Several types of oral health issues can affect pregnant women and have a negative impact on both of their personal health and the health of their unborn child. There are a lot of misconceptions regarding the safety of dental care. Pregnant women therefore receive less dental treatment than non-pregnant women. In this study, we focused on the oral health, common dental issues, clinical management strategies and treatment approaches of pregnant women
Effective and sufficient treatment is necessary to maintain the dental and oral health in one's life. Dental care is even more crucial for women during their menopausal, nursing, and child-bearing years. Being pregnant is an indication of health rather than a sickness state. It is not typical for a healthy person to lose their teeth for no apparent cause. Pregnant women also are subjected to the same conditions. They won't have tooth loss or other dental issues if they follow a few easy measures. However, dental decay and gingival issues are known to affect mothers when they are pregnant. Pregnant women who have poor oral health may face the following conditions: loose teeth, mouth dryness, pre-eclampsia, pregnancy granuloma, gingivitis, low birth weight babies, early delivery, and tooth erosions. Pregnancy-related hormonal changes have a direct impact on gum disease and a secondary impact on tooth decay (1 - 6).
Changes seen in the gums
Women who are pregnant have changes in their hormonal balance. Because the placenta generates more oestrogen and progesterone during pregnancy; several tissues experience specific modifications. The gingiva becomes more sensitive to irritations at this time. Pregnancy tumours, often referred to as gingivitis or epulis gravidarum, are frequently observed throughout pregnancy. Pregnancy gingivitis often begins in the second month of gestation, peaks in the eighth month, and resolves on its own following delivery. They come from pyogenic granulomas and go away in one to two months. If they do not go away on their own, surgery is advised. Excision surgery can be carried out using a laser or with traditional techniques. Pyogenic granulomas have a tendency to bleeding; therefore laser therapy may provide the patient with more pleasant outcomes. In actuality, therapy during pregnancy is not necessary if they do not bother the patient or bleed excessively. According to Silk et al, gingivitis was discovered in 40 % of pregnancies (3 - 7). However, others contend that pregnancy has little effect on healthy gingiva and that gingivitis is only a response brought on by increasing plaque (8). The gum papillae may seem red or similar to a strawberry like colour that has expanded. Fissures may develop on the papillae and the gingival margins. There have been reports of discomfort and bleeding. The gingiva of those with hyperplastic characteristics is dull, pale pink, with a rough, dry surface. The gums may occasionally have a deep crimson tint. Pregnancy tumours may appear when gingiva growth is restricted to a single location. Usually, an irritation is the root cause. Pregnancy tumour, gingivitis simplex, gingivitis ulcerosa, and gingivitis hypertrophicans are the names given to these alterations in the gingiva. It has been demonstrated that the increased blood level of progesterone, which raises vascular permeability, is the source of these alterations. Low vitamin C levels are considered to be another cause of this condition (9). It is believed to be advantageous to provide vitamin C, Phosphate and Calcium (10, 11). Mothers who have attachment loss have a higher risk of giving birth to low birth weight babies (small for gestational age) when compared with mothers with healthy periodontiums (12 - 16). Many systemic disorders, including those connected to pregnancy, are linked to periodontal diseases.
Changes seen in the teeth
Pregnancy is known to increase the risk of tooth decay. There is visible tooth loss and discomfort in the teeth. The idea that every pregnancy results in tooth loss and that the foetal supply of calcium needed for intrauterine growth comes from the mother's teeth is unfounded in science. Dentists have the following explanation for this phenomenon: in 70% of pregnancies, nausea and vomiting are experienced. Vomiting can have a detrimental impact on dental hygiene or erode the layer of enamel in mothers. The concentration of Calcium decreases during pregnancy. However bone turnover doubles during pregnancy, there is no change in the quantity of ionised calcium when compared to pre-pregnancy levels. Preventing this issue during pregnancy can be achieved by improving dental hygiene practices.
The following variables determine how oral and dental health deteriorates during pregnancy:
- Some mothers may experience intense cravings for certain foods particularly carbs, during the first few months of their pregnancy, and most of the time they forget to wash their teeth afterward.
- Because of the effects of pregnancy hormones (progesterone and oestrogen), pregnant women may refrain from cleaning their teeth. As a result, bacterial plaque increases.
- Vomiting causes the mouth's acidity to rise, particularly in the early months of pregnancy. In the initial months following vomiting, the mother might not give enough attention about oral hygiene. Inadequate tooth brushing might lead to the formation of an acidic oral environment.
- There is a reduction in saliva flow. These factors contribute the caries development at this time.
