Abstract
Objective:
This review highlights the intricate relationship between asthma, anti-asthmatic drugs, and oral health. It serves as an essential resource for healthcare providers and patients alike, underlining the importance of educating asthma patients about potential oral health risks associated with long-term medication use and also about proactive measures to safeguard oral health while effectively managing asthma
Data Sources:
A bibliographic search of 27 scientific articles published between 2000 and 2023 was carried out in PubMed, ScienceDirect and Google Scholar.
Study Selection:
Those peer-reviewed, English-language studies that addressed the link between asthma and oral health were included.Studies that weren't pertinent to the study were omitted. Studies authored in languages outside English were disqualified. Studies that were unreliable or pointless were eliminated.
Result :
This review was performed to increase awareness among healthcare providers and asthmatic patients regarding the potential side effects of anti-asthmatics on oral health. Although corticosteroid and beta 2 agonists regimens are efficient, they deliberately cause adverse events if used for a longer time frame. Hence, the mechanism of steroids and beta 2 agonists damaging the oral health is unclear.
Conclusion: This review stresses the importance of the risk associated with anti-asthmatics usage and the need for proactive measures to maintain oral health during asthma treatment.
Keywords
Anti-Asthma, Oral Health, Corticosteroids, Oral candidiasis.
Introduction
Asthma is a widespread chronic lung disease affecting millions of individuals of all ages worldwide, characterized by symptoms such as wheezing, chest tightness, and shortness of breath1. In accordance with epidemiological data, there were 43.12 million instances of asthma reported in 2017, and there were 272.68 million illnesses and 0.49 million fatalities related to the condition overall. Over the past 25 years, both fatalities and disability-adjusted life years have reduced, but mortality has fallen significantly2. The management of asthma often involves the use of anti-asthmatic drugs, which can be broadly categorized into controllers (e.g., corticosteroids, LABA, leukotriene antagonists) and relievers (e.g., SABA). These medications aim to control acute attacks and prevent inflammation in the airways. They are commonly administered through inhalers or nebulizers, making direct contact with the oral cavity inevitable3 The use of anti-asthmatic drugs can have significant implications for oral health. Prolonged usage of these medications can lead to a range of oral issues, including dental caries, dental erosion, and oral candidiasis. These oral health concerns are often the result of factors such as reduced salivary flow (xerostomia) and alterations in oral pH caused by these drugs4. Saliva, a crucial component of oral health, plays a vital role in maintaining the integrity of oral tissues and defending against various oral diseases. However, anti-asthmatic drugs can disrupt this protective mechanism, leading to oral health problems. For instance, the use of inhalers can reduce salivary secretions, which, in turn, may promote the growth of Candida species, leading to oral candidiasis. Additionally, the decrease in salivary protection can make teeth more vulnerable to dental caries and erosion5. This review highlights the intricate relationship between asthma, anti-asthmatic drugs, and oral health. It serves as an essential resource for healthcare providers and patients alike, underlining the importance of educating asthma patients about potential oral health risks associated with long-term medication use and also about proactive measures to safeguard oral health while effectively managing asthma. In particular, the review focuses on the impact of corticosteroids, which are commonly used to manage asthma but require careful consideration due to potential adverse effects. In addition, to mitigate the impact of anti-asthmatic drugs on oral health, various strategies and countermeasures are discussed in this review. They include mouth rinsing after inhaler use, the use of spacers to reduce oral exposure to steroids, promoting salivary flow through methods like sugar-free gum or sialagogue medications, and the application of topical antifungal agents to prevent or manage oral candidiasis.
METHODS
The purpose of this research was to learn more about how anti-asthmatic medications affect dental health. A bibliographic search of 27 scientific articles published between 2000 and 2023 was carried out in PubMed, ScienceDirect and Google Scholar.
