Abstract
The tongue plays a pivotal role in various oral functions, including speech, mastication, and deglutition. Its interaction with dentures significantly impacts their stability, retention, and functionality. Understanding the tongue's role is crucial for designing dentures that accommodate its movements and forces. Challenges like tongue thrusting, enlarged tongues, and restricted mobility can complicate prosthetic design. Advances in tongue prosthetics and rehabilitation offer hope for patients with tongue loss or impairment. However, challenges in denture stability and customized solutions for partial glossectomy patients remain. Future directions include digital scanning, 3D printing, biofeedback, and tissue engineering to improve tongue-related prosthetic outcomes.
Keywords
Tongue, Prosthodontics, Denture, Stability, Function, Speech, Mastication.
Introduction
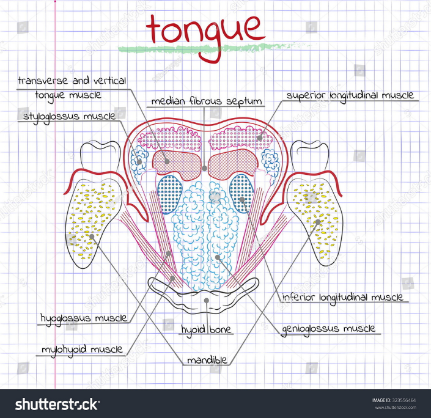
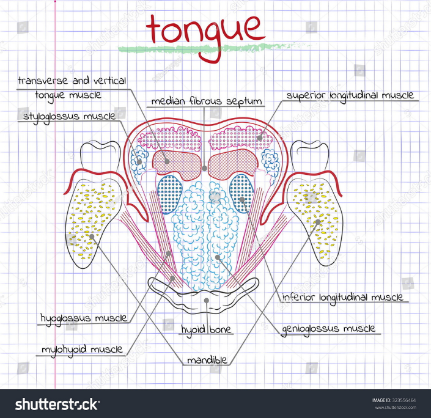
The tongue is a muscular organ anchored to the hyoid bone, mandible, soft palate, pharyngeal wall, and styloid process in the oral cavity. It is crucial for several vital oral and maxillofacial functions, including taste, chewing, and swallowing. The tongue also plays a key role in sucking, speech, receiving food, and articulation. Impairment in any of these activities can significantly affect a patient's socialization and quality of life. Additionally, the tongue is essential for effective speech, helping to form consonants and vowels by contacting specific parts of the teeth, alveolar ridge, or hard palate.1 The tongue is a vital oral structure influencing speech, mastication, deglutition, and overall oral health. Its complex anatomy and dynamic functions play a critical role in prosthodontics, particularly in designing, fabricating, and adapting prostheses. It consists of intrinsic muscles that alter its shape and extrinsic muscles that enable movements like protrusion and retraction. Its surface is divided into the anterior two-thirds (oral part) and posterior one-third (pharyngeal part), covered by a mucosal layer with specialized papillae. Innervated by the hypoglossal nerve (motor), glossopharyngeal and lingual nerves (sensory), and chorda tympani (taste), the tongue plays a crucial role in speech articulation, mastication, bolus formation, and maintaining prosthesis stability and retention in prosthodontics.2 The implications of the tongue in prosthodontics are significant, particularly in the context of rehabilitation following glossectomy or other oral surgeries. The tongue plays a crucial role in speech, swallowing, and overall oral function, making its preservation or restoration vital for patient quality of life. This area plays a crucial role in denture stability during functions such as chewing, swallowing, and speaking, as the direction and magnitude of these forces vary between individuals and over time. How these forces interact with dentures can either enhance their stability or lead to their displacement.3 This article gives an overview of implications of tongue in prosthodontics.