These factors make it essential to focus more on oral health care throughout this time (1 - 9).
Importance of nutrition on dental health during pregnancy
A mother's and her child's health is positively impacted by a sufficient intake of nutrients, while an inadequate intake has the opposite effect. The mother's bones need to be strong throughout this time, thus she has to take 1200–1500 mg of calcium per day. Pregnant women should consume foods high in calcium, such as milk and dairy products, as well as green, leafy vegetables, to satisfy their calcium needs. There won't be any distinct dental issues during pregnancy if the women maintain a healthy diet and receive enough dental treatment. Pregnancy-related nutrition is crucial for the mother's overall health as well as the baby's dental health. The fifth and sixth weeks of pregnancy are when the baby's teeth begin to erupt. The goal of the nutrients consumed during pregnancy is to maintain the body's nutritional balance and to provide the foetus the energy and resources it needs to grow normally. Pregnancy has been demonstrated to elevate the Calcium and Magnesium levels in the molar teeth, whereas there is no change in Zn value. The rise in Calcium is assumed to be caused by rising levels of insulin-like growth factor-1 and placental lactogen during pregnancy (17).
These are the basic dietary recommendations for maintaining good oral and dental health during the entire pregnancy -
- Fruits, vegetables, cereal, milk, dairy products, meat, fish and eggs that are rich for A, C, D vitamins, calcium and phosphorus must be taken in a balanced diet.
- Sugar need to be stayed away from as much as possible, particularly in between meals.
- Toffees and dried fruit should be avoided.
- The mother's health and the health of the unborn child are both impacted by nutrition during this time. It is well known how vitamins A and D affect the development of enamel. Use of fluoride during pregnancy does not appear to be a reliable way to stop tooth decay (18).
Nicotine and alcohol consumption during pregnancy
Smoking is bad for teeth, especially the gums. Patients who smoke have higher rates of periodontal inflammation and damage. It becomes more difficult to maintain dental hygiene when there are more filiform and fungiform papillae on the tongue's surface, resulting in what is known as a "smooth tongue." Owing to smoking's anaemic effects, oral wounds may heal slowly and exhibit spontaneous bleeding (16). Changes in the mother's dental health have an indirect impact on the infant as well. Cigarette smoke contains around 4000 different chemicals. Among these are acids, aldehydes, ketones, cyanide, and carbon monoxide, all of which have immediate harmful consequences. It is well known that carbon monoxide, which makes up 4% of cigarette smoke, blocks oxygen from being transported by attaching itself to haemoglobin in red blood cells. Smokers' hemoglobin's ability to carry oxygen is decreased by 2.5% from 15%. As a result, the fetus's oxygenation level drops. Smokers have a higher risk of abortion. Additionally, the baby's birth weight is lower than average when they are delivered alive. Babies of smoker mothers are far more likely to die as newborns, either early or late (19, 20). Alcohol use can alter these receptors, which can result in dental abnormalities. Few researches reported that tiny teeth, structural enamel degradation, and delayed tooth rupture were observed in young rats when pregnant rats were administered alcohol at certain dosages. Indirect effects on the baby's condition may result from it, as well as hepatic and dental diseases in the mother (3, 21–23). Foetal hepatic syndrome can result from excessive alcohol use, which is teratogenic to unborn children. Dentists differentiate and proliferate because of epithelial growth factor receptors.
Guidelines for oral health during pregnancy
When it comes to enhancing dental health during pregnancy, getting both professional and personal care is crucial. Preventive maintenance practices carried out during pregnancy have been linked to plaque buildup and caries prevalence, according to Zanata et al (24, 25).
- Dental and oral hygiene should be maintained regularly.
- Given the clear correlation between hormonal changes during pregnancy and the development of gingival diseases and plaque accumulation, a comprehensive dental examination must be performed before to conception in order to achieve optimal oral hygiene and establish the habit of maintaining it. Pregnancy-related hormone increases the oral mucosa's sensitivity to outside stimuli, particularly when it comes to bacterial plaques.
- Using dental floss and using toothbrushes at least twice a day is recommended for effective dental care.
- Mouthwashes or warm, salted water gargling is required. Gum sensitivity is decreased and gums are relaxed by warm, salty water.