We used search strategy terms such as “ASTHMA”, “ASTHMA AND ORAL HEALTH”, “ASTHMA DRUG THERAPY”, “ASTHMA AND ORAL CANDIDIASIS”, “INHALERS AND ORAL DISEASE”, “CORTICOSTEROIDS; ORAL CANDIDIASIS”, “ORAL CANDIDIASIS”, “ANTI-ASTHMATICS AND ORAL HEALTH”, “ASTHMA; DENTISTRY”, “ASTHMA DRUG THERAPY”,
Inclusion criteria:
Those peer-reviewed, English-language studies that addressed the link between asthma and oral health were included. Exclusion criteria: Studies that weren't pertinent to the study were omitted. Studies authored in languages outside English were disqualified. Studies that were unreliable or pointless were eliminated.
RESULT AND DISCUSSION
Asthma and its treatment
Asthma is a chronic, noncommunicable lung disease caused by long-term inflammation in the trachea, bronchi, terminal bronchioles, and parenchyma, with the degree of inflammation influenced by airway hyper-responsiveness and not asthma severity2. Asthma phenotypes vary due to genetic predisposition, personal or family history of allergies, chewing tobacco, smoking, specific pollutants, trigger factors such as exercise, gastro-oesophageal reflux disease, sensitivities to the environment, aspirin use, plants and insects, chemical odours, obesity, stress, and respiratory tract infections. It results from inflammation, mucus production, and obstruction, leading to increased resistance and difficulty in treatment if not addressed3. Asthma treatment includes the use of various types of medications aimed at achieving two key
OBJECTIVES:
Acute Symptom Control:
During acute asthma attacks, the goal is to quickly open narrowed airways and alleviate breathing difficulties. This is typically accomplished using fast-acting reliever medications, such as SABA.
Chronic Management and Prevention:
For the long-term control of asthma, the focus is on reducing airway inflammation and resistance to maintain stable airflow. This involves prophylactic measures and medications to prevent exacerbations and minimize symptoms.
Asthma medications are categorised as follows:
1. Bronchodilators:
These drugs stimulate beta 2 receptors, leading to the relaxation of bronchial muscle cells, a decrease in the release of mediators, and bronchodilation. Examples include salbutamol, terbutaline, bambuterol, salmeterol, formoterol, and ephedrine.
They work by inhibiting phosphodiesterase (PDE), increasing cAMP production, resulting in bronchodilation, vasodilation, and cardiac stimulation. These drugs include theophylline, aminophylline, choline theophyllinate, hydroxyethyl theophylline, and doxophylline.
These bronchodilators block cholinergic constriction, primarily in large airways. Combining inhaled ipratropium with beta-2 agonists can produce more profound and longer-lasting bronchodilation. Drugs in this category include ipratropium bromide and tiotropium bromide.
- Leukotriene Antagonists:
These drugs are an alternative to inhaled corticosteroids and are used for mild to moderate asthma. They work by competitively antagonizing cysteinyl leukotrienes (cysLTs), reducing bronchoconstriction, increasing vasodilation, and recruiting eosinophils. Examples include montelukast and zafirlukast.
3. Mast Cell Stabilizers:
These medications are prescribed for long-term prophylaxis in mild to moderate bronchial asthma and allergic rhinitis. They work by inhibiting mast cell degranulation, restricting the release of mediators like histamine, leukotrienes, platelet-activating factor (PAF), and interleukins. Drugs in this category include sodium cromoglycate and ketotifen.
- Corticosteroids:
While corticosteroids do not cause immediate bronchodilation, they are essential for decreasing bronchial hyperactivity by suppressing the inflammatory response triggered by antigen-antibody reactions. They are available in two forms:
Examples include hydrocortisone and prednisolone.
Examples include beclomethasone, budesonide, fluticasone, and flunisolide.
- The choice of anti-asthmatic medications is determined by the severity and type of asthma. These medications, in combination with lifestyle adjustments and identifying and avoiding asthma triggers, form the basis of asthma management and prevention.