Functional Classification of the Tongue: Implications for Prosthodontic Treatment
The functional classification of the tongue, as outlined by Barnett Kessler, highlights varying levels of tongue activity and their impact on oral health and prosthodontic treatments. The Occupational Tongue refers to individuals whose professions or daily activities necessitate frequent and precise tongue movements. Professions such as those of jurists, teachers, lecturers, preachers, and musicians rely heavily on the tongue’s dexterity for speech and articulation. These individuals often require an enhanced range of motion to perform their roles effectively. In contrast, the Still Tongue, or Passive Tongue, is typically characterized by minimal tongue activity. This may occur due to physical conditions such as injury, deformity, or a congenital issue like ankyloglossia (tongue-tie), which restricts the movement of the tongue. The Normal Tongue refers to a tongue that functions within the typical range of movement necessary for normal oral activities. This category is ideal for prosthodontic treatment as it allows for optimal denture function and stability, facilitating the proper alignment and retention of dental prostheses. On the other hand, the Habitual Tongue exhibits frequent, often forceful movements, typically developed through habitual actions or patterns. These individuals may have a thick and powerful base of the tongue, which can exert significant pressure on dental restorations. Such habitual movements may pose challenges in maintaining the stability and retention of dentures, as the tongue’s forceful actions can potentially dislodge the prosthetic device. Understanding these classifications is crucial for effective prosthodontic planning, as they inform the design and fitting of dentures, taking into account the functional capacity and tendencies of the patient's tongue.3,4
Classification of Tongue Position According to Wright and Its Impact on Denture Stability

Figure 2
Wright’s classification of tongue position plays a significant role in prosthodontic treatment, particularly in the design and fitting of dentures. The Class I Position is considered the most favorable for denture retention and stability. In this position, the floor of the mouth is situated at a higher level, which allows the tongue to adequately cover the lingual flange of the denture. This creates a secure border seal between the tongue and denture, enhancing the stability and retention of the prosthesis while minimizing the risk of overextension. Conversely, the Class II and III Positions are deemed unfavorable for denture function. In these positions, the floor of the mouth is lower, causing the tongue to have insufficient coverage of the denture’s lingual flange. As a result, these positions can lead to several challenges, including poor lingual seal, overextension of the denture flange, and an increased likelihood of denture dislodgement during tongue movements. The instability caused by these positions can make the denture prone to shifting or loosening, particularly during functional movements such as speaking or chewing. From a clinical perspective, the natural resting position of the tongue should be considered when designing dentures, especially in patients with Class II and III positions. Adjustments to the denture are often necessary to optimize the fit and improve its stability, helping to minimize issues related to overextension and discomfort. Ensuring patient comfort is crucial in these cases, as it plays a key role in achieving satisfaction with the prosthesis. Properly addressing these considerations can lead to improved functional outcomes and greater comfort for the patient.3,4
The Impact of Tongue Function on Prosthodontics: Considerations and Challenges
The tongue plays a vital role in the design and functionality of various prosthetic devices in prosthodontics. In complete dentures, the position and movement of the tongue are essential for ensuring retention and stability. A poorly designed denture base can interfere with tongue movements, leading to discomfort and issues with speech, mastication, and swallowing. For partial dentures, the interaction between the tongue and components like clasps or the framework must be carefully considered, as tongue movement can displace ill-fitting prostheses. In fixed prosthodontics, it is crucial to design the prosthesis in a way that accommodates tongue function, avoiding irritation or disruption in speech and swallowing. For implant-supported prostheses, the proprioceptive function of the tongue aids in adapting to the implants, although challenges arise in patients with atrophic or altered tongue anatomy. In post-glossectomy patients, prosthetic solutions, such as palatal augmentation prostheses, are essential to compensate for the loss of tongue volume, thereby improving speech and swallowing capabilities. Several clinical challenges related to tongue function in prosthodontics also arise, including tongue thrusting, which can destabilize prostheses in edentulous patients, often requiring functional training or prosthetic adjustments.5 Additionally, hypertrophic tongue or enlarged tongues complicate prosthesis design and require careful planning to ensure a proper fit. Restricted tongue mobility, as seen in conditions like ankyloglossia (tongue-tie), affects the adaptation and effectiveness of prostheses. Furthermore, the tongue's role in cleaning oral prostheses emphasizes the need for proper oral hygiene practices to maintain both the functionality of the prostheses and overall oral health.6