Treatment options and Management Strategies during pregnancy
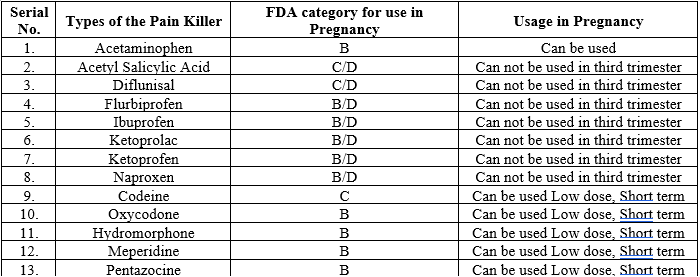
Many dentists believe they may conduct simple procedures on pregnant patients provided they get the doctor's clearance. Nonetheless, considering the strains that both the mother and the infant will experience, the majority of dental operations are crucial during the first and last three months of pregnancy. It is best to avoid receiving dental care during the first trimester. Since this is the stage of organogenesis, it is a very delicate time. Misuse of medical intervention can result in abortions. Nonetheless, immediate dental care is required if there is discomfort or if waiting would just make the situation worse. In some cases, dental extractions and root canal therapy are feasible. The second trimester is the most appropriate period for making many treatments, for those that if postponed until the end of pregnancy would be dangerous, such as tooth extraction, filling, and canal treatment. It is difficult for the mother to adopt the proper postures for dental treatment during the third trimester, and she may experience discomfort. The baby is almost ready to be delivered, having grown significantly in the womb. Additionally, keep in mind that a pregnant woman may develop vena cava inferior syndrome (also known as supine hypotensive syndrome) if she spends an excessive amount of time sitting in a dental chair during the last trimester. To alleviate the venous circulation in this case, turn the mother to the left in a semi-sloped position (1, 26). Similar to the first trimester, dental intervention is not advised unless it is absolutely necessary for urgent care. Many dental procedures, including extractions, local anaesthetics, root canal therapy, scaling, and root planing, can be carried out safely during pregnancy, despite the reluctance of some expectant mothers to undergo prenatal oral care (4, 5). Existing infections can have a far greater detrimental impact on the baby's health in emergency situations like tooth and gingival inflammation than can the negative consequences of dental treatment. As a result, dental care must be given in accordance with obstetrician recommendations. The quantity of ionised radiation in a single radiograph can be decreased by lead gowns, quick films, accurately calibrated instruments, and a collimator, all of which won't harm the developing foetus, in order to determine the operations to be carried out. According to the National Radiation Protection Committee, cumulative radiation exposure shouldn't be greater than 0.20 Gy since higher levels might result in mental impairment and microcephaly (27–30). Pregnancy-related congenital abnormalities and abortion have been linked to nitrous oxide anaesthesia (27, 31). When using local anaesthetics during pregnancy for any kind of operation, including tooth extraction, it is important to follow the manufacturer's instructions. There won't be any inconvenience if there is no specific notification. According to Food and Drug Administration (FDA) recommendations, pregnant women can safely utilise local anaesthetics such as lidocaine and prilocain (1, 30). Mercury gases generated during dental procedures should be avoided to prevent the patient or dental staff from breathing in stronger mercury fumes, even if they are not expected to have teratogenic consequences. Furthermore, it has been proposed that exposure to mercury at levels ? 1 ?g/day before to pregnancy is linked to attention deficit or hyperactivity disorder in young children (32, 33). Two dental examinations in the first trimester and one each in the second and third are the optimal numbers. Following a positive assessment at the initial check-up, it is important to determine whether oral hygiene is being supplied in the second trimester and whether the scheduled procedure (such as a filling or tooth extraction) is being carried out at this time. Penicillin, erythromycin, and cephalosporins are safe antibiotics to use during pregnancy when prescribed. However, using tetracycline (which changes the colours of teeth), vancomycin (which is ototoxic & nephrotoxic), and streptomycin (which is ototoxic) when pregnant might have negative consequences. The American Dental Association further states that barbiturates, benzodiazepines, and ciprofloxacin should be completely avoided. It is advised to take prenatal vitamin supplements. Teeth pain can be a contributing factor to the onset of contractions since it puts the patient under stress. As a result, consulting before prescribing painkillers is advised. Because non-steroidal anti-inflammatory medicines (NSAIDs) can result in patent ductus arteriosus (PDA) and narcotic analgesics also can depress the central nervous system, it is best to avoid using them while pregnant. It is preferable to use paracetamol throughout pregnancy. According to Food and Drug Administration (FDA) guidelines, the following list of painkillers is appropriate for use during pregnancy (Table 1) (32, 33):


 Priyanka Tanwar* 1
Priyanka Tanwar* 1
 Mamta Naagar 2
Mamta Naagar 2
 10.5281/zenodo.13732558
10.5281/zenodo.13732558