Abstract
One of the most prevalent chromosomal diseases, Klinefelter syndrome (KS), affects between 1 in 500 and 1 in 1,000 male infants. The extra X chromosome (47,XXY) that characterizes KS causes a range of clinical symptoms from mild to severe that affect both cognitive and physical development. This article explores the pathophysiology and genetic etiology of Klinefelter syndrome, emphasizing the role of chromosomal abnormalities in disrupting normal male development. Examined are the developmental effects of KS, such as hypogonadism, gynecomastia, and cognitive deficits