Abstract
Hemorrhoids, prevalent in the adult population, present a significant challenge in clinical management due to their symptomatic burden and impact on quality of life. This review delves into the current medical treatments available for hemorrhoid management, emphasizing the efficacy and safety profiles of various pharmacological agents. Treatments range from over-the-counter remedies such as topical anesthetics and corticosteroids to prescription medications like flavonoids and vasoactive compounds. The review critically assesses the therapeutic benefits and potential adverse effects associated with these medications, aiming to provide a comprehensive guide for clinicians in tailoring patient-specific treatment plans. In addition to pharmacotherapy, the review explores the role of emerging treatments in the medical management of hemorrhoids. It highlights novel approaches, such as topical nitroglycerin and calcium channel blockers, which offer promising outcomes in symptom relief and reduction of hemorrhoidal tissue. Furthermore, the review considers the integration of lifestyle modifications and complementary therapies, underscoring the importance of a holistic approach in managing this multifaceted condition. By examining the latest evidence-based practices, this review aims to enhance the understanding and optimization of hemorrhoid management strategies in clinical practice.
Keywords
Hemorrhoids, symptoms, Diet planning, Incidence in pregnancy, Ayurvedic treatment.
Introduction
The first mention of hemorrhoids is from a 1700 BC Egyptian papyrus, advising an ointment with acacia leaves for quick recovery. In 460 BC, the Hippocratic corpus describes a treatment similar to modern rubber band ligation, suggesting to hemorrhoids with thick woollen thread until they drop off. Hemorrhoids might also be referred to in the Bible, using the term "emerods".
Hemorrhoids are a common anorectal condition characterized by the enlargement and displacement of the anal cushions. They affect millions globally, posing significant medical and socioeconomic challenges. Several factors, including constipation and prolonged straining, contribute to their development. Key findings of hemorrhoidal disease include the abnormal dilatation and distortion of the vascular channels, and damage to the supporting connective tissue within the anal cushion. Inflammatory reactions and vascular hyperplasia are also often observed. This article reviews the pathophysiology and clinical aspects of hemorrhoidal disease, along with current non-operative and operative management approaches. Hemorrhoid disease is a prevalent condition in the anal region, seen in all ages and genders. It affects 50-85% of individuals worldwide, with peak prevalence between 45-65 years. Hemorrhoids significantly impact quality of life, presenting symptoms such as bleeding during or after defecation, pain, discomfort, prolapse, and perianal itching.
Symptoms and Classification:
- First-degree: Visible vessels, no prolapse.
- Second-degree: Prolapse with defecation, retracts on its own.
- Third-degree: Prolapse, requiring manual replacement.
- Fourth-degree: Prolapsed, cannot be replaced.
Treatment Approaches:
- Low Grades: Managed conservatively with lifestyle modifications, fiber supplements, anti-inflammatory suppositories, and venotonic drugs.
- Higher Grades: Treated with non-surgical approaches like sclerotherapy, rubber band ligation, laser therapy, and surgical methods like hemorrhoidectomy and stapled hemorrhoidopexy.
Surgical Considerations:
- Surgical treatments are reserved for advanced cases or when non-surgical methods fail.
Postoperative complications may include pain, urinary retention, and a shift towards non-surgical techniques is observed.
Types &Classification Of Piles
- Types:
- Internal Piles:
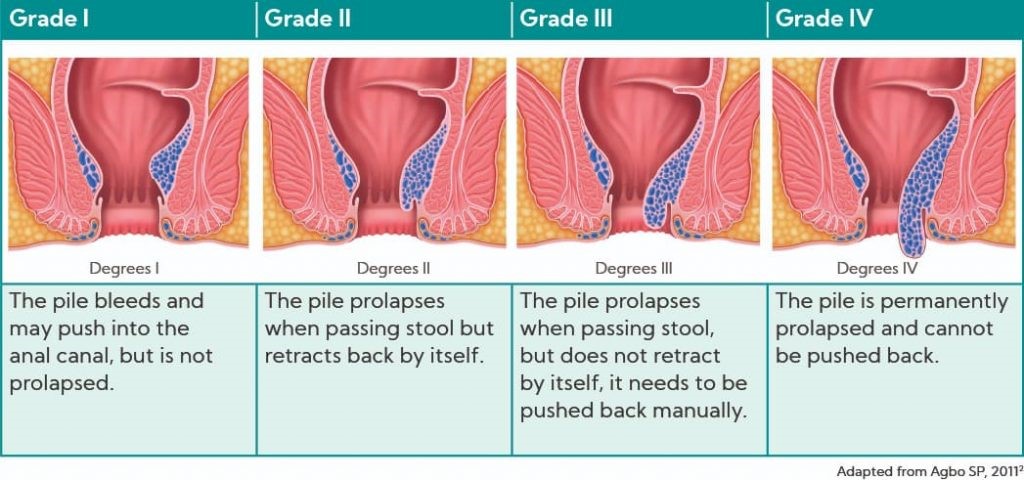
- Grade I: Bleed without prolapsing.