Table 1: Anti-Asthmatics And Their Effect On Oral Health
Oral health Vs Anti-Asthmatics
Saliva plays a major role in preserving and maintaining oral tissue hygiene. It is an exocrine secretion that contains 99% water with enzymes, immunoglobulins, proteins and other antimicrobial factors that protect dental health5. The functions of saliva include lubrication and maintenance of mucosal integrity, buffering capacity and re-mineralization and antimicrobial action that contribute to preserving oral health. Salivary flow and composition possess a defensive mechanism that is impaired in asthmatic conditions, as anti-asthmatic agents can slow down the above mechanism by decreasing salivary secretions (xerostomia), which is due to the long-term usage of beta-2 agonists. Acid pH is lowered in the oral cavity due to inhalers6.Major mechanisms of anti- asthmatics include bronchodilation and anti-inflammatory actions by which airway obstructions are cleared, making breathing easier. Nevertheless, most anti- asthmatic are adhered to inhalers or nebulizers containing corticosteroids, and contact with the oral mucosa cannot be avoided, which increases the risk of oral health problems7.
Some of the most common diseases that are caused by the impact of anti-asthmatic agents include the following:
- Oral Candidiasis
- Dental erosion
- Dental caries
ORAL CANDIDIASIS:
It is a spontaneous infection of the oral mucosa caused by an over-abundance of Candida species, particularly Candida albicans. White patches on the tongue, oropharynx, hard and soft palates, labial, lingual and buccal mucosa serve as telltale signs. The prevalence of oral candidiasis is typical in asthmatic patients who are under a long-term regimen consisting of inhalers or nebulizers containing corticosteroids 2,8,9,10.In contrast to the debris remained in the oral mucosa, which is typically brought on in patients who receive a high dose of ICS, it is triggered by the topical effects of inhaled corticosteroids on the oral mucosa, where only 20% of drugs enter the lungs2,6,8,10,11. Some studies imply that individuals who use ICS have a higher incidence of candidiasis owing to the immunosuppressive and anti-inflammatory properties effects of the treatment. Long-term administration of beta-2 agonists may decrease salivary flow rate,Increased salivary glucose levels, decreased oral pH, and diminished buffering capacity can all promote the proliferation of candida species on the oral mucosa2,8,10,11,12. Few studies showed that the dry powder inhalers' lactose monohydrate constituent can also increase salivary glucose levels6,8,10,11. The above mentioned mechanisms can make the oral mucosa more vulnerable to Candida growth. Fukushima et al13 studied the adverse effects between inhaled fluticasone propionate and beclomethasone dipropionate and found that the anti-inflammatory effects of fluticasone propionate are twice the effect of beclomethasone; they also stated that inhaled fluticasone dose-dependently decreases local immunity, thereby concluding that the growth of candida increases with increasing doses of fluticasone. Some studies have reported that asthma causes oral health; mild to moderate asthma causes a reduction in salivary flow, causing mucosal changes in accordance with chronic mouth breathing11. Tahir F et al8 concluded that asthma strongly affects oral health and causes xerostamia due to the use of inhalers, a decrease in saliva secretion, and chronic mouth breathing; beta-2 agonists, as anti-asthmatic agents, play a important role in the salivary flow rate by reducing Parotid saliva increased by 36% and entire saliva by 26%.Katarzyna Macikowska et al14. stated that glucocorticoid therapy for a prolonged period of time has a negative effect on the immune system and salivary secretion. Ashuja RB et al12 conducted a study to assess the baseline microbial count in asthmatic subjects and controls in the third and sixth months following the start of inhaler therapy. They found that candidal pathogenicity is dependent on their capacity for adhesion on the oropharyngeal surface to form pseudohyphae and to secrete histolytic enzymes, and they came to the conclusion that there is a higher incidence of Candida growth in the case than in the control. Abidullah et al15 found that the growth of Candida species in asthmatic individuals is very high. Anti-asthmatic agents affect the oral environment, making it prone to opportunistic infection. Canida proliferate when the neutrophils are dropped, as they are the first line in the defense kills until 40% of candida growth is diminished with the myeloperoxidase hydrogen halide system due to the immunosuppression of corticosteroids in the anti-asthmatic medications. A study was carried out to determine the relationship between asthma subjects and oral candida invasion. The CFU/ml of Candida albicans in saliva was determined in controls, and 64% growth of Candida albicans was found in asthmatic subjects, and in 36% of patients, there was no development of Candida albicans, implying that anti-asthmatic patients have microfloral changes that support candida growth. Asthma patients are prone to candida infection based on disease severity and drug dosage, and it is feasible that asthma patients are more vulnerable to candida growth.
