Abstract
Iodine is an essential mineral and fundamental component of diet. It is well absorbed orally but oral consumption is food source depending and sometimes not meet daily requirement and the deficiency of iodine occurs. Iodine deficiency is a worldwide health problem and has various types of hazardous consequences. The body needs iodine to make thyroid hormones. The thyroid gland produces thyroid hormones. The two most important hormones are tetraiodothyronine (thyroxine or T4) and triiodothyronine (T3). Iodine deficiency can cause diseases such as hypothyroidism, goiter, and cause damage to brain. During pregnancy the need of iodine is additionally more for development of growing foetus. Hence to tackle this problem and useful method has been to reinforce the consumption of iodised salt. An iodine patch is designed in such a manner that it will look like a regular bindi. This bindi is expected to resolve the problem of iodine deficiency in many women. It appears to be simple but brilliantly designed method. As wearing of bindis is an important part of cultural practice of indian women since years this iodine patch is very easy to use for them. This iodine patches are adhesive in nature and can be put exactly in between their eyebrows. These have been impregnated with a solution of iodine. A wonderful innovation of this life saving bindi may be useful for different iodine deficiency issues and improving patient’s consistency.
Keywords
Iodine, Bindi, Iodine patch, Triiodothyronine, Tetraiodothyronine
Introduction
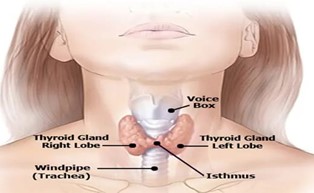
The thyroid gland helps in regulation of iodine levels in the body. This “thyroid” word is derived from greek word which means “shield” [1]. This gland is an endocrine gland located in the neck region (front of the throat, below the larynx (Adam’s apple) that produces and releases hormones which ultimately regulate metabolism, growth and development. Its