- Grade II: Prolapse during bowel movements but retract on their own.
- Grade III: Prolapse during bowel movements and need to be manually pushed back.
- Grade IV: Always prolapsed and cannot be pushed back.
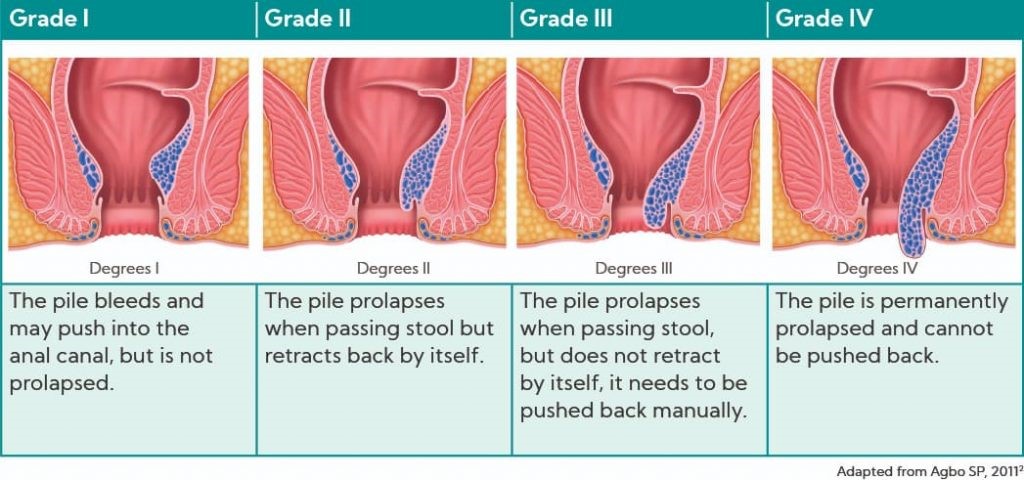
Figure 1: Grades of Piles
- Symptoms of Internal Piles:
- Blood in stools or on toilet paper.
- Fullness or pain in the rectum.
- Prolapse during bowel movements (Grades II-IV).
- Painless rectal bleeding.
- External piles
- Forms around the anus and are visible externally.
- They can be very painful, causing swelling, itching, and discomfort
- Symptoms of External Piles:
- A visible lump or swelling around the anus
- Pain or discomfort, especially when sitting or during bowel movements
- Itching or irritation in the anal area
- Thrombosed Piles:
- Thrombosed piles occur when blood clots form in external piles, causing intense pain,
swelling, and inflammation.
- Immediate medical attention is crucial, as drainage or surgery might be needed.
- Symptoms of Thrombosed Piles:
- A Sudden, severe pain and swelling around the anus
- A hard bulge at the anal opening
- Possible bleeding if the clot breaks
- Mixed Piles:
- Mixed piles consist of both internal and external hemorrhoids, leading to a complex combination of symptoms that might require specialized treatment.
- Indicators of both internal and external piles
- Consultation with a healthcare professional is essential for diagnosis and treatment planning
- Prolapsed Piles:
- Prolapsed piles occur when internal hemorrhs swell and extend outside the anus during bowel movements. This can be quite distress and often requires medical attention.
- Symptoms of Prolapsed Piles:
- A mass protruding during or after a bowel movement
- Difficulty pushing the prolapsed pile back inside
- Discomfort and pain when the hemorrhoid is outside the anus.
- Causes:
- Low-fiber diet and constipation
- Prolonged straining during defecation
- Diarrhea
- Hereditary predisposition
- Pregnancy
- Occupation
- Sports
- Leisure activities
- Hemorrhoids are believed to result from various conditions that increase intra-abdominal pressure or exacerbate hemorrhoid symptoms. These conditions include pregnancy, persistent cough, abdominal obesity, constipation, straining, vigorous activity, and weightlifting.
- Classification
- Goligher’s Classification:
- Grade I: Hemorrhoids that bleed but do not prolapse.
- Grade II: Hemorrhoids that prolapse when straining but retract on their own.
- Grade III: Hemorrhoids that prolapse and need to be manually repositioned.
- Grade IV: Hemorrhoids that are always prolapsed and cannot be pushed back.
- Classification Based on Relation to the Dentate Line:
- Internal Hemorrhoids: Covered by mucosa and originate above the dentate line.
- External Hemorrhoids: Arise below the dentate line and are covered by anoderm.
- Mixed Hemorrhoids: Arise both above and below the dentate line.
- Classification Based on Anatomical Locations:
- Primary Hemorrhoids: Occur at the three primary positions of the anal cushions.
- Secondary Hemorrhoids: Arise between the primary anal cushions.
- Circumferential Hemorrhoids: Encircle the anal opening.