Bottom of Form
Role of Tongue in Tray Selection and Adjustments for Optimal Prosthetic Fit
When selecting and positioning the mandibular tray, it is crucial to ensure that the patient’s tongue is properly managed to prevent any interference or discomfort. The patient should be instructed to lift and bring the tongue forward during tray placement, which prevents the tongue from becoming trapped beneath the tray. This technique not only ensures that the tongue remains unobstructed but also facilitates an accurate seating of the tray. After positioning the tray, it is essential to assess the lingual borders by observing the functional movements of the tongue, such as extending it straight out. If the tray lifts from the posterior end during such tongue movements, it may indicate an overextension of the distolingual flange, in which case a reduction of the tray's border is necessary for better fit and function. Additionally, tray displacement during specific tongue movements can reveal overextension in various areas. For example, if the tray moves during a right-side tongue movement, it suggests overextension on the left side, particularly around the mylohyoid portion. Conversely, movement during a left-side tongue movement indicates potential overextension on the right side. Displacement toward the soft palate could point to overextension of the anterior portion or the lingual frenum, which should also be addressed. These observations are critical for ensuring that the tray fits comfortably and effectively, helping to prevent complications such as discomfort or ill-fitting prostheses. By incorporating the tongue's natural movements into tray placement and adjustments, clinicians can significantly enhance the precision of the prosthetic process, ensuring a better overall outcome for the patient. Proper tray seating and careful adjustments not only improve the prosthetic fit but also promote patient comfort, making the procedure smoother and increasing patient compliance. This method of tray selection and fine-tuning is essential for achieving the desired results in prosthetic treatments while preventing discomfort and complications.7

Role of the Tongue in Border Molding for Denture Fabrication
Border molding is a crucial technique in the fabrication of dentures, ensuring that the borders of the impression tray are shaped to capture the precise contours and boundaries of the patient's oral tissues. The involvement of the tongue during this process is key to achieving an accurate and custom fit for the denture. For the anterior lingual flange, the patient is asked to move the lower lip from side to side with the tip of their tongue. This movement helps to establish the height of the anterior lingual flange while also recording the position of the lingual frenum. In the mylohyoid region, which extends from premolar to premolar, the patient is instructed to move their tongue to one side, touching the left cheek for the right flange molding and vice versa. This action helps determine the correct length and slope of the lingual flange in this area, ensuring that the denture contours to the mylohyoid muscle and avoids interference with its movement.8 For the retro mylohyoid portion, the patient is asked to open their mouth wide, protrude their tongue, and close their jaw against the operator's thumb resistance. This maneuver shapes the distal portion of the lingual flange, which rises towards the retromolar pad, providing guidance for its contour and extension towards this area. Additionally, to develop the thickness of the anterior lingual flange, the patient is asked to forcefully push their tongue against the front of the palate. This action shapes the flange thickness to ensure that the denture has adequate support and stability in the anterior region. The clinical importance of incorporating the tongue in border molding cannot be overstated. It ensures a custom fit by shaping the borders to match the patient's unique oral anatomy, while also allowing for muscle movements, such as those of the mylohyoid muscle, to be accommodated. This results in a denture that remains stable during function and maintains patient comfort. The final outcome of this process is a functional and well-fitting denture that enhances the patient's ability to speak, chew, and swallow, while minimizing discomfort. By involving the tongue in the molding process, clinicians can create dentures that are not only functional but also tailored to the patient's individual needs, significantly improving their quality of life.3,4,9
The Role of the Tongue in Occlusal Plane and Jaw Relation in Prosthodontics