shape is like a butterfly having 2 lobes on either side of the wind pipe connected by a thin tissue called as isthmus. The length of the lobe is about 4cm and width is about 1- 2 cm. [2] This gland produces thyroid hormones which are peptide containing iodine. Triiodothyronine (T3) and tetraiodothyronine (T4) are 2 most important hormones. In india most of the people face iodine deficiency problem due to inadequate intake of iodine in their diet. Around 350 million individuals have iodine deficiency problem since their time of birth.[3,5] Iodine deficiency issues are directly related to iodine deficient soil. As the iodine present in top most layer of soil, it is continuously filtered by various natural disasters such as glaciations (movement of a mass of ice over an area of land), flooding, cutting of trees, streams, shifting direction.[4,5]
Thus the crops cultivated on iodine deficient soil are having very less iodine content. Hence both human and animal will get low iodine in the eating regimen. Previous research data says that iodine deficiency may cause goiter, cretinism, hypothyroidism, early termination of birth, retardation of brain development, psychomotor disorder etc.[5,6,7] But recent studies found out that lack of iodine may cause intrauterine disorders such as intrauterine infections, intrauterine fetal demise, intrauterine growth restriction (IUGR). These diseases can cause several types of complications, which may be fatal.[8,9]
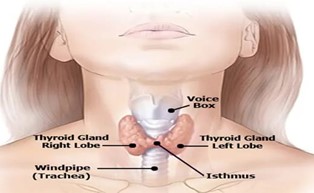
Fig no 1 : Thyroid gland
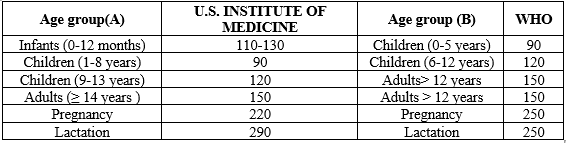
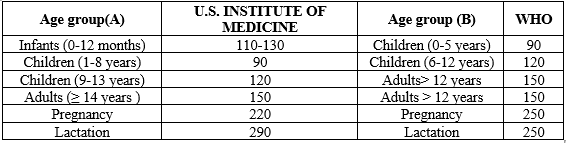
Recommended iodine intake on daily basis:
Epidemiology :
History :