- Classification Based on Symptoms:
- Prolapsing Hemorrhoids
- Non-Prolapsing Hemorrhoids
- Further Categorization of Goligher Grade:
- Each primary Goligher grade (I to IV) is further classified with suffixes based on te number of hemorrhoids and the presence of circumferential hemorrhoids or thrombosis:
- Single pile mass
- Two piles but covering less than 50% of the anal canal circumference
- Circumferential piles covering more than 50% of the anal canal circumference
- Thrombosed or gangrenous piles (complicated)
- Symptoms of Hemorrhoids
Bleeding:
- Fresh red blood during or after defecation
- Long-term bleeding can lead to a drop in hemoglobin levels
- Dark red blood with stool may indicate colonic disease
- Tarlike dark blood suggests bleeding from the upper GI tract
Prolapse:
- Besides bleeding, prolapse is a major symptom
- Goligher classification hinges on the degree of prolapse
- Patients with third-or fourth degree hemorrhoids often report something protruding from their anus and inflamed perianal tissue
Pain:
- Internal hemorrhoids are generally not painful unless they have been forcibly reduced or are incarcerated.
- Pain is usually caused by anal conditions like thrombosed external hemorrhoids or anal
fissures, which are located below the dentate line.
Itching:
- Itching around the anus is common in patients with internal hemorrhoids
- Increased perianal discharge from mucosal prolapse irritates the skin, causing itching.
- Itching (pruritus ani) can also result from conditions like mycosis, allergic dermatis,contact dermatitis, psoriasis, benign tumors, malignancies, oxyuriasis, and diabetes.
Discharge:
- Mucoid secretion typically occurs from the mucosa proximal to the dentate line.
- Prolapsed hemorrhoids can cause mucoid discharge.
- Mucoid discharge can also be a symptom of other conditions, including rectal polys anal fistulas, ulcerative colitis, Crohn’s disease, and irritable bowel syndrome.
Soiling:
- Some individuals with third and fourthdegree hemorrhoids may experience soiling due to mucus discharge, as fine regulation of continence is impaired.
- Incidence Or Pathogenesis Of Hemorrhoidal Disease In Pregnancy
Hemorrhoidal disease often troubles pregnant women, affecting 25-35% of pregnancies, mainly in the third trimester. It can be internal or external. During pregnancy, blood volume rises by 40_50%, leading to increased cardiac output and blood flow in pelvic veins. This higher pressure in the veins (vulvar, rectal, and lumbar) elevates the risk of developing hemorrhoids. The enlarged uterus compresses pelvic veins, and increased venous pressure along with hormonal changes in the first trimester causes venous relaxation. Estrogens cause tissue vascular displacement, while progesterone decreases venous tone, both contributing to hemorrhoid development.
Hemorrhoids are a common issue during pregnancy and spontaneous vaginal delivery. Increased intraabdominal pressure from uterine growth, a 30% increase in blood volume, hormonal changes, and constipation (affecting up to 38% of pregnant women) all contribute. Hemorrhoids peak in the last trimester and the first month postdelivery, affecting 25_35% of pregnant women, and up to 85% in certain populations during the third trimester. External hemorrhoid thrombosis occurs in 8% during the last trimester and 20% right after delivery. Preventing piles during pregnancy involves a combination of dietary, lifestyle, and hygiene practices:
- Eat a High Fiber Diet: Prevent constipation and reduce hemorrhoid risk by consuming fruits, vegetables, whole grains, and legumes.
- Stay Hydrated: Drink plenty of fluids (water and juices) to soften stools and ease bowel movements.
- Exercise Regularly: Promotes bowel regularity, improves blood circulation in the rectal area, and reduces hemorrhoid risk.
- Avoid Prolonged Sitting or Standing: Take breaks to move around and stretch your legs to prevent pressure on rectal veins.
- Avoid Straining During Bowel Movements: Don't resist the urge to pass stools, use a stool softener if needed, or elevate your feet with a footstool while on the toilet.
- Maintain Proper Hygiene: Keep the anal region clean and dry, use soft wipes instead of soaps or cloth to prevent irritation and itching.
- Ayurvedic Medicine Management
Ayurveda, a traditional Hindu medicinal practice originating from India, is now practiced worldwide. Recognized as an alternative or complementary therapy in the West, Ayurveda is holistic, addressing the mind, body, and spirit to bring balance and alleviate illness.
entral to Ayurveda are the three doshas: pitta (fire), vata (air), and kapha (water). Each dosha corresponds to specific elements and influences physical and emotional traits. The goal in Ayurveda is to balance these doshas through diet, lifestyle changes, and herbal remedies.
Panchakarma:
Panchakarma is an Ayurvedic therapeutic treatment aimed at cleansing the body and mind by removing toxins. It consists of five therapies: Vamana, Virechana, Basti, Shirodhara, and Nasya. This natural treatment is particularly effective for piles, with Vamana, Virechana, and Basti being the most beneficial for this condition. Before diving into the details of the treatments, let's consider what causes piles.
Panchakarma Treatments for Piles:
Vamana:
Ideal for patients with chronic indigestion and piles. Patients drink a decoction of liquorice or
Acorus calamus root to induce vomiting, ensuring purification with 4 to 6 bouts.