The positioning of the occlusal plane plays a critical role in ensuring the stability and comfort of dentures, and the tongue’s position is integral to this process. The optimal position of the occlusal plane should align with or be slightly below the lateral border of the tongue. Placing the occlusal plane too high can result in instability of the denture due to lateral tilting forces exerted on the teeth. The correct positioning of the occlusal plane ensures that during function, forces are distributed evenly across the denture base, enhancing both stability and comfort for the patient. In the context of jaw relations, the tongue also plays a crucial role in various steps. For example, the mandibular wax rim is typically set at about two-thirds the height of the retromolar pad. The positioning of the occlusal plane, when aligned with the lateral border of the tongue, ensures proper stability and function of the denture. During vertical relation recording, the tongue should remain in its natural resting position to accurately capture the patient’s occlusal plane and vertical dimension. Additionally, when training the patient to close in centric relation, they may be instructed to touch their tongue to the palate and swallow. This action helps establish a stable, reproducible jaw position, which supports proper occlusion and the functional movement of the dentures. Thus, the tongue's involvement is key in achieving a functional, stable, and comfortable prosthetic fit.3,4,5
The Role of the Tongue in Teeth Arrangement and Denture Stability
The arrangement of teeth in dentures requires careful consideration of various anatomical and functional factors, with the tongue playing a pivotal role in guiding and stabilizing the prosthesis. One of the key landmarks for positioning the lingual cusps of the molars is the mylohyoid ridge. The lingual cusps should align harmoniously with this ridge and never be placed too lingually. If the cusps are placed too far lingually, it can lead to several complications, including tongue cramping, tongue biting, and instability of the denture during tongue movements, making the prosthesis uncomfortable and functionally inadequate. The neutral zone technique is another critical aspect that involves balancing the forces exerted by the tongue and the cheeks/lips. The teeth and denture flanges should be positioned within this neutral zone, where muscle forces are in equilibrium, thereby enhancing the stability and comfort of the denture. If the neutral zone is not properly accounted for, dentures can become unstable, failing to accommodate the natural neuromuscular function of the oral cavity. Achieving the ideal tooth position and flange contour is essential for creating dentures that align with the patient’s neuromuscular dynamics. When dentures are designed with consideration for these factors, they are more likely to remain stable during functional movements, such as speaking and chewing. This alignment enhances the overall comfort and functionality of the denture, contributing to higher patient satisfaction and improved quality of life. By incorporating the role of the tongue in the arrangement and positioning of teeth, prosthodontists can ensure that dentures function optimally and provide a comfortable, stable fit for the patient.5,10
The Role of the Tongue in Speech Considerations for Dentures
The tongue plays a critical role in speech, and its interaction with dentures is essential for clear articulation of various sounds. Linguo-dental sounds, such as "Th" (as in "this" or "that"), are produced when the tip of the tongue contacts the palatal surface of the upper anterior teeth. For clear articulation of these sounds, the positioning of the upper anterior teeth is vital. Similarly, linguopalatal sounds, like "D", "N", "L", and "T", are produced by the interaction between the tongue and the palate. The contour of the palate and the positioning of posterior teeth significantly influence the clarity of these sounds. Alveolar sounds, such as "D" and "T", are produced when the tongue contacts the anterior portion of the hard palate. Proper alignment of the anterior teeth and the contour of the palate are crucial for supporting the articulation of these sounds. Additionally, nasal sounds like "N" and "NG" can be impacted by the thickness of the denture base. Excessive thickness on the palatal surface reduces tongue space and air volume, making it difficult for the tongue to move freely and impeding clear articulation of linguopalatal and linguoalveolar sounds. Another critical consideration is the potential for tongue cramping, which can occur if the teeth are placed too lingually or if the arch is too narrow. This can interfere with the articulation of linguoalveolar and lateral lingual sounds, leading to mispronunciations and unclear speech. Misalignment of the teeth can also cause faulty phonation, affecting speech clarity and communication. Clinically, it is essential to manage the thickness of the denture base carefully to ensure sufficient tongue space and airflow for clear speech. Proper teeth positioning, with consideration for natural tongue movements, is crucial for effective articulation of various sounds. Dentures designed to support natural tongue function not only enhance speech clarity but also improve patient comfort and confidence in communication. A well-designed denture that accommodates the tongue’s role in speech will significantly improve the patient’s ability to speak clearly and comfortably.3,11
The Role of the Tongue in Polished Surface Contour and Food Trough Formation in Dentures