The Bindi : tracing the history of our most iconic fashion. The bindi , a forehead decoration worn by women in india, has a long history that dates back to the third and fourth centuries. The art, sculptures and ancient texts depicts about bindi. [10] It was believed that women wear bindi to offer blood sacrifices to God. It was a part of ancient rituals. The term bindi comes from the ancient Sanskrit word “BINDU” meaning particle or “small drop”. It was common for women in urban locations to wear the bindi during 1930s and 1940s.[10,11]
Age to apply bindi :
Traditionally, women after marriage are used to wear bindi to symbolize her place as the family’s protector and sage of sorts. Now a days, however any women irrespective of her age and marital status can wear the bindi as a sign of their religious devotion and even for fashion region.[12,13]
Lifesaving bindi :
The attempt for incorporation of iodine into the traditional bindis is an unique, brilliant and simple idea. Because a bindi can be worn daily. Solution of iodine is impregnated in this bindi. A survey is carried out in mottu village, malkangiri, odisha. Mottu village total population is 1171, out of which female population is 44.6%. Village literacy rate is 64.0%. Out of 44.67.7?male have iodine deficiency issue.[14] Since these tribal women don’t take iodised salt, they are usually deficient in iodine. An iodine patch, which is designed in such a manner that it looks like a bindi is expected to correct these tribal women’s health crisis and maintain overall wellbeing.[15] Therefore, a firm hired and it has distributed many packets of iodine coated bindis to women, which will provide users an appropriate dose of iodine through their skin on their foreheads on daily basis.[16]
State government plan for iodine deficiency :
The Department of Health & Family Welfare, Government of Odisha has organised a programme
named Iodine Deficiency Disorder Control Programme (IDDCP) that aims in prevention and control of iodine deficiency disorders.[17]
Principle :
The National Iodine Deficiency Disorders Control Programme ( NIDDCP ) implemented in odisha since december 1989, which is a 100?ntral Plan Scheme.[18]