Figure 2: Vamana
Virechana:
Treats digestive disorders and constipation, making it perfect for piles. It thoroughly cleanses the
gastrointestinal tract, eliminating Pitta toxins from the liver, gall bladder, and small intestine.
Figure 3: Virechana
Basti:
Known as the "mother" of all Panchakarma treatments. It eliminates toxins from the three doshas (Vata, Pitta, Kapha) through the colon using ghee and herbal decoction. This treatment addresses constipation, irritable bowel syndrome, and digestive disorders.
Figure 4:Basti
Ayurvedic Churn for Piles:
Nagkeshar (Mesua ferrea Linn):
- This is also known as Ironwood or Cobra's Saffron. It is a valuable herb in Ayurveda.
It is a component of Misrakgana Chaturjat and is used in various formulations as Prakshepa Dravya1Nagkeshar is known for its Pachan (digestive) properties, aiding in improving digestion due to its Laghu (easy to digest) naturelIn Charak Samhita, Nagkeshar is described for use in Arsha Chikitsa (treatment of piles). Nagkeshar (Mesua ferrea Linn) has several beneficial properties, including being a diuretic,
analgesic, antipyretic, antibacterial, antifungal, antiarthritic, and antioxidant. In the context of
piles (hemorrhoids), Nagkeshar can be particularly useful due to its ability to pacify the Pitta
Dosha, which helps manage bleeding piles by balancing the body's heat.

Figure 5: Nag Keshar
Nagkeshar's action involves inhibiting acetylcholine and muscarinic receptors, resulting in smooth muscle relaxation. Its multifaceted properties make it a promising natural remedy for managing hemorrhoids.
Benefits of Nagkeshar:
- Bleeding Piles: Helps manage bleeding piles due to its astringent property1.
- Dysentery and Stomach Irritation: Powder form helps manage these conditions1.
- Topical Application: Reduces pain and inflammation due to its analgesic and anti-inflammatory properties1.
- Liver Health: Acts as a liver appetizer1.
- Reduces Colonic Motility: Helps with irritable bowel syndrome and reduces cramps.
- Aids Digestion: Enhances digestion and increases lung capacity for better Prana utilization.
- Anti-Spasmodic Effects: Relaxes smooth muscles, aiding in colonic motility and easing cramps.
Ayurvedic Approaches to Treating Piles and FistulaAyurveda offers a holistic approach to managing and treating piles and fistulas by balancing the three Doshas and enhancing overall health. Certain herbs are particularly effective as Ayurvedic medicines for these conditions.
- Touch-Me-Not Plant (Mimosa Pudica):
- Known for its healing properties in managing bleeding piles.
- Contains alkaloid mimosine, which eases pain and reduces inflammation.
- Application: A paste of touch-me-not leaves can be applied externally to the affected area.
- Example: Kerala Ayurveda Pilogest capsules contain touch-me-not and other herbs to provide relief and prevent recurrence.

Figure 6: Mimosa Pudica
- Triphala:
- A potent mix of three herbs: Amalaki, Bhibhitaki, and Haritaki.
- Excellent for constipation relief, promoting smooth evacuation, and reducing straining and piles risk.

Figure 7: Triphala
- Guggul:
- Properties: Guggul (Balsamodendron Mukul) is a potent anti-inflammatory herb in Ayurveda.
- Benefits: Reduces inflammation, manages hemorrhoidal concerns, and provides quick relief from piles. Its laxative and astringent properties help metabolize the bioactive etiologic components of hemorrhoids, eliminating toxins (Ama) and improving digestive health.

Figure 8:Guggul
- Turmeric:
- Properties: Turmeric (Haldi) is antimicrobial and anti-inflammatory, commonly found in Indian households.
- Benefits: Prevents secondary infections and manages bleeding from hemorrhoids. Helps reduce anal itching, shrinks hemorrhoids due to its astringent effect, and improves digestive fire (Agni) for better digestion and prevention of hemorrhoids.

Figure 9: Turmeric
Suppositories:
- Rectal suppositories are a useful way to administer medications, especially when oral intake is not possible. They can be particularly helpful for children and older adults who have difficulty swallowing pills or liquids.
- Common Uses of Rectal Suppositories:
- Fever-Reducing Medications: Acetaminophen can be used rectally if oral intake is compromised, reducing potential stomach and intestine side effects.
- Hemorrhoid Treatments and Laxatives: Historically used to treat hemorrhoids and relieve constipation.
Other Medications:
- Hydrocortisone: For inflammation.
- Mesalazine: For inflammatory bowel disease (IBD).
- Bisacodyl or Glycerol: For constipation relief.
- Promethazine or Ondansetron: For nausea and vomiting.
- Pain Medications: Such as ibuprofen or oxycodone.
This unique suppository preparation contains:
- Hydrocortisone Acetate I.P. 0.25%: Helps reduce inflammation.
- Lidocaine B.P. 3.00%: Acts as a local anesthetic to relieve pain.