The position and function of the tongue are fundamental to the stability and performance of dentures. The tongue is one of the most powerful muscles in the mouth, exerting an impressive 16.4 pounds per square inch (Psi) of force—significantly more than the 4.3 Psi exerted by the lips and cheeks. This force directly impacts denture stability, particularly in the lingual surface contour. When contouring dentures, it is critical to account for the tongue's role to ensure that the denture remains stable during normal oral functions such as speaking and swallowing. Properly contoured lingual surfaces provide adequate support to resist disruptive forces from tongue movements, which could otherwise lead to instability or discomfort. The denture design must strike a balance, ensuring sufficient retention while also accommodating the natural forces exerted by the tongue. The tongue also plays a vital role in the initiation of jaw movements and food trough formation during mastication. Neuromuscular control, largely driven by the tongue, initiates the opening and closing of the mandible, ensuring that the teeth come together properly to break down food. This coordination is essential for chewing food into smaller particles that are more easily swallowed. During mastication, food particles may escape from the premolar region into the buccal or lingual spaces. The buccinator muscle helps retrieve food from the buccal space, while the tongue plays a key role in retrieving food from the lingual space, guiding the food back to the occlusal surfaces for further grinding. Additionally, the modiolus, an anatomical landmark located on the buccal surface of the lower first premolar, facilitates the movement of food during mastication. It helps direct the posterior movement of food along the cheek and tongue. Once the food has been sufficiently chewed, the tongue works in coordination with other oral muscles to form a cohesive bolus of food, preparing it for swallowing. Efficient mastication and bolus formation ensure that the food is properly prepared before being propelled toward the pharynx for swallowing, supporting the digestive process. In denture design, recognizing the tongue's involvement in both food manipulation and denture stability is essential for creating functional, comfortable, and effective prostheses.12
Bottom of Form
Advancements and Challenges in Tongue Prostheses and Rehabilitation
Tongue prostheses have become an essential tool in the rehabilitation of patients who have undergone glossectomy, particularly in enhancing speech and swallowing functions. Research has demonstrated that individuals receiving tongue prostheses experience substantial improvements in speech intelligibility and their ability to swallow, significantly boosting their quality of life. These prostheses, typically made from materials such as high-temperature vulcanizing silicone, offer excellent comfort and adaptability, making them ideal for long-term use. The material's flexibility and ease of adjustment ensure that the prosthesis can effectively mimic the natural movement of the tongue, which is crucial for speech and deglutition. However, despite these benefits, challenges in denture stability remain a concern, particularly because the tongue’s muscular activity can interfere with the retention and functionality of complete dentures. Understanding the dynamics of tongue movement is therefore essential for prosthodontists to design dentures that can effectively accommodate such movements, ensuring they remain stable during daily activities. Patients who have undergone partial glossectomy, in particular, face unique difficulties that require tailored prosthodontic solutions to restore their oral functions effectively. These patients often experience changes in tongue size and function, demanding customized approaches for prosthetic design. In addition to traditional prosthodontics, innovative approaches are emerging, such as tongue-based control systems for prosthetic limbs. This development highlights the potential to integrate tongue function not only in oral rehabilitation but also in broader prosthetic applications, thus extending the versatility of the tongue as a functional interface for various types of prosthetic devices. These advancements are reshaping the landscape of rehabilitation, offering patients enhanced control and improved quality of life across multiple domains of prosthetic care.13,14,15
CONCLUSION
Recent advancements in prosthodontics related to the tongue include digital scanning and CAD/CAM technology, which capture precise tongue dynamics to improve prosthesis design. 3D printing enables the customization of tongue prosthetics, particularly beneficial for post-resection patients. Biofeedback devices are helping train tongue movements in individuals with neuromuscular disorders or tongue thrust issues, improving functional outcomes. Additionally, tissue engineering holds promise for regenerative solutions to address tongue tissue loss, offering new avenues for rehabilitation and enhancing prosthetic success. The tongue is a dynamic and influential organ in prosthodontics, impacting prosthetic success and patient satisfaction. Understanding its anatomy, function, and interaction with prostheses is crucial for effective rehabilitation. Advances in technology and interdisciplinary approaches promise to overcome existing challenges, improving outcomes for patients with varied needs.