Goals :
The main goal lies in prevention and control of iodine deficiency disorder such as goiter, cretinism, mental retardation & deaf mutism etc. in the state. Another objective is to conduct the I.D.D surveillance in various medical colleges / research institutions in endemic districts according to the guide lines of Government of India.[19,20]
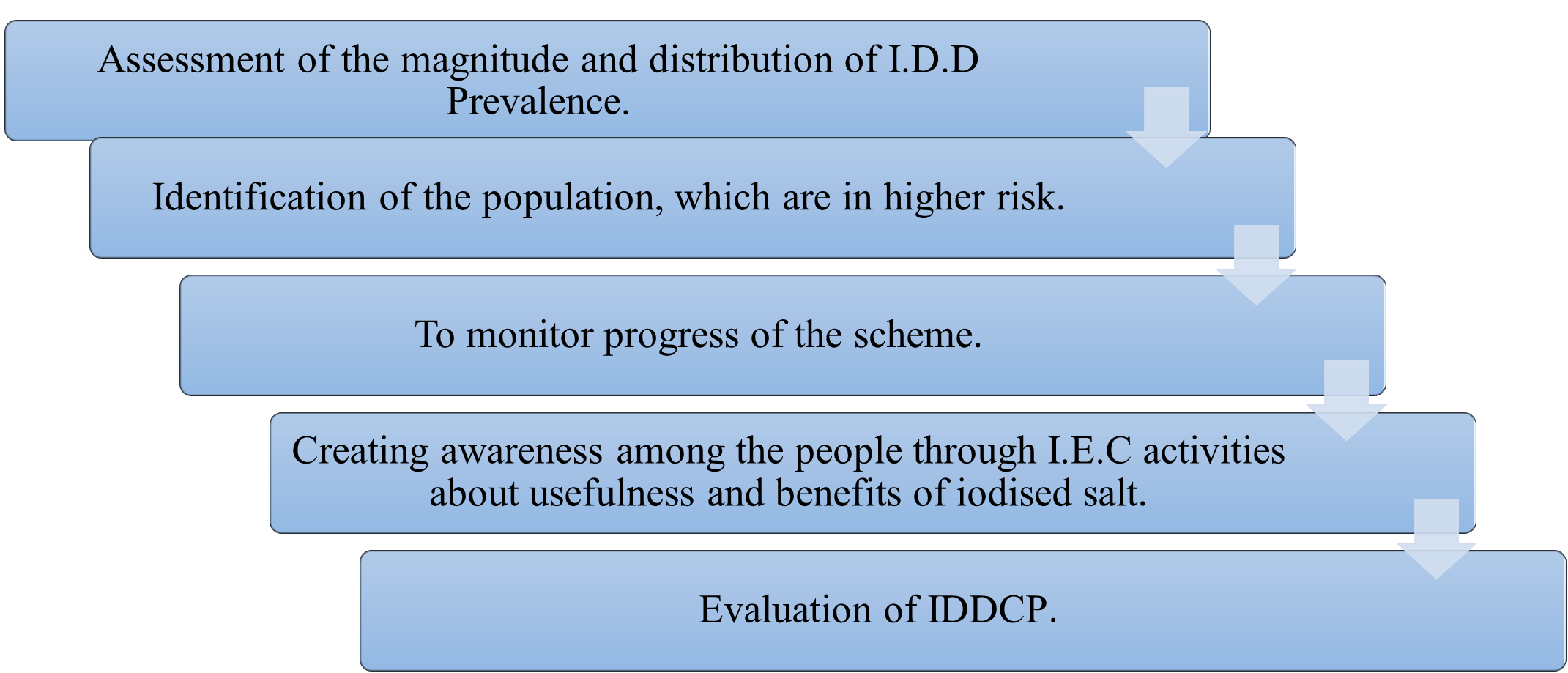
STEPS OF IDDCP :
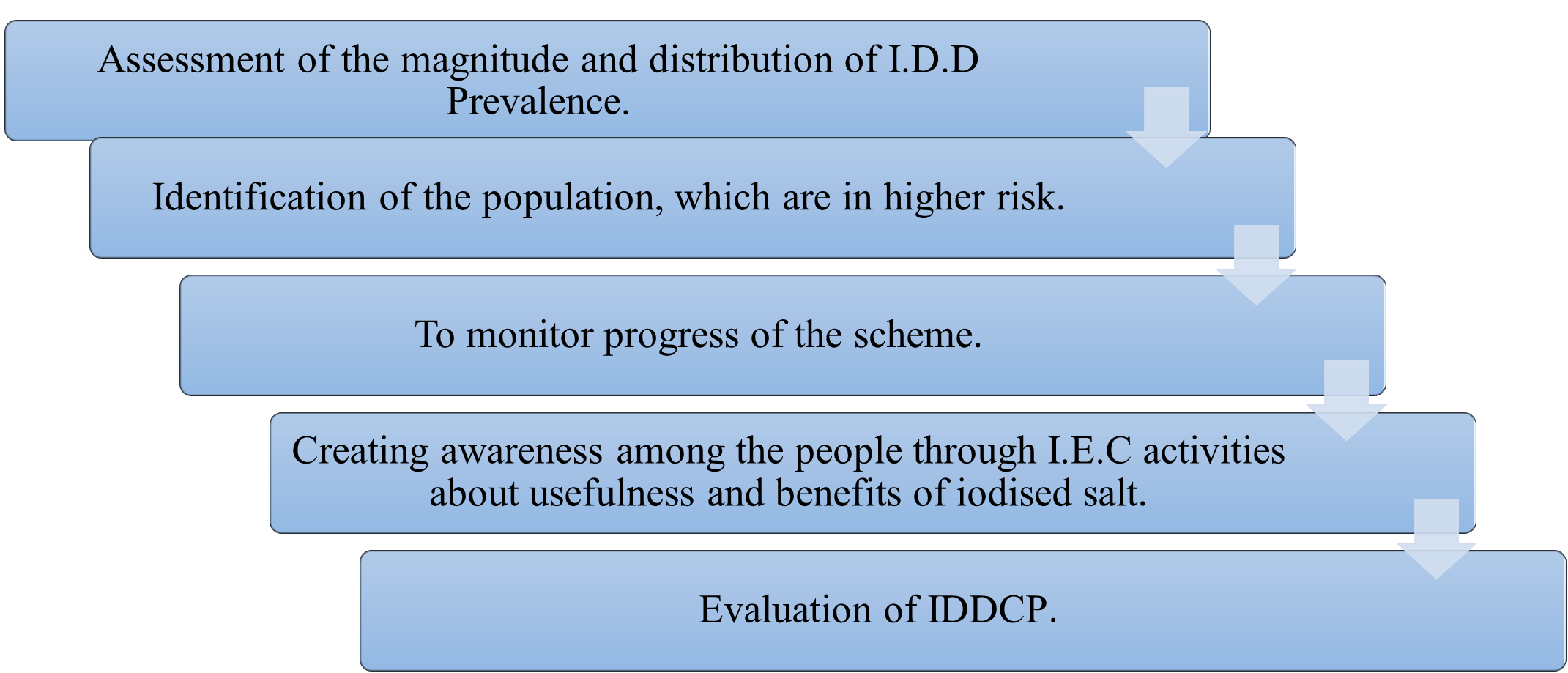
Figure 2: Steps of IDDCP
Activities :
As per guideline of Government of India – an IDD Monitoring Laboratory is established for analysis of salt samples and urine samples. Public awareness through electronic media, sensitisation seminars etc. is carried out.[21,22]
Iodine profile :
The name “Iodine” is derived from the greek word “Iodes” meaning violet. It was discovered by Bernard Courtois in 1811. [24] It is an essential nutrient for humans, who need a daily intake of about 0.1 milligrams. Our body contain upto 20 milligrams , mainly in the thyroid gland .
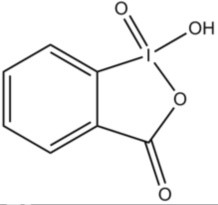
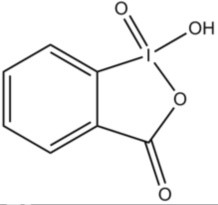
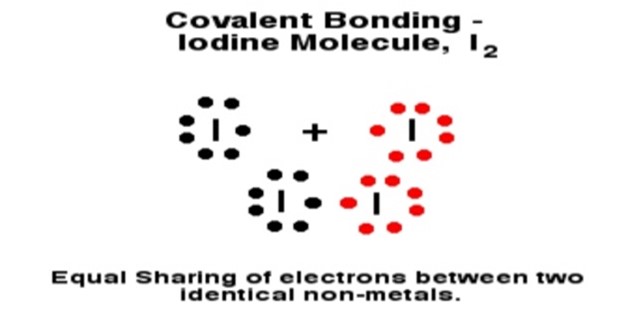
Fig 3 : Chemical structure of iodine
-
Allotropes : I2
- Group : 17
- Block : p
- Atomic number : 53
- State at 200C : solid
- Electron configuration: [Kr]4d105s25p5
- Melting point : 113.70C
- Boiling point : 184.40C
- Density ( g cm-3) : 4.933
- Relative atomic mass : 126.904
- Key isotopes : 127I
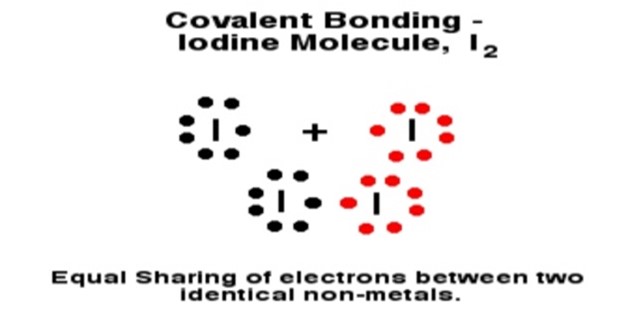
Figure 4 Bonding of iodine molecule
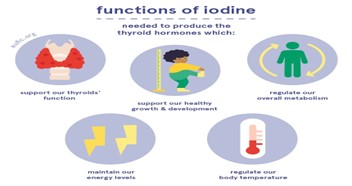
Functions of iodine :
- Production of thyroid hormone - Iodine helps thyroid gland to secrete 2 important thyroid hormones i.e tetraiodothyronine ( T4), triiodothyronine (T3). These hormones regulate metabolism of the body. During pregnancy and infancy these thyroid hormones plays a significant role in proper development of brain and bone of the foetus.