- Zinc Oxide I.P. 5.00%: Provides a protective barrier and aids in healing.
- Allantoin B.P. 0.50%: Promotes wound healing and soothes irritation.
- Soluble Suppository Base: Ensures smooth delivery.
This combination makes it effective for treating piles and fissures, easy to use, and can be conveniently inserted into the rectum.
- Diet & Exercises
- Diet For Piles
Many foods are rich in fiber, which can help manage piles. Some of the best options include:
- Wheat Bran and Shredded Wheat: Just 1/3–1/4 of a cup of high-fiber bran cereal contains 9.1-14.3 grams of fiber, while 1–1/4 cups of shredded wheat cereal provides 5–9 grams of fibre. These cereals contain insoluble fiber, which adds bulk to stool and makes it easier to pass.
- Apples: A medium apple with its skin has about 4.4 grams of fiber. The insoluble fiber in the apple's skin helps bulk up stool, acting as a natural laxative.
- Pears: Pears are very high in fiber and contain compounds beneficial for people with hemorrhoids. A pear with its skin has about 6 grams of fiber and contains fructose, a natural laxative.
- Barley: Barley is rich in a fiber called ?glucan, which forms a viscous gel in the colon, softening the stool. Barley consumption can also promote good colon health.
- Corn: One cup of cooked sweet corn contains around 4.2 grams of fiber. Corn also has strong antioxidants that prevent cellular damage and compounds that may help reduce pain.
- Oatmeal: One cup of cooked oatmeal contains around 4 grams of fiber. The fiber in oats helps improve gut health, soften stool, and reduce the risk of straining.
- Lentils: Pulses like lentils, chickpeas, lima beans, and split peas are excellent sources of fiber. One cup of cooked lentils contains around 15.6 grams of fiber. Consuming green lentils can significantly increase stool weight and reduce the time it spends in the colon.
Foods to Avoid:
- Fried and salty foods
- Chips and other packaged snacks
- Full-fat dairy products
- Prepared or heavily processed foods
- Red meat
- Candies and chocolates
- Soda, sports drinks, energy drinks, and coffees with added milk, sugar, or cream
- Alcohol
- Excessive caffeine intake
- Exercises to Treat and Prevent Hemorrhds
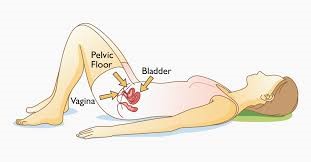
- Pelvic Floor Contractions:
- Strengthen your pelvic floor muscles to make it easier to pass stool and relax your anal sphincter, preventing straining.
- Lie on your back or sit.
- Contract your anal muscles as if stopping yourself from passing gas.
- Hold the contraction for 5 seconds.
- Relax for 10 seconds.
- Repeat 5 times.
- Repeat using only half your strength.
- Squeeze and relax the muscles as fast as you can.
- Continue for as long as possible.
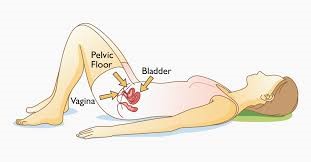
Figure 11: Pelvic floor contraction yoga
- Deep breathing:
This exercise helps alleviate pelvic floor muscle tension and promote relaxation.
- Sit up straight and place your hands above your waist on either side of your lower rib cage.
- With each inhale, breathe deeply into your abdomen, allowing your belly to expand.
- With each exhale, draw your navel toward your spine.
- Continue for up to 5 minutes.
Figure 12 : Deep Breathing Pose
- Child’s Pose (Balasana):
This pose helps increase circulation around your anus and relieve constipation while relaxing your lower back, hips, and legs. It’s said to provide a massage to your internal organs. To increase the pressure to your lower abdomen, place your fists or stacked palms on this area.
- Start on your hands and knees.
- Sit back, placing your hips on your heels.
- Extend your arms in front of you or relax them alongside your body.
- Rest in this position for up to 5 minutes.
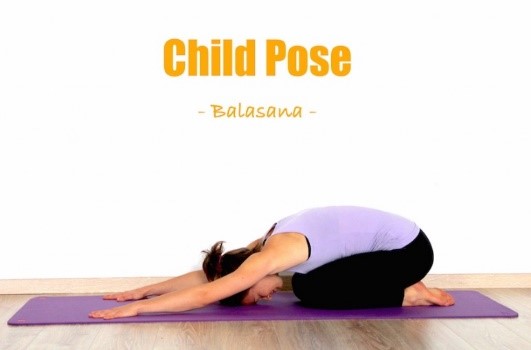
Figure 13: Balasana
- Legs Up-the-Wall Pose (Viparita Karani):
This asana can boost circulation to your anus while alleviating discomfort and irritation.
- Sit with your right side next to a wall.
- Place your legs up on the wall and lie down on your back.
- Place your arms in any comfortable position or give yourself a gentle abdominal massage.
- Hold this position for up to 15 minutes.