REFERENCES
- Srinivas K, Jyoti Gupta, Ratnakar P, Arti Saluja Sachdev, Vasu Saxena, Taseer Bashir. Anatomy of tongue - A review article International Journal of Multidisciplinary Research and Development. 2014; 1(7):124-125.
- Essentials of complete denture prosthodontics- Winkler, 3 RD Edition
- Dr. Divya Puri, Dr. Pankaj Dhawan and Dr. Piyush Tandan. International journal of applied dental sciences tongue and its prosthodontic implications. Int. J. Appl. Dent. Sci. 2020;6(2):362-366.
- Kumar, Prince; Khattar, Ashish1; Yadav, Suresh2; Kumar, Puneet3. Prosthodontic significance of tongue: An overview. SRM Journal of Research in Dental Sciences 3(3):p 224, Jul–Sep 2012. | DOI: 10.4103/0976-433X.107410
- Desjardins RP. The tongue as it relates to complete dentures. J Am Dent Assoc. 1974;88(4):814–822.
- Pankaj, Kharade., Kanchan, P., Dholam., Gurmit, K., Bachher. (2017). 1. Appraisal of Function After Rehabilitation With Tongue Prosthesis.. Journal of Craniofacial Surgery, doi: 10.1097/SCS.0000000000004008
- Bhupinder, Kaur., Gaurav, Gupta., Navreet, Sandhu., Sarabjeet, Singh, Sandhu., Gurpreet, Kaur., Tina, Gupta. (2014). 3. Tongue: the most disturbing element in mandibular denture: how to handle it?.
- Madhura, Govind, Titar., Pronob, Kumar, Sanyal., Shubha, Kamnoor., Sujit, Anil, Vyavahare. (2024). 2. Prosthodontic rehabilitation with functional palatal duplication prosthesis of completely edentulous patient with partial glossectomy.. Indian journal of applied research, doi: 10.36106/ijar/9504314
- Jasmina, Tabeen, Bhat., Narendra, Kumar., Kunwarjeet, Singh., Humaira, Tanvir. (2021). 8. Phonetics in prosthodontics: its clinical implications in designing of prosthesis. International Journal of Applied Dental Sciences, doi: 10.22271/ORAL.2021.V7.I2B.1193
- Rothman R. Phonetics consideration in denture prosthesis. J Prosthet Dent. 1961; 11:214?23
- Barnett Kessler. An analysis of the tongue factors and its functioning areas in dental prosthesis. 1955; 5(5):629-35.
- Beresin VE, Schiesser FJ. The neutral zone in complete dentures. J Prosthet Dent. 2006; 95(2):93-100.
- Phonetics and tongue position to improve mandibular denture retention. J Pros Dent. 2007; 98(5):344-7.
- Kydd WL. Maximum forces exerted on the dentition by the perioral and lingual musculature. J Am Dent Assoc. 1957; 55(5):646-51.
- Wright CR. Evaluation of the factors necessary to develop stability in mandibular dentures. J Prosthet Dent. 2004; 92(6):509-18.


 Dr. Vengateshwara*
Dr. Vengateshwara*
 Dr. Ponsekar Abraham A.
Dr. Ponsekar Abraham A.



 10.5281/zenodo.14584533
10.5281/zenodo.14584533