- Fibrocystic breast disease - Iodine helps in the treatment of Fibrocystic breast disease.
- Goiters - Iodine lowers the risk of goiters.
- Hyperthyroidism - Iodine is used for management of hyperthyroidism (an overactive thyroid gland)
- Cognitive function of brain - Iodine is essential for proper cognitive function of the brain especially in children.
- Growth & development – Iodine is crucial for proper growth and development of the body.[26,27]
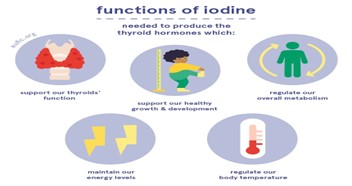
Figure 5 : Functions of iodine
Absorption, distribution, metabolism & excretion (ADME) of iodine in body :
Iodine is ingested in our body in various chemical forms. It is a trace element present in soil and water. Many foods contain iodine such as fish (cod and tuna), dairy products (milk, yogurt, cheese), eggs etc. But not everyone can get these foods. That’s why nutrient supplements (in various dosage forms) are given to the iodine deficient patients.[28,29] Most forms of iodine don’t remain in their original form rather they are converted into iodide in the abdomen. Iodide is almost entirely absorbed in the stomach and duodenum part of the small intestine. Kidney plays a major role in clearance of the iodine from the blood circulation. Half life of iodine is around 10hrs in blood plasma under normal conditions. But this time period may decline in case of an overactive thyroid gland. The thyroid gland becomes overactive due to iodine deficiency or hyperthyroidism. A healthy individual carries 15-20 mg of iodine. 80-85 % of which is available in the thyroid.[30,31] The thyroid cell has basolateral membrane. In this membrane iodide is transfered into the thyroid gland by the help of sodium/iodine symporter. During this transport the concentration gradient of iodine is 20-50 times that of the blood plasma. It is an active transport. When T3 and T4 degrades in the periphery, they release iodine that again enters the blood plasma. Most iodine, which is ingested is excreted through urine, while a small amount of iodine excreted in the faeces.[32,33] Iodine is one of the necessary nutrient during pregnancy. Mammary gland stores iodine and transfer it to new born through breast milk. Many body parts such as salivary glands, gastric mucosa, and choroid plexus take up iodine in trace amount. [34]
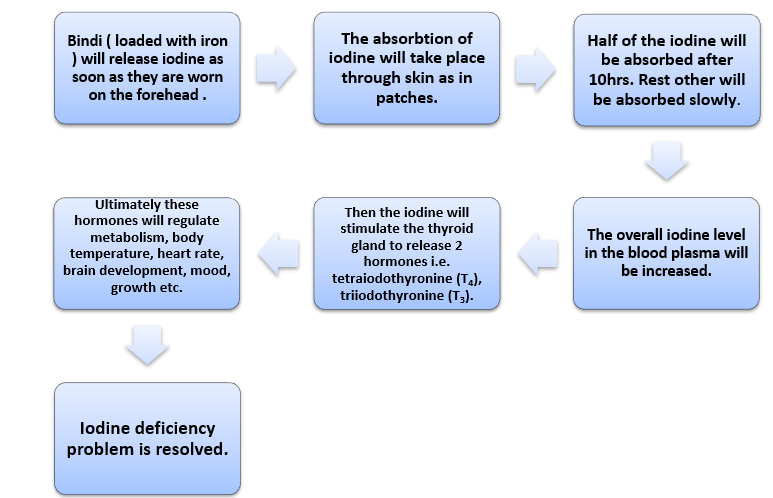
Iodine as a patch for bindi :
Most of the women across the developed countries get the required amount of iodine by way of their diet ( iodized salt ). But in developing countries especially in rural areas women have poor diet, which is unable to provide adequate amount of iodine. Because nutrition rich diet is quite expensive for them. As a result iodine deficiency occurs. To resolve this problem iodine transdermal patch is designed like a bindi.[33] The pH of the skin is the most important factor for any type of transdermal patch. The optimum pH of the skin in face and body parts lies in the range of 4.7 to 5.75. Hence this bindi should be compatible with this pH, otherwise various types of side effects such as itching, swelling, redness will appear. The bindi should be worn for atleast 8 hours on daily basis to get it’s therapeutic efficacy properly. About 150 – 250 microgram of iodine is incorporated in this bindi.[36]
Figure 6 : Life saving bindi
Effectiveness of bindi in females :
To detect whether a person is having iodine deficiency or not, iodine patch test is carried out. In this test a solution of iodine is applied to an abdomen or arm of the body. If the solution is quickly absorbed by the skin then ultimately the iodine will disappear from that part. Hence the person who is the subject in this test has iodine deficiency. The bindi should function on the same principle as the iodine patch test. However, some sources reveal that most of the iodine solution evaporates from the skin and only less than 12% is properly absorbed by the skin. If the thyroid gland needs only 150 micrograms of iodine, then a patient should be administered 3 times more than it’s required dose. Some scientists suggest that the body will take up only required amount of iodine and the rest part will be excreted out through urine.[35]
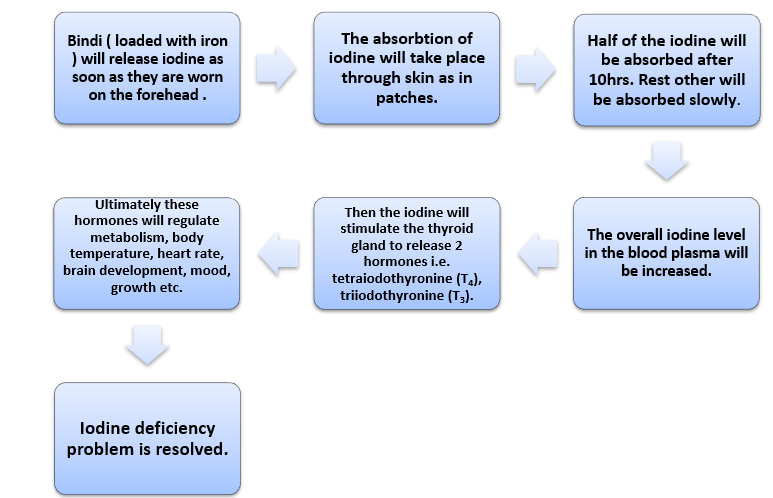
Fig 7 : Mechanism of action of iodine loaded bindi
This bindi loaded with iron is very simple to use for females. They will get the therapeutic efficacy of this patch without any extra effort. Because wearing a bindi is their one of the daily activities.
If we consider the cost in manufacturing of this bindi, then the cost is very less in comparision to other medications. Thus it will be less expensive for a patient to buy this iodine loaded bindi. Hence the patients will be benefited.[37]
CONCLUSION:
When a patient takes medicine, he or she has a perception that I have a disease and I have to take the required medications to treat this disease. But conversion of medication into daily used things by clever methodologies helped the patients to use the medicines for ornamental purpose. Innovation of Life Saving Bindi may combat different iodine deficiency messes in a protected and controlled manner. It not only resolve the iodine deficiency disorders but also improves patient compliances. From this above data, it concluded that life saving bindi approach is an efficient process to avoid deficiency of iodine, especially in adult girls and females and it will give very much impact to avoid iodine deficiency especially in vegetarian people (female). From the above study, it is found that govt. of odisha adopted a vast step to the people of malkanigiri, especially mottu area, who have suffered from iron deficiency need more focus on other tribal areas of india, not only india but also worldwide this approach / initiative especially for the female’s health care system.
REFERENCES
- National Research Council, Committee to Assess the Health Implications of Perchlorate Ingestion. Health Implications of Perchlorate Ingestion. Washington, DC: The National Academies Press, 2005.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press, 2001.
- World Health Organization. United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. Geneva, Switzerland: WHO, 3, 2007.
- Patrick L. Iodine: deficiency and therapeutic considerations. Altern Med Rev. 13(2), 2008, 116-127.
- Zimmermann MB. Iodine deficiency. Endocr Rev. 30(4), 2009, 376-408.
- Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 372(9645), 2008, 1251-1262.
- WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 10(12A), 2007, 1606-1611.
- Pennington JA, Young B. Iron, zinc, copper, manganese, selenium, and iodine in foods from the United States Total Diet Study. J Food Compost Anal. 3(2), 1990, 166-184.
- Pennington JAT, Schoen SA, Salmon GD, Young B, Johnson RD, Marts RW. Composition of Core Foods of the U.S. Food Supply, 1982-1991. III. Copper, Manganese, Selenium, and Iodine. J Food Comp Anal. 8(2), 1995, 171-217.
- Teas J, Pino S, Critchley A, Braverman LE. Variability of iodine content in common commercially available edible seaweeds. Thyroid. 14(10), 2004, 836-841.
- Dasgupta PK, Liu Y, Dyke JV. Iodine nutrition: iodine content of iodized salt in the United States. Environ Sci Technol. 42(4), 2008, 1315-1323.
- U.S. Department of Agriculture, Agricultural Research Service. USDA Nutrient Database for Standard Reference, Release 23.
- U.S. Food and Drug Administration, Code of Federal Regulations, CFR 21, Sections 184.1634 and 184.1265. Revised 2009.
- International Council for the Control of Iodine Deficiency Disorders. Accessed 9/13/201
- Santiago-Fernandez P, Torres-Barahona R, Muela-Martínez JA, Rojo-Martínez G, García-Fuentes E, Garriga MJ, León AG, Soriguer F. Intelligence quotient and iodine intake: a cross-sectional study in children. J ClinEndocrinolMetab. 89(8), 2004, 3851-3857.
- Vermiglio F, Lo Presti VP, Moleti M, Sidoti M, Tortorella G, Scaffidi G, Castagna MG, Mattina F, Violi MA, Crisà A, Artemisia A, Trimarchi F. Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. J ClinEndocrinolMetab. 89(12), 2004, 6054-6060.
- Dal Maso L, Bosetti C, La Vecchia C, Franceschi S. Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors. Cancer Causes Control. 20(1), 2009, 75-86.
- Ahad F, Ganie SA. Iodine, Iodine metabolism and Iodine deficiency disorders revisited. Indian Journal of Endocrinology and Metabolism. 14(1), 2010, 13-17.
- Maria-Jesus Obregon, Francisco Escobar del Rey, and Gabriella Morreale de Escobar. The effects of iodine deficiency on thyroid hormone deiodination. Thyroid. 15(8), 2005, 917-929. doi:10.1089/thy.2005.15.917.
- Ghent WR, Eskin BA, Low DA, Hill LP. Iodine replacement in fibrocystic disease of the breast. Can J Surg. 36(5), 1993, 453-60.
- Teng W, Shan Z, Teng X, Guan H, Li Y, Teng D, Jin Y, Yu X, Fan C, Chong W, Yang F, Dai H, Yu Y, Li J, Chen Y, Zhao D, Shi X, Hu F, Mao J, Gu X, Yang R, Tong Y, Wang W, Gao T, Li C. Effect of iodine intake on thyroid diseases in China. N Engl J Med. 354(26), 2006, 2783-93.
- Sooch SS, Deo MG, Karmarkar MG, Kochupillai N, Ramachandran K, Ramalingaswami V. Prevention of endemic goitre with iodized salt. Bull World Health Organ. 49, 1973, 307–12.
- McCarrison R. Observations on Endemic Cretinism in the Chitral and Gilgit Valleys. Proc R Soc Med. 2, 1909, 1–36.
- Stott H, Bhatia BB, Lal RS, Rai KC. The distribution and cause of endemic goitre in the United Provinces. Indian J Med Res. 18, 1931, 1059–85.
- http://dghs.gov.in/content/1348_3_NationalIodineDeficiency.aspx
- Geneva: World Health Organization; 1990. World Health Organization. Prevention and Control of Iodine Deficiency Disorders, Report to 43rd World Health Assembly. WHA432.
- Bueren GV. World Declaration and Plan of Action on the Survival, Protection and Development of Children. Chapter 72. Martinus WW Nijhoff Publishers; International documents on children; 1998, 414–35.
- New York: 2002. May, [accessed on 2011]. United Nations. United Nations General Assembly Special Session on Children. UNGASS. United Nations Non- Governmental Liaison Service (NGLS) Round up 92. Available from: http://www.un-ngls.org/orf/pdf/ru92kids.pdf.
- Rhee CM, Bhan I, Alexander EK, Brunelli SM. Association between iodinated contrast media exposure and incident hyperthyroidism and hypothyroidism. Arch Intern Med. 172, 2012, 153–159.
- Gordon CM, Rowitch DH, Mitchell ML, Kohane IS. Topical iodine and neonatal hypothyroidism. Arch PediatrAdolesc Med. 149, 1995, 1336–1339.
- Linder N, et al. Topical iodine-containing antiseptics and subclinical hypothyroidism in preterm infants. J Pediatr. 131, 1997, 434–439.
- Vermeulen H, et al. Benefit and harm of iodine in wound care: a systematic review. J Hosp Infect. 76, 2010, 191–199.
- Ader AW, et al. Effect of mouth rinsing with two polyvinylpyrrolidone-iodine mixtures on iodine absorption and thyroid function. J ClinEndocrinolMetab. 66, 1988, 632–635.
- Safran M, Braverman LE. Effect of chronic douching with polyvinylpyrrolidone-iodine on iodine absorption and thyroid function. Obstet Gynecol. 60, 1982, 35–40.
- McMonigal KA, et al. Thyroid function changes related to use of iodinated water in the U.S. Space Program. Aviat Space Environ Med. 71, 2000, 1120–1125.
- Georgitis WJ, McDermott MT, Kidd GS. An iodine load from water-purification tablets alters thyroid function in humans. Mil Med. 158, 1993, 794–797.
- Pearce EN, et al. Effects of chronic iodine excess in a cohort of long-term American workers in West Africa. J ClinEndocrinolMetab. 87, 2002, 5499–5502.
- Abraham GE, Flechas JD, and Hakala JC. “Orthoiodosupplementation: Iodine sufficiency of the whole human body.” The Original Internist, 9(4), 2002, 30-41.
www.neelvasantfoundation.org/event.html


 Rajlaxmi Patro*
Rajlaxmi Patro*
 Pratikshya Mohapatra
Pratikshya Mohapatra
 Chandan Nayak
Chandan Nayak
 Manoranjan Sahu
Manoranjan Sahu
 10.5281/zenodo.13881960
10.5281/zenodo.13881960