Figure 14: Viparita Karani
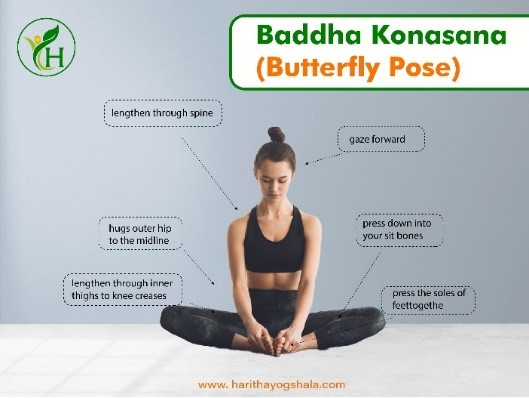
- Bound Angle Pose (Baddha Konasana):
This pose can strengthen and improve flexibility in your inner thighs, groin, and knees. It can also help stimulate your abdominal organs and soothe digestive discomfort.
- Sit with your sitting bones on a cushion, block, or folded blanket.
- Place the soles of your feet together and your knees out wide.
- Interlace your fingers around your pinky toes as you lengthen your spine.
- Stay in this position for up to 1 minute.
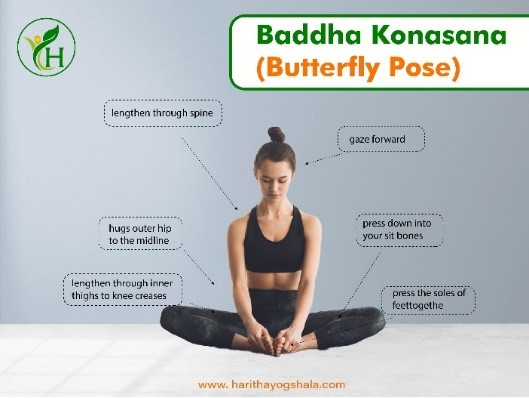
Figure 15: Baddha Konasana
- Treatments For Hemorrhoids:
- Conventional Surgical Treatment for Hemorrhoids:
Conventional surgery for hemorrhoids typically involves the excision of the piles1. This method is considered highly effective, especially when compared to outpatient procedures like rubber band ligation, sclerotherapy, and infrared coagulation2. The most commonly used techniques are:
- Open (Milligan-Morgan) Hemorrhoidectomy:
This involves cutting out the hemorrhoidal tissue1. It's known for its precise curative effect but can be associated with postoperative pain, bleeding, and other complications like urinary retention and anal stenosisl.
- Closed (Ferguson) Hemorrhoidectomy:
Similar to the Milligan-Morgan technique, but the dissection is done within the anal canal without pulling the hemorrhoid out3. This method also aims to reduce postoperative complications. A recent Cochrane Database review found that using bipolar energy in hemorrhoidectomy can shorten the procedure time and reduce postoperative pain compared to conventional surgery
- Closed Hemorrhoidectomy:
This is the most commonly used technique. It involves making an elliptical incision in the external hemorrhoidal tissue, extending through the dentate line to the upper limit of the hemorrhoids. Care is taken to remove only redundant anoderm and hemorrhoidal tissue. The wound is closed with continuous absorbable sutures, and usually three piles are excised. It's effective in 95% of cases with rare instances of surgical wound infection.
- Open Hemorrhoidectomy:
Preferred by many surgeons worldwide, this technique involves leaving the wound open. Studies comparing open and modified closed (semi-open) hemorrhoidectomy have shown faster healing and fewer postoperative complications with the modified technique. Common complications include urinary retention (2-36%), bleeding (0.03-6%), anal stenosis (0-6%), infection (0.5-5%), and incontinence (2-12%).
- Lateral Internal Sphincterotomy with Hemorrhoidectomy:
This combination should not be routine due to the risk of major complications like anal incontinence, although it's safe in selected cases with increased resting sphincter pressure.
- Hemorrhoidectomy Using Energy Sources:
Techniques like electric or ultrasonic scalpels might shorten surgery time and reduce blood loss, but they offer no advantage in terms of pain, healing time, or complications compared to conventional surgery.
- Open Hemorrhoidectomy with Bipolar Electrosurgical Scalpel:
- Associated with fewer postoperative analgesics, faster wound healing, and quicker return to work compared to using an electric scalpel.
- Offers no significant advantage in terms of postoperative pain, patient satisfaction, disease
recurrence, or complication rates.
- Injection Sclerotherapy:
- Used for treating bleeding hemorrhoids using various sclerosants (e.g., Ethanolamine
Oleate, 5% Phenol in Almond oil).
- Works by obliterating the hemorrhoid vascularity and inducing inflammation, leading to fibrosis and fixation of hemorrhoids.
- Generally requires only mild analgesics post-treatment.
- Complications may include anorectal abscess, necrotizing fasciitis, retroperitoneal sepsisand pulmonary allergic reactions.
- Less effective compared to other treatment modalities for hemorrhoids.
- Contraindicated in the presence of anal diseases such as fistulas, tumors, and anal fissures.
- Laser Therapy:
- Initially used with the Nd:YAG laser in the 1960s; later improved with CO2 laser and
pulsed/scanned lasers.
- CO2 laser open hemorrhoidectomy resulted in less postoperative pain and better
cosmetic outcomes compared to conventional surgery.
- Dopplerguided hemorrhoidal laser for thermal occlusion of hemorrhoidal arteries shows promising results but can be costly.
- The CO2 laser was found to be effective in providing partial to complete resolution of
grades II and III hemorrhoids with less pain and shorter recovery time compared to openhemorrhoidectomy.
- Bipolar Diathermy and Direct-Current Electrotherapy:
- Use local heat application to induce coagulation and fibrosis, resulting in hemorrhoid fixation.
- Comparable success rates to infrared coagulation with relatively low complication rates.
These various surgical treatments offer different benefits and complications, making it
essential to tailor the approach based on individual patient needs and conditions.
- Alternative Therapies for Piles:
- Nutrition and Dietary Supplements:
- Psyllium: This well-known fiber softens stool, reducing the pain associated with piles and making bowel movements smoother. It can be consumed with water or milk, but patients with inflammatory bowel disease should consult their doctor before use. Gradually increase the dose to avoid bloating.
- Probiotics: Good bacteria that maintain gut health. Regular consumption of probiotic-rich foods like curd and buttermilk helps reduce piles symptoms, speeds up healing, and prevents recurrence.
- Herbs:
The use of herbs in treating piles is a time-honored practice, but it's essential to use them under a doctor's supervision. Some commonly used herbs include:
•Witch Hazel (Hamamelis virginiana): Applied topically or as a sitz bath, it reduces pain by temporarily shrinking piles. Many over-the-counter pads for piles contain witch hazel.
•Goldenrod (Solidago virgaurea): Used topically to reduce inflammation.
•Gotu Kola (Centella asiatica): Helps with venous insufficiency or varicose veins.
•Yarrow (Achillea millefolium): Treats bleeding associated with hemorrhoids
- Other Home Remedies:
•Castor Oil: Reduces the size of piles and eases pain. Can be taken by adding to milk or applied topically.
•Tea Tree Oil: Has antimicrobial properties, keeping the inflamed site of piles germ-free. Applied topically.
•Coconut Oil: Acts as a moisturizer, relieving symptoms like swelling and inflammation, and reducing the urge to itch.
•Myrtle Essential Oil: Improves bleeding, pain, irritation, and itching for low-grade piles.
•Aloe Vera: Provides relief from burning, itching, and swelling when applied to the anus.
- Homeopathy:
•Aesculus: Used to manage piles with a burning sensation.
- Collinsonia: Effective for chronic, itchy hemorrhoids with constipation.
- Follow Good Toilet Practices:
- Limit toilet time to 3-5 minutes.
- Avoid excessive wiping and straining.
- Use moist toilet paper to clean and avoid rubbing the area.
- Do Sitz Baths:
- Sit in warm water for at least 15 minutes, 2-3 times daily.
- Avoid adding salts, lotions, or oils to the water.
- Maintain Proper Hydration:
- Drink adequate water to keep stool consistency.
- Avoid Caffeinated Beverages:
- Limit tea and coffee as they can harden stools and make defecation more painful.
- Indulge in Physical Activity:
- Light exercise helps maintain regular bowel habits and relieve constipation.
- Avoid Spicy and Processed Foods:
- These can aggravate piles symptoms like pain and discomfort.
- Avoid Certain Medications:
- Avoid painkillers like codeine and NSAIDs like ibuprofen as they can cause constipation and increase rectal bleeding.
- Use Ice Packs:
- Apply an ice pack wrapped in a soft towel to reduce swelling and pain.
- Sit Right:
- Elevate feet while passing stool to change rectum position and ease stool passage.
- Modify Your Clothing:
- Wear loose-fitting, breathable, cotton underwear and pants to prevent irritation and reduce symptoms.
- Skin Tags: Flap of tissue hanging off the anus, develops when the clot in a thrombosed hemorrhoid dissolve. Can be irritating.
- Anemia: Chronic bleeding from hemorrhoids can lower blood count.
- Infection: Untreated external hemorrhoids can become infected due to sores.
- Strangulated Hemorrhoid: Blood flow to a prolapsed hemorrhoid can be cut off, causing severe pain and bleeding.
- Blood Clots: Clots can form in piles, causing extreme pain and sometimes requiring drainage.
- Hemorrhage: The most common complication, where hemorrhoids rupture and cause serious rectal bleeding, needing immediate medical attention. Aggravated by passing hard stools.
- SUMMARY
Piles, or hemorrhoids, are swollen veins in the lower anus and rectum that can form lumps. They
vary in size and location, and many people may not realize they have them. Causes include
overexertion, chronic constipation, and straining during bowel movements. While many piles
resolve on their own, painful or visible piles might need surgical removal.
Treatment Approaches:
- Dietary and lifestyle modifications to radical surgery, depending on severity.
- Most hemorrhoids resolve on their own, but treatments focus on symptom relief, such as
warm baths, hydrocortisone cream, or suppositories.
- Preventative measures include exercising, drinking plenty of water, and eating more fiber to relieve constipation.
Hemorrhoids are very common, often caused by strain on the rectal veins. Risk factors include
chronic constipation, pushing during bowel movements, family history, and pregnancy. With
appropriate management and preventative measures, symptoms can be alleviated, and future
occurrences can be minimized.
CONCLUSION
The treatment of hemorrhoids ranges from dietary and lifestyle modifications to radical surgery, depending on the severity of the symptoms. While surgery is effective, it is reserved for advanced cases due to potential complications. Non-operative treatments, especially topical or pharmacological approaches, are often not fully effective. Thus, a deeper understanding of the pathophysiology of hemorrhoids is essential for developing innovative treatments.
Innovative Treatments:
- Emortrofine® Oro: A sublingual nano emulsion offering faster and complete absorption of its components compared to traditional tablets.
Emortrofine® Gel: A transparent liquid bandage clinically effective in reducing hemorrhoidal symptoms. It's safe for use during pregnancy, warranting further studies for this category where specific treatments are currently lacking.
REFERENCES
- Loder PB, Kamm MA, Nicholls RJ, Phillips RK. Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg. 1994;81:946–954. doi: 10.1002/bjs.1800810707.
- Morgado PJ, Suárez JA, Gómez LG, Morgado PJ. Histoclinical basis for a new classification of hemorrhoidal disease. Dis Colon Rectum. 1988;31:474–480.
- Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, et al. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis. 2009;24:105–113.
- Chung YC, Hou YC, Pan AC. Endoglin (CD105) expression in the development of haemorrhoids. Eur J Clin Invest. 2004;34:107–112.
- Fontem RF, Eyvazzadeh D. Internal Hemorrhoid. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
- Andler RS, Peery AF. Rethinking What We Know About Hemorrhoids. Clin Gastroenterol Hepatol. 2019 Jan;17(1):8-15.
- Hemorrhoids, American Society of Colon and Rectal Surgeons.
- Lawrence A, McLaren ER. External Hemorrhoid. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
- Piles, NHS, Last updated on: 28th March, 2022.
- Hemorrhoids, National Institute Of Diabetes and Digestive and Kidney Diseases.
- Altomare DF, Giannini I. Pharmacological treatment of hemorrhoids: a narrative review. Expert Opin Pharmacother 2013; 14(17):2343-2349
- Hills DL, Firth BG, Wi ni ford, Willer son IT. Pregnancy and cardiovascular abnormalities of clinical problems in cardiology. ABE. Milan: 1990; p. 917-927
- Struckmann JR, Meiland H, Bagi P, Juul-Jørgensen B. Venous muscle pump function during pregnancy. Assessment by ambulatory strain-gauge plethysmography. Acta Obstet Gynecol Scand 1990; 69(3):209-215
- Williams JW, Cunningham FG, Mc Donald PC, Gant NF. Williams obstetrics. 18th edAppleton & Lange. Nor walk: 1989; p. 129-168
- Cruikshank DP. Cardiovascular, pulmonary, renal and hematologic disease in pregnancy.In In: Scott JR, Disain PJ, Hammond CB, Spellacy WN, editors.editors Danforth’s obstetrics and gynecology. 6th ed Philadelphia: Lippincott. 1990; p. 433-459
- Plapler H, de Faria Netto AJ, da Silva Pedro MS. 350 am-bulatory hemorrhoidectomies using a scanner coupled to a CO2 laser. J Clin Laser Med Surg 2000; 18: 259-262
- Armstrong DN, Frankum C, Schertzer ME, Ambroze WL, Orangio GR. Harmonic scalpel hemorrhoidectomy: five hundred consecutive cases. Dis Colon Rectum 2002; 45: 354-359.
- Giordano P, Nastro P, Davies A, Gravante G. Prospective evaluation of stapled haemorrhoidopexy versus transanal haemorrhoidal dearterialisation for stage II and III haemorrhoids: three-year outcomes. Tech Coloproctol. 2011;15:67–73. doi: 10.1007/s10151-010-0667.
- Agnivesha, Charaka samhita, Ayurveda Deepika commentary of Chakrapani, edited by; Vaidya Yadavji Trikamji Acharya, Chaukhamba Orientalia, Varanasi, reprint; chikitsa sthana, 2015; 14: 27-31.
- Agnivesha, Charaka Samhita, Ayurveda Deepika commentary of Chakrapani, edited by; Vaidya Yadavji Trikamji Acharya, Chaukhamba Orientalia, Varanasi, reprint chikitsa sthana, 2015; 14: 21-22


 Sachitanand Biradar *
Sachitanand Biradar *
 Shweta Biradar
Shweta Biradar
 Sagar Shivange
Sagar Shivange






 10.5281/zenodo.14414911
10.5281/zenodo.14414911