illness(12). High fever, a hacking cough, a sore throat, a runny or stuffy nose, aching muscles, a throbbing head, chilled extremities, and intense weariness are just some of the unpleasant symptoms that may accompany the flu. Although many people recover from the flu within a week or two, those with compromised immune systems, the elderly, and young children are at a far higher risk of developing pneumonia as a result of their exposure to the virus(13). When an infected individual sneezes, coughs, or talks, the virus spreads through the air in the form of droplets. Contact with an infected surface or object followed by touching one's mouth, nose, or eyes is another route of infection. The best strategy to prevent getting the flu is to be vaccinated against it annually, practice good hand hygiene, and limit contact with sick individuals. Get plenty of sleep, drink plenty of fluids, and see a doctor if your flu symptoms persist if you have a history of complications.
PULMONARY FIBROSIS:
Pulmonary fibrosis is a disorder that occurs when scarring or fibrosis develops in the lungs. Scarring makes it difficult for the lungs to function normally, which may lead to decreased oxygen levels in the blood. Pulmonary fibrosis may have a wide variety of causes, including but not limited to radiation therapy, some medicines, autoimmune diseases, and genetics. The cause of pulmonary fibrosis is frequently unknown (14). Breathing problems, a dry, persistent cough, fatigue, weight loss, chest discomfort, and shortness of breath are all indications of pulmonary fibrosis. It may become more challenging for patients with pulmonary fibrosis to carry out daily activities if these symptoms increase with time. Although there is presently no cure for pulmonary fibrosis, treatments exist that may help with symptoms and slow the progression of the condition. Treatment options range from medication and oxygen treatment to pulmonary rehabilitation and lung transplantation. Patients with pulmonary fibrosis should work with their medical teams to manage their symptoms and undergo regular assessments to see whether their treatment is effective.
ALLERGY:
An allergic response ensues when the immune system overreacts to a normally safe chemical (an allergen). Allergens are substances that may cause an allergic reaction in a person and can be found everywhere(15). When an allergic person is exposed to an allergen, their immune system responds by producing antibodies against it. These antibodies are known as immunoglobulin E (IgE). The production of histamine and other chemicals in the body, activated by these antibodies, may cause a variety of symptoms, including sneezing, runny nose, itching, hives, swelling, and even anaphylaxis (16). People of all ages are susceptible to developing allergies, and the intensity of these reactions may vary widely. Allergies may be either seasonal or persistent. Even adults may develop allergies at any time. The first and foremost crucial step in managing allergies is avoiding allergens. In severe cases, allergy injections may desensitize the immune system, while antihistamines and corticosteroids may help reduce symptoms. Preventing allergic responses is possible by avoiding allergens, maintaining a healthy lifestyle, and not smoking. Medical attention should be sought if symptoms do not improve or worsen over time (17). Allergies may significantly impact a person's quality of life, but they can have a normal, healthy life with proper care.
LUNG CANCER:
Lung cancer is the most common kind of cancer in the United States. It is one of the most common types of cancer and a leading cause of cancer-related death worldwide(11). Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are the two most common forms of lung cancer. Eighty to eighty-five percent of lung cancer cases are NSCLC, whereas only ten to fifteen percent are SCLC. Lung cancer is most often caused by actively smoking cigarettes, cigars, or pipes, or by being exposed to secondhand smoke. Lung cancer risk factors include exposure to environmental toxins such as radon and asbestos, in addition to a personal or family history of the disease (18). Lung cancer symptoms may include a persistent cough, chest pain, shortness of breath, hoarseness, coughing up blood, extreme fatigue, and a loss of weight for no apparent reason. However, certain forms of lung cancer may not exhibit symptoms until they have advanced sufficiently. Lung cancer treatment options vary by cancer kind and stage but may include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or a combination of these. Those who are at a high risk of acquiring lung cancer may be encouraged to be screened regularly. This may be because early detection is crucial in successfully treating the condition (19). Avoiding tobacco smoking and other environmental contaminants are just two of several important preventative actions against lung cancer.
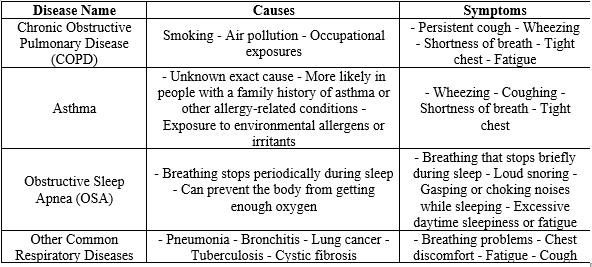
Table 1: Respiratory Diseases Overview
Diagnosis
Diagnosing lung diseases involves a comprehensive approach that integrates patient history, physical examination, and various diagnostic tests to accurately identify the specific type and severity of the condition. Initially, a thorough patient history and physical examination are conducted, focusing on symptoms such as chronic cough, dyspnea, and chest pain, alongside risk factors like smoking history and occupational exposures (1). Pulmonary function tests (PFTs) are essential, with spirometry and diffusion capacity tests helping to differentiate between obstructive and restrictive lung diseases. For instance, a reduced forced expiratory volume in one second (FEV1) with a low FEV1/FVC ratio indicates obstructive lung disease like COPD, while a reduced total lung capacity suggests restrictive disease. Imaging studies, including chest X-rays and high-resolution computed tomography (HRCT), play a crucial role, with HRCT being the gold standard for evaluating lung parenchyma in diseases such as idiopathic pulmonary fibrosis (IPF) and hypersensitivity pneumonitis. Positron emission tomography (PET) scans are valuable for diagnosing and staging lung cancer. Laboratory tests, including blood tests and sputum analysis, support diagnosis by identifying infectious agents and inflammatory markers. Bronchoscopy and lung biopsy provide direct visualization and tissue samples for definitive diagnosis, particularly for interstitial lung diseases when non-invasive methods are inconclusive. Advances in molecular diagnostics and genetic testing are increasingly used to identify specific genetic mutations, guiding targeted therapies for lung cancer. Emerging technologies like artificial intelligence and machine learning enhance the accuracy of interpreting imaging studies and predicting disease progression. This multi-faceted approach ensures early and precise diagnosis, crucial for effective management and improved patient outcomes. Continuous advancements in diagnostic technologies promise even more precise and personalized approaches to lung disease diagnosis in the future (20).
RESULTS AND DISCUSSION
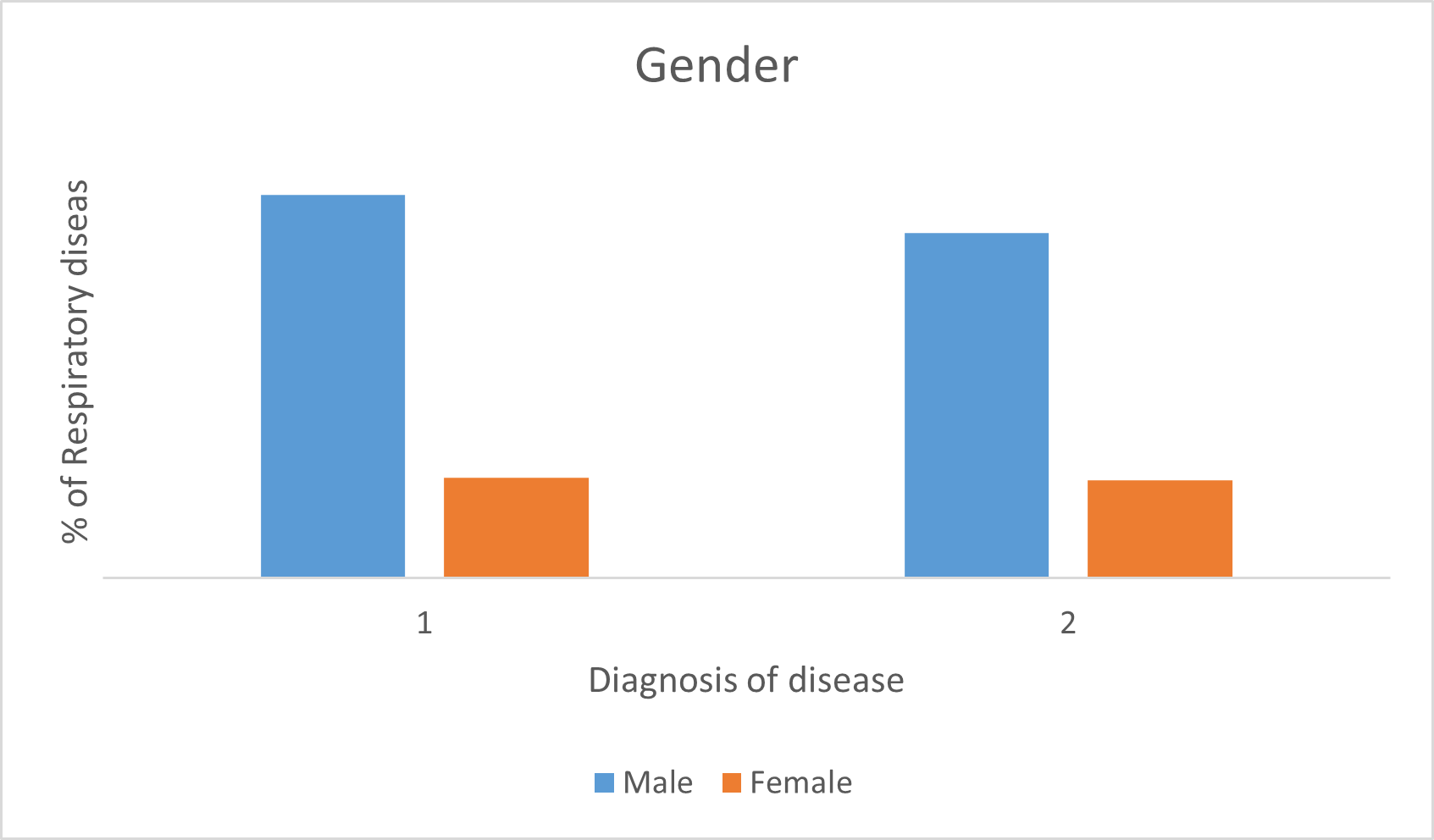
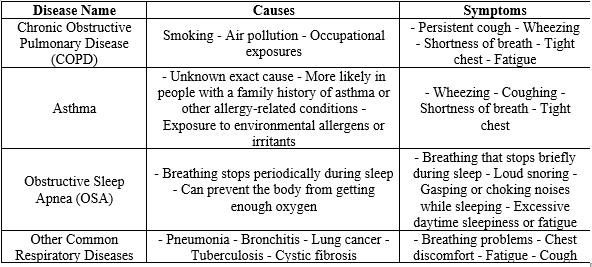
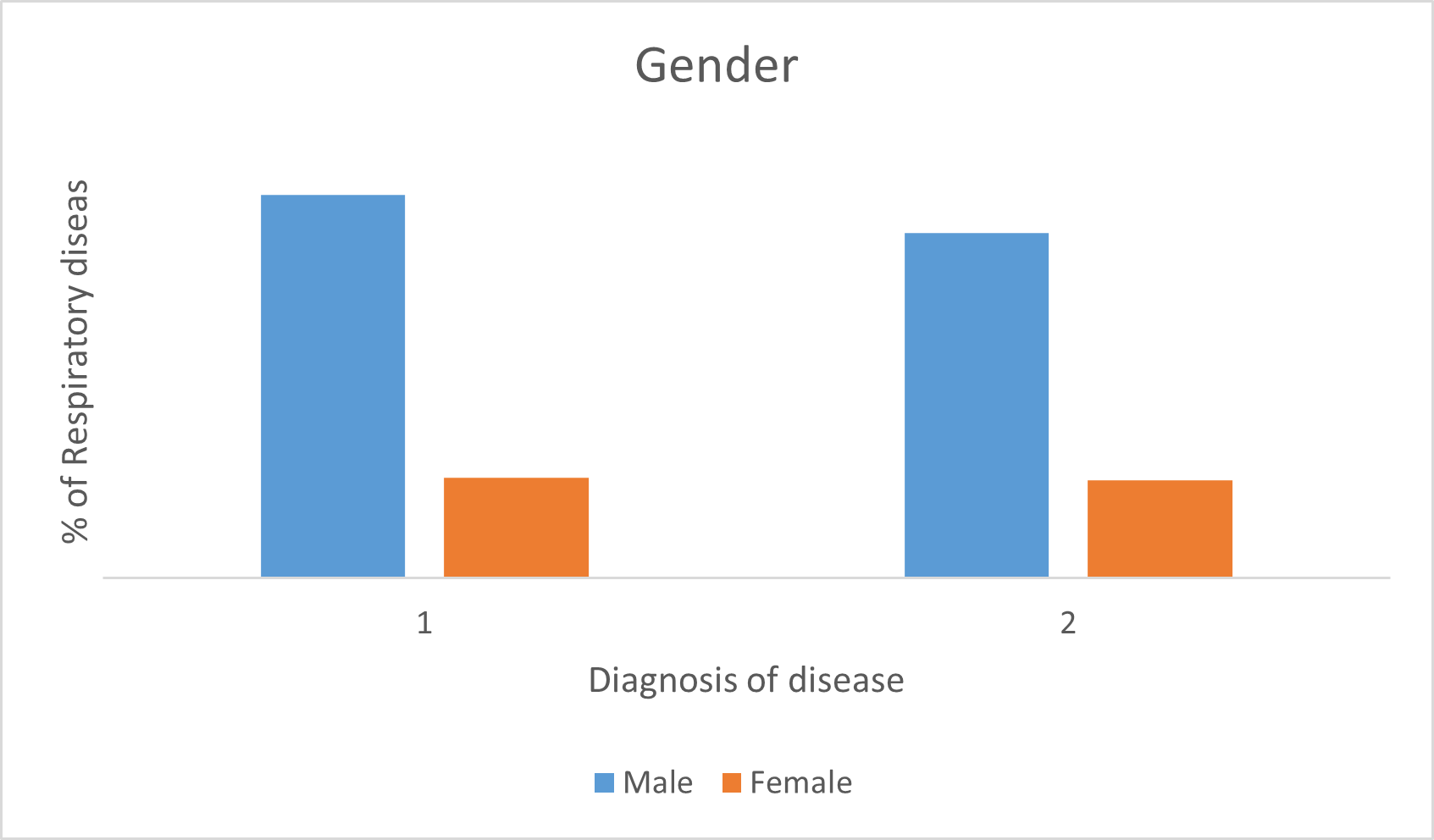
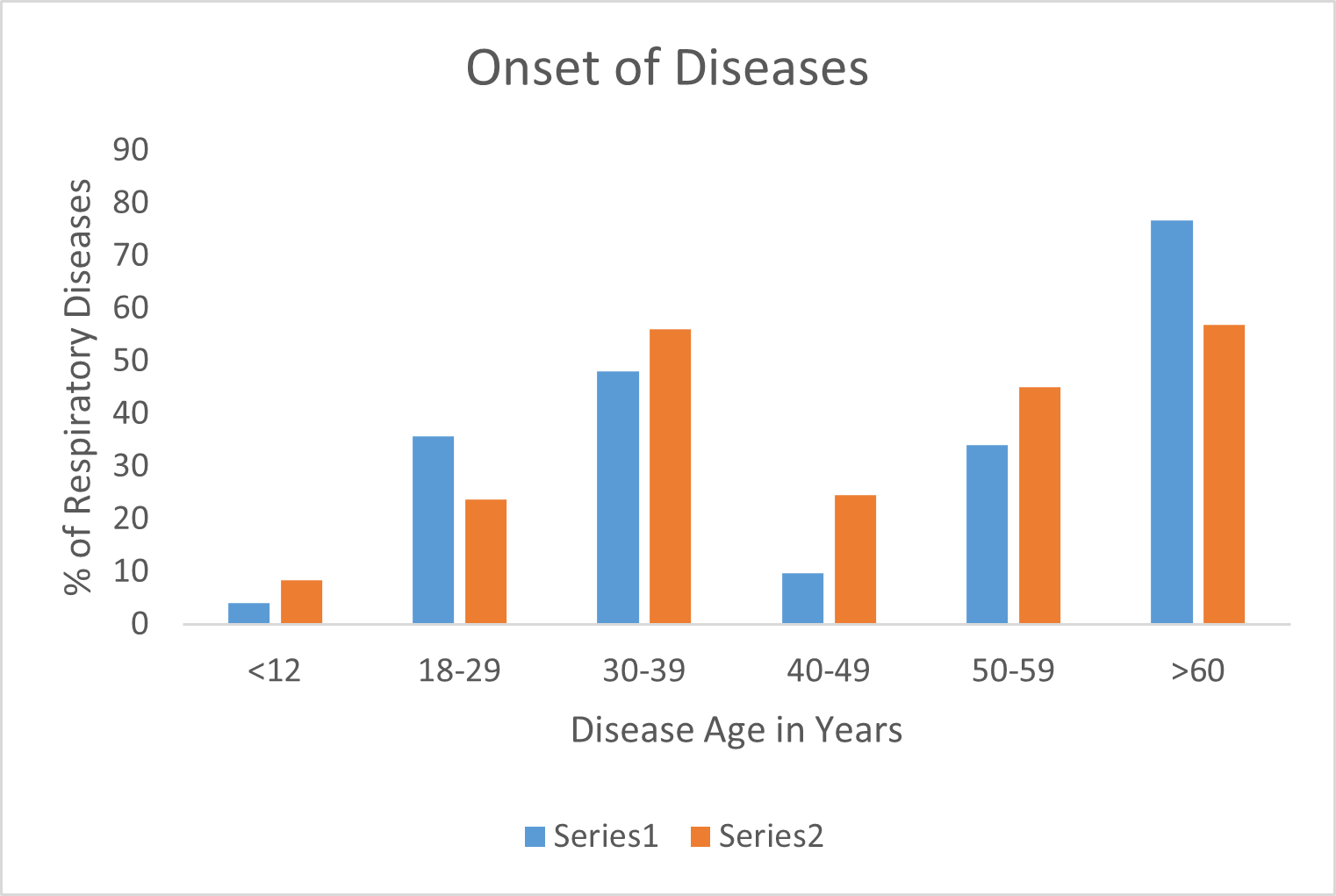
Fig 1: Comparative Analysis of Respiratory Diseases based on gender.
The "Gender" chart reveals a pronounced disparity in respiratory disease diagnoses, with males showing significantly higher prevalence in both Series 1 and Series 2. This disparity is influenced by higher smoking rates among males, contributing to a greater burden of diseases like COPD and lung cancer. Additionally, males are more frequently exposed to occupational hazards such as dust and chemicals, increasing respiratory morbidity. Biological differences in lung structure and function may also contribute to the observed gender differences in disease prevalence . Conversely, the lower incidence in females may reflect underdiagnosis or differences in health-seeking behavior and exposure risks.
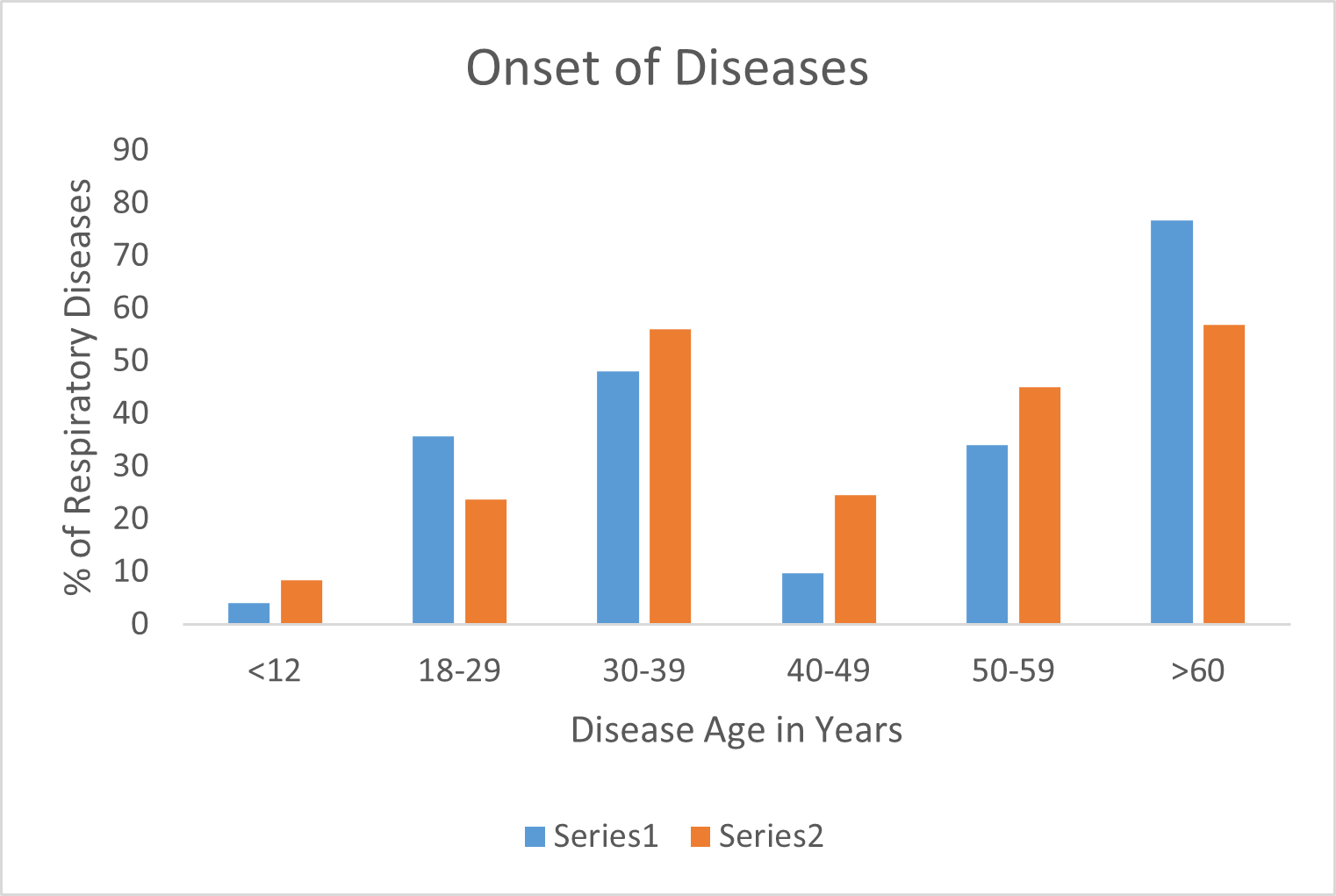
Fig 2: Comparative Analysis of Respiratory Diseases based on age.
The "Onset of Diseases" chart highlights a significant prevalence of respiratory diseases among individuals over 60 years of age, with approximately 70% in Series 1 and 50% in Series 2. This high prevalence can be attributed to factors such as cumulative exposure to environmental pollutants, age-related physiological changes, and a higher incidence of comorbidities like cardiovascular disease and diabetes that exacerbate respiratory conditions. Additionally, the notable incidence in the 30-39 age group, particularly in Series 1, indicates that respiratory diseases are not limited to the elderly. This younger demographic may be affected by occupational exposures, smoking, and lifestyle choices that increase the risk of developing respiratory ailments
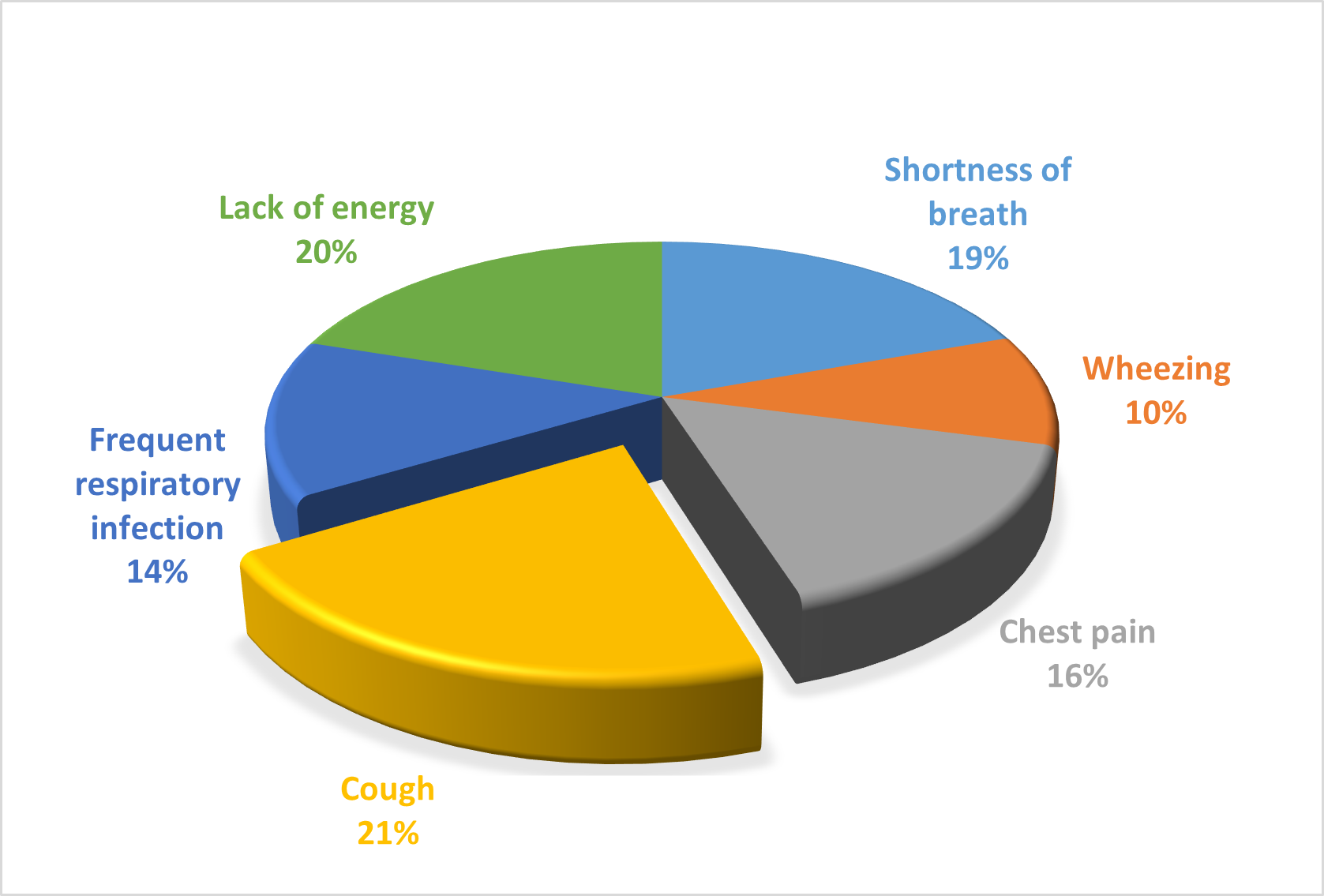
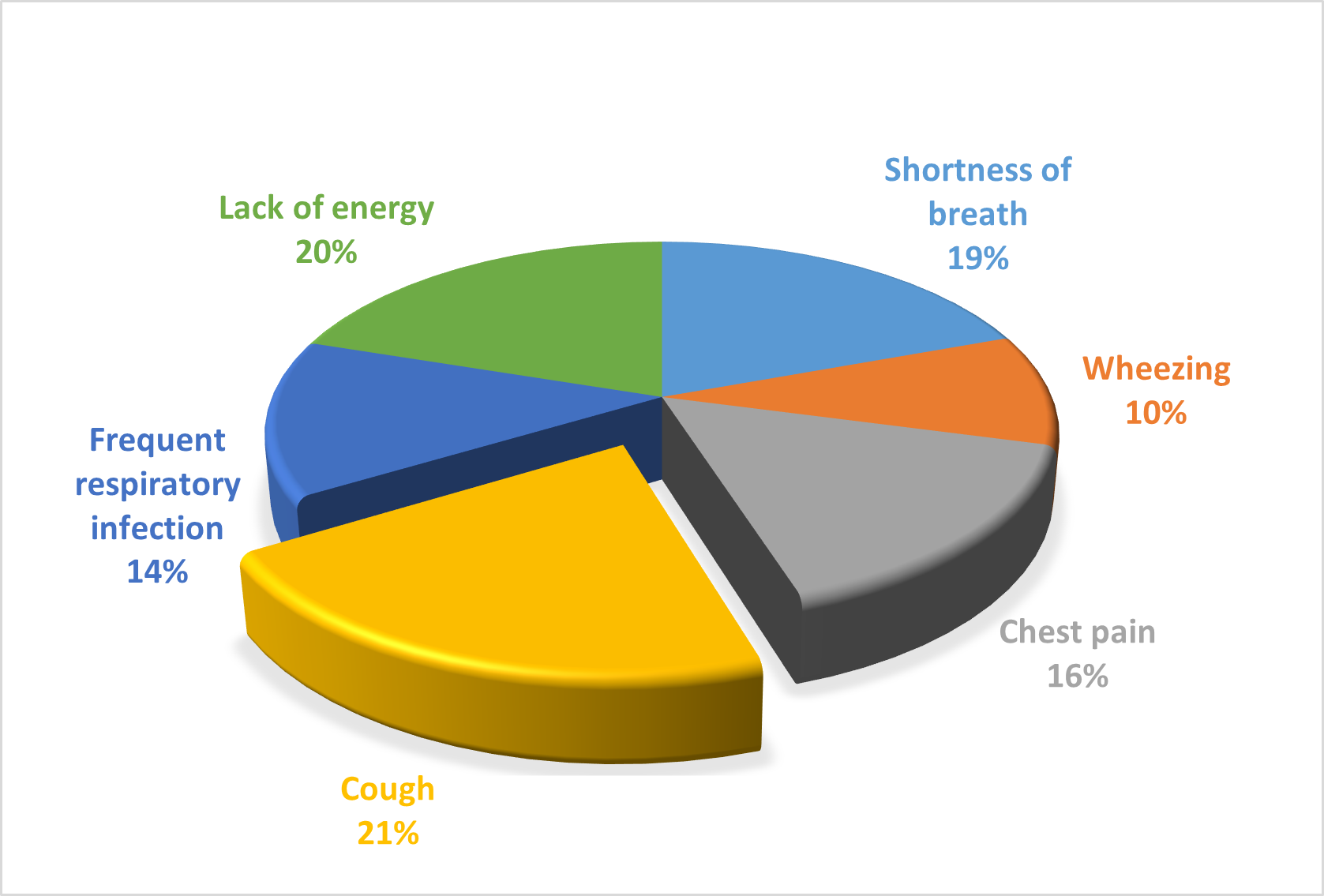
Fig 3: Comparative Analysis of Respiratory Diseases based on Symptoms.
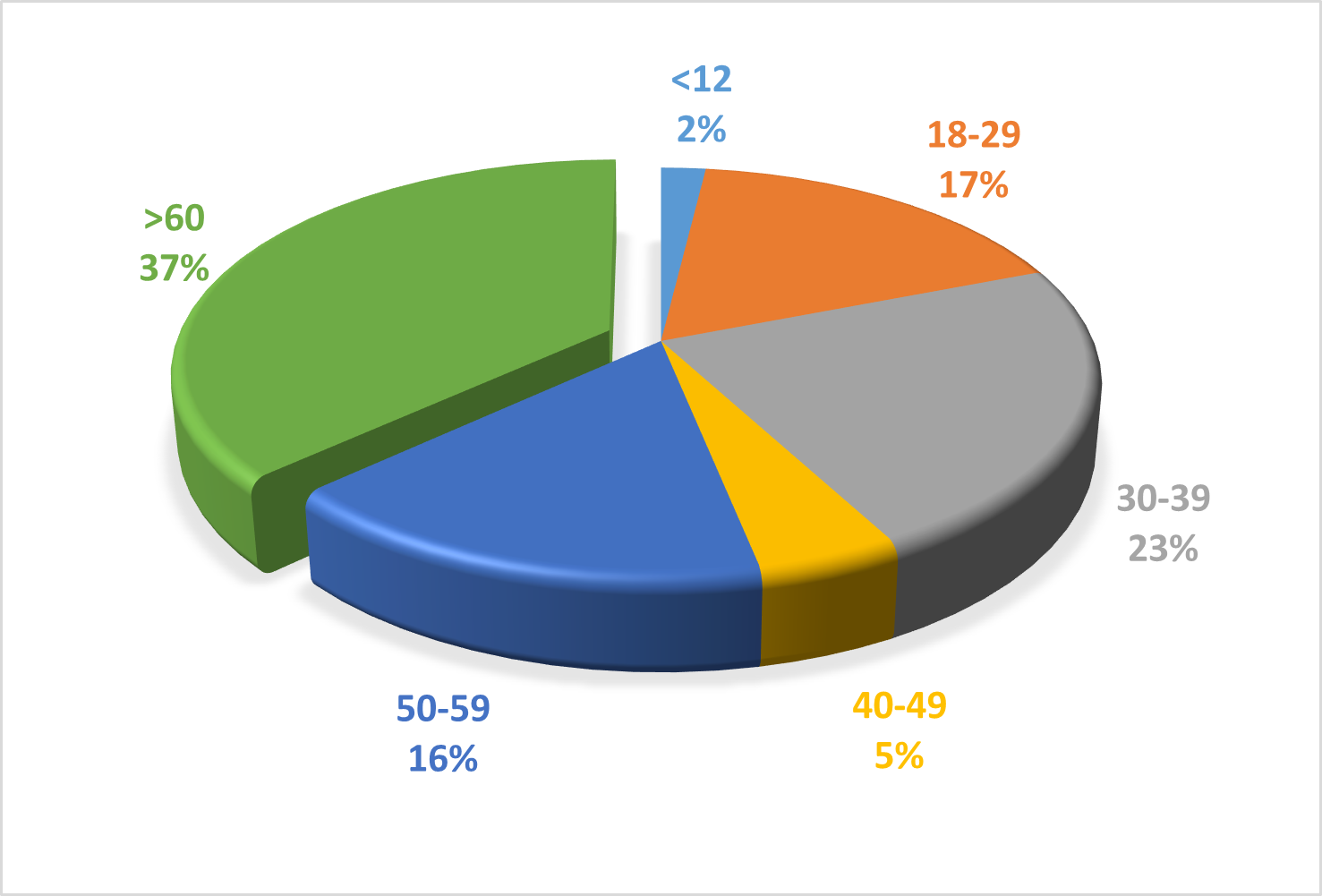
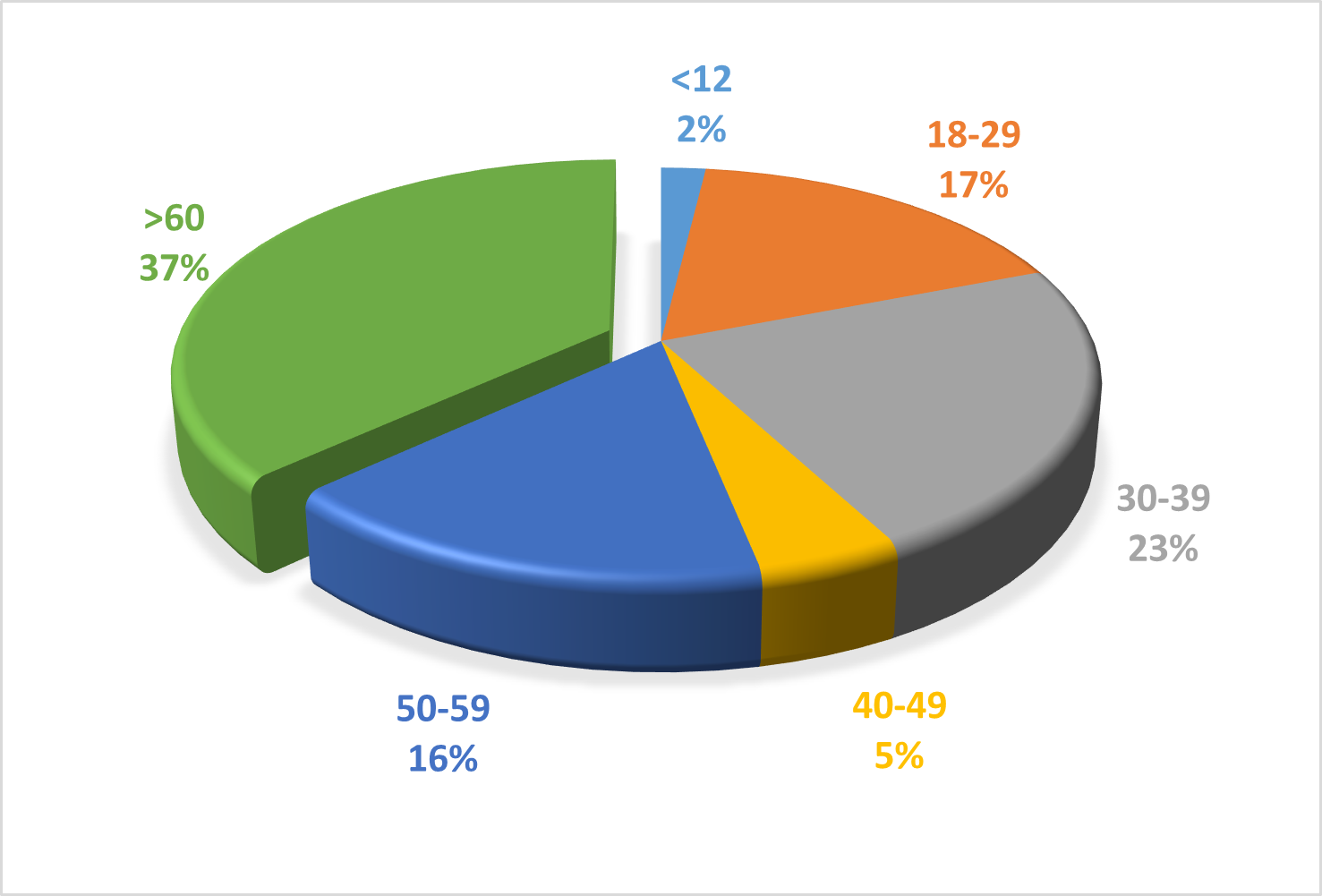
Fig 4: Comparative Analysis of Respiratory Diseases on Severity in Different Age.
The pie charts provide a comprehensive overview of respiratory diseases, highlighting both the age distribution of affected individuals and the prevalence of various symptoms. The first chart shows that respiratory diseases predominantly affect individuals over 60 years of age, who constitute 37% of the cases. This is followed by the 30-39 age group at 23%, the 18-29 age group at 17%, the 50-59 age group at 16%, the 40-49 age group at 5%, and children under 12 years at 2%. This age distribution underscores the higher vulnerability of older adults to respiratory diseases, likely due to factors such as age-related decline in immune function and the cumulative effect of environmental exposures. The second chart details the symptoms experienced by patients with respiratory diseases. Cough (21%) and lack of energy (20%) are the most common symptoms, significantly impacting patients' quality of life. Shortness of breath (19%) is also prevalent, often correlating with disease severity and necessitating comprehensive management strategies. Chest pain (16%), frequent respiratory infections (14%), and wheezing (10%) are other notable symptoms, each contributing to the overall disease burden and requiring specific diagnostic and therapeutic approaches . Together these charts illustrate the broad impact of respiratory diseases across different age groups and highlight the diverse symptoms that healthcare providers must address to improve patient outcomes.
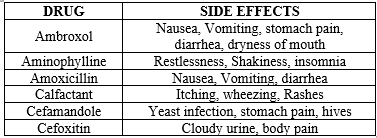
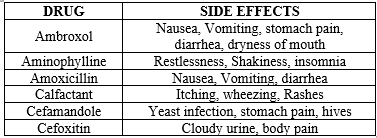
Table 2: Therapeutic agents with adverse events for respiratory diseases.
espiratory problems may cause sickness in the lungs, bronchi, trachea, and other areas of the respiratory system. The future course of respiratory illnesses will be determined by advances in medicine, research, and public health. Future progress in genetics, genomics, and proteomics may provide personalized therapy for respiratory illnesses. In this way, doctors may tailor treatments to everyone’s genetic and molecular profile, resulting in more effective care with fewer side effects. Gene therapy has enormous potential as a treatment for respiratory diseases. Genetic anomalies are often at the core of respiratory diseases, and they might be treated by medical specialists utilizing genetic engineering techniques. Telemedicine has been a lifesaver in fighting against respiratory infections during the COVID-19 pandemic. Telemedicine may be used in the future to remotely monitor patients' respiratory symptoms and change treatment approaches. Flu and pneumonia vaccines have gone a long way over the years, making them a crucial tool in the battle against respiratory illnesses. Improved adjuvants and delivery technologies point to a future when better immunizations may be achievable. Smoking cessation initiatives, reduced air pollution, and early diagnosis and treatment of respiratory disorders are all examples of public health policies that may help prevent the onset of these diseases and improve the quality of life for those who currently suffer from them. The future of respiratory illnesses will be influenced by recent medical advances, scientific discoveries, and public health initiatives. By focusing on these underlying causes, we may assist the millions of individuals throughout the world who suffer from respiratory problems.
CONCLUSION
The researchers wanted to find out how common and severe respiratory problems are among the general population. Many of those who took the survey said they had been diagnosed with some kind of respiratory illness, highlighting the prevalence of these problems. Conditions involving the respiratory system were the most often reported, with asthma, COPD, and allergies being the most common. The impact of respiratory problems on people's quality of life was highlighted by the fact that many respondents had respiratory symptoms such as shortness of breath, coughing, and wheezing. They were unable to exercise or hang out with pals as usual because of these problems. The need to spread awareness about respiratory illnesses, their root causes, and available treatment options was emphasized throughout the research. Spreading awareness about preventive measures and encouraging early identification and treatment is crucial. Avoiding environmental toxins and quitting smoking are only two examples In conclusion, the results of the survey study on respiratory illnesses provide important insight into the breadth and depth of these problems. The findings stress the need for more research and public education in respiratory health.
ACKNOWLEDGMENTS
We authors gratefully acknowledge all participants for their invaluable contributions to this survey-based research and extend our sincere thanks to our colleagues and funding bodies for their support.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- Viegi G, Maio S, Fasola S, Baldacci S. Global Burden of Chronic Respiratory Diseases. https://home.liebertpub.com/jamp [Internet]. 2020 Jul 28 [cited 2024 May 8];33(4):171–7. Available from: https://www.liebertpub.com/doi/10.1089/jamp.2019.1576
- Holland WW, Halil T, Bennett AE, Elliott A. Factors Influencing the Onset of Chronic Respiratory Disease. Br Med J [Internet]. 1969 Apr 26 [cited 2024 May 8];2(5651):205–8. Available from: https://www.bmj.com/content/2/5651/205
- Schiermeier Q. Climate and weather: Extreme measures. Nature. 2011 Sep 8;477(7363):148–9.
- Smith KR. National burden of disease in India from indoor air pollution. PNAS. 2000 Nov 21;97(24):13286–93.
- Carter P, Lagan J, Fortune C, Bhatt DL, Vestbo J, Niven R, et al. Association of Cardiovascular Disease With Respiratory Disease. J Am Coll Cardiol [Internet]. 2019 May 7 [cited 2024 May 8];73(17):2166–77. Available from: https://www.jacc.org/doi/10.1016/j.jacc.2018.11.063
- Baïz N, Annesi-Maesano I. Is the asthma epidemic still ascending? Clin Chest Med. 2012 Sep;33(3):419–29.
- Ferkol T, Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc [Internet]. 2014 Mar 27 [cited 2024 May 8];11(3):404–6. Available from: http://www.thoracic.org/
- Ayres JG, Forsberg B, Annesi-Maesano I, Dey R, Ebi KL, Helms PJ, et al. Climate change and respiratory disease: European Respiratory Society statement. Eur Respir J. 2008 Aug;34(2):295–302.
- Ogunbayo A. Retrospective Study of Effects of Air Pollution on Human Health. 2016 [cited 2024 May 18]; Available from: http://www.theseus.fi/handle/10024/111047
- Respiratory health effects of indoor air pollution [Review articl...: Ingenta Connect [Internet]. [cited 2024 May 18]. Available from: https://www.ingentaconnect.com/content/iuatld/ijtld/2010/00000014/00000009/art00003
- Schluger NW, Koppaka R. Lung disease in a global context: A call for public health action. Ann Am Thorac Soc. 2014;11(3):407–16.
- Eze JN, Ozoh OB, Otuu FC, Shu EN, Anyaehie BU. Respiratory symptoms and lung function among inmates in a Nigerian prison: a cross sectional study. BMC Pulm Med. 2022 Dec 1;22(1).
- Hulin M, Simoni M, Viegi G, Annesi-Maesano I. Respiratory health and indoor air pollutants based on quantitative exposure assessments. Eur Respir J. 2012 Oct 1;40(4):1033–45.
- Majewski S, Piotrowski WJ. Air Pollution—An Overlooked Risk Factor for Idiopathic Pulmonary Fibrosis. Journal of Clinical Medicine 2021, Vol 10, Page 77 [Internet]. 2020 Dec 28 [cited 2024 May 18];10(1):77. Available from: https://www.mdpi.com/2077-0383/10/1/77/htm
- Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011 Aug;41(8):1059–71.
- D’Amato G, Cecchi L, Bonini S, Nunes C, Annesi-Maesano I, Behrendt H, et al. Allergenic pollen and pollen allergy in Europe. Allergy. 2007 Sep;62(9):976–90.
- Brunekreef B, Annesi-Maesano I, Ayres JG, Forastiere F, Forsberg B, Künzli N, et al. Ten principles for clean air. European Respiratory Journal. 2012 Mar 1;39(3):525–8.
- Navarro-Torné A, Vidal M, Trzaska DK, Passante L, Crisafulli A, Laang H, et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. [cited 2024 May 9]; Available from: www.integratedhomecare.eu
- Personal and Family History of Respiratory Disease and Lung Cancer Risk | American Review of Respiratory Disease [Internet]. [cited 2024 May 9]. Available from: https://www.atsjournals.org/doi/abs/10.1164/arrd.1986.134.3.466
- Damiani A, Orlandi M, Bruni C, Bandini G, Lepri G, Scaletti C, et al. The role of lung biopsy for diagnosis and prognosis of interstitial lung disease in systemic sclerosis: a systematic literature review. Respir Res. 2024 Dec 1;25(1


 Hema Arya* 2
Hema Arya* 2
 Shelesh Kumar Bansal 1
Shelesh Kumar Bansal 1
 10.5281/zenodo.11404154
10.5281/zenodo.11404154