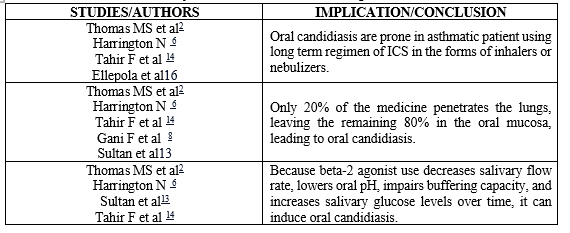
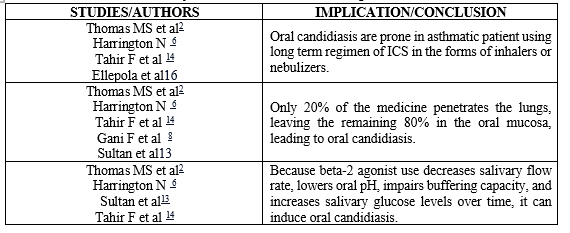
Table 2: Summary of the studies and their implication/ Conclusion
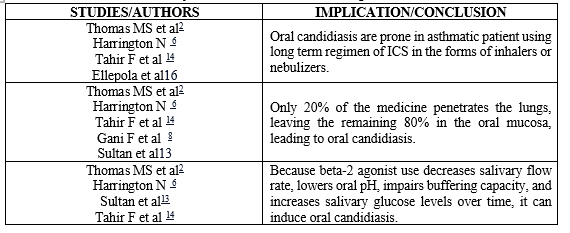
The table 2 depicts a summary of the above mentioned details.
DENTAL CARIES:
Dental caries is a long-term disorder in which oral bacteria convert sugar into acid, harming teeth and causing further tooth structure loss. If left untreated, inter-proximal caries, as is known, will develop. More than 35% of the population suffers from dental caries according to the global burden of disease. According to a recent study, asthma patients have caries two percent more frequently than healthy people do. Although the exact origin of this is unknown, studies using the random effect model suggest that asthma patients had a 1.5 times higher probability of developing the condition than average people, with primary and permanent dentitions being the most severely affected16. More thorough research is being done, and parameters such as pH, salivary flow, and composition are being examined in the mouth. These findings clearly link asthma medications, asthma conditions, and a higher risk of dental caries17.

Figure 1: Prolonged use of beta 2 agonist and dry powder inhaler18
Streptococcus, Neisseria, Veillonella, Prevotella, Haemophilus, Kingella, and Porphyromonas are the microorganisms that are most frequently involved in dental caries. Asthma and tooth cavities are linked to these organisms.The most common of these is Veillonella, which was initially connected to the causes of tooth cavities and asthma in children. Boskabady Marzie et al , stated the severity of tooth decay in asthma patients using inhaled medications demonstrated that asthma patients' DMFT scores are greater indicating tooth decay.In addition to the oral-induced characteristics, the severity of the condition and the use of inhaled drugs, including their type, dosage, and frequency, can greatly influence19. Similarly in another study, greater DFS in children with regular dental care may be related to asthma-related physiologic changes20.
DENTAL EROSION:
Dental erosion is non-carious destructive multifactorial condition with a complex aetiology (pH <5>
PROACTIVE MEASURES
- Fukushima et al. changed the gargle solution from water to amphotericin B solution (1:50 dilution) in 27 patients with asthma who were tested for candida for 1 month of treatment. The results found to be favorable, as 22 of 27 patients with candida showed values below the minimum detection limit, and the minimum inhibitory concentration was found to be 0.16 ?L/mL in 22 patients in comparison to 0.14 ?L/mL in 5 patients13. Mouth rinsing after every use of ICS is recommended. Rinsing with amphotericin B diluted 1:5 is proven to be better than just gargling with water2,6,26,27.
- Usage of spacers with inhalers decreases the effect of steroids as the deposition of drugs in the oral mucosa is reduced2,11.
- To increase the salivary flow rate, sugar-free gums and sialagogue medications can be used2,10,11.
- Nystatin, a topical antimycotic, should be used until the end of steroid therapy, as it can damage the oral mucosa and avoid the recurrence of symptoms2,10,11,15,27.
- The dental practitioners recommended for asthmatic patients are as follows25:
- Frequent dental visits
- Education on asthma and its impact on oral health.
- Rinsing with mouthwash with neutral pH, sodium bicarbonate/sodium fluoride containing solutions.
- Measuring bone mineral density for ICS
CONCLUSION
This review was performed to increase awareness among healthcare providers and asthmatic patients regarding the potential side effects of anti-asthmatics on oral health. Although corticosteroid and beta 2 agonists regimens are efficient, they deliberately cause adverse events if used for a longer time frame. Hence, the mechanism of steroids and beta 2 agonists damaging the oral health is unclear. Hence, it is not evident that these drugs cannot be the only reason for the damage in oral health. Thus we stress the importance of the risk associated with these drugs usage and the need for proactive measures to maintain oral health during asthma treatment.
REFERENCE:
- https://www.ncbi.nlm.nih.gov/books/NBK279519/#_ncbi_dlg_citbx_NBK279519
- Barnes, P. J., & Drazen, J. M. (2002). Pathophysiology of asthma. Asthma and COPD, 343-359.
- Sinyor, B., & Perez, L. C. (2022). Pathophysiology of asthma. In StatPearls [Internet]. StatPearls Publishing.
- Thomas, M. S., Parolia, A., Kundabala, M., & Vikram, M. (2010). Asthma and oral health: a review. Australian Dental Journal, 55(2), 128-133.
- Pacheco-Quito, E. M., Jaramillo, J., Sarmiento-Ordoñez, J., & Cuenca-León, K. (2023). Drugs Prescribed for Asthma and Their Adverse Effects on Dental Health. Dentistry journal, 11(5), 113. https://doi.org/10.3390/dj11050113
- Gani, F., Caminati, M., Bellavia, F., Baroso, A., Faccioni, P., Pancera, P., ... & Senna, G. (2020). Oral health in asthmatic patients: a review: Asthma and its therapy may impact on oral health. Clinical and Molecular Allergy, 18, 1-8.
- Pacheco-Quito, E. M., Jaramillo, J., Sarmiento-Ordoñez, J., & Cuenca-León, K. (2023). Drugs Prescribed for Asthma and Their Adverse Effects on Dental Health. Dentistry Journal, 11(5), 113.
- Tahir, F., & Hafeez, F. (2018). Oral health in asthmatics: a review. J Dent Oral Care Med, 4(1), 102.
- Ellepola, A. N. B., & Samaranayake, L. P. (2001). Inhalational and topical steroids, and oral candidosis: a mini review. Oral diseases, 7(4), 211-216.
- Harrington, N., Prado, N., & Barry, S. (2016). Dental treatment in children with asthma–a review. British dental journal, 220(6), 299-302.
- Kele?, S., & Yilmaz, N. A. (2016). Asthma and its impacts on oral health. Meandros Medical And Dental Journal, 17(1), 35-38.
- Ashuja, R. B., Nandini, D. B., Vidyasagar, B., Ashwini, R., Donoghue, M., & Madhushankari, G. S. (2018). Oral carriage of cariogenic bacteria and Candida albicans in asthmatic adults before and after anti-asthma medication: A longitudinal study. Journal of oral and maxillofacial pathology: JOMFP, 22(1), 144.
- Fukushima, C., Matsuse, H., Tomari, S., Obase, Y., Miyazaki, Y., Shimoda, T., & Kohno, S. (2003). Oral candidiasis associated with inhaled corticosteroid use: comparison of fluticasone and beclomethasone. Annals of Allergy, Asthma & Immunology, 90(6), 646-651.
- Macikowska, K., Paruzel-Pliskowska, A., Curlej-W?drzyk, A., Ka?u?a, P., & Pytko-Polo?czyk, J. (2021). The condition of the oral cavity in patients receiving chronic steroid therapy-practical remarks. Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego, 49(293), 382-384.
- Abidullah, M., Sanober, A., Kumar, S., Gaddikeri, K., Soorneedi, N., Fatema, R., & Ahmed, S. M. (2022). Salivary Candida albicans in asthmatic patients taking anti-asthmatic medication. Journal of Medicine and Life, 15(9), 1110-1114.
- Bernardo Antonio Agostini, Kaue Farias Collares, Francine dos Santos Costa, Marcos Britto Correa & Flavio Fernando Demarco (2019) The role of asthma in caries occurrence – meta-analysis and meta-regression, Journal of Asthma, 56:8, 841-852, DOI: 10.1080/02770903.2018.1493602.
- Alavaikko, S., Jaakkola, M. S., Tjäderhane, L., & Jaakkola, J. J. (2011). Asthma and caries: a systematic review and meta-analysis. American journal of epidemiology, 174(6), 631–641. https://doi.org/10.1093/aje/kwr129.
- Mehta A, Sequeira PS, Sahoo RM.(2009) Bronchial Asthma and Dental Caries Risk: Results from a Case Control Study. The Journal of Contemporary Dental Practice, Volume 10, 059-066.
- Boskabady Marzie, Nematollahi Hossein, and Boskabady Mohammed Hossein (2012) Effect of Inhaled Medication and Inhalation Technique on Dental Caries in Asthmatic Patients. Iran Red Cres Med J. 816-21. DOI: 10.5812/ircmj.4658
- Shulman, J. D., Taylor, S. E., & Nunn, M. E. (2001). The association between asthma and dental caries in children and adolescents: A population-based case?control study. Caries research, 35(4), 240–246. https://doi.org/10.1159/000047464.
- Imfeld, T. (1996). Dental erosion. Definition, classification and links. European journal of oral sciences, 104(2), 151-155.
- Lussi, A., Schlüter, N., Rakhmatullina, E., & Ganss, C. (2011). Dental erosion–an overview with emphasis on chemical and histopathological aspects. Caries research, 45(Suppl. 1), 2-12.
- Al?Dlaigan, Y. H., Shaw, L., & Smith, A. J. (2002). Is there a relationship between asthma and dental erosion? A case control study. International Journal of Pediatric Dentistry, 12(3), 189-200.
- O'Sullivan, E. A., & Curzon, M. E. (1998). Drug treatments for asthma may cause erosive tooth damage. Bmj, 317(7161), 820.
- Farag, Z. H. A., & Awooda, E. M. (2016). Dental erosion and dentin hypersensitivity among adult asthmatics and non asthmatics hospital-based: a preliminary study. The open dentistry journal, 10, 587.
- Akpan, A., & Morgan, R. (2002). Oral candidiasis. Postgraduate medical journal, 78(922), 455-459.
- Buhl, R. (2006). Local oropharyngeal side effects of inhaled corticosteroids in patients with asthma. Allergy, 61(5), 518-526.


 Rama Parthasarathy*
Rama Parthasarathy*
 Sona Primuha S.
Sona Primuha S.

 10.5281/zenodo.12617362
10.5281/zenodo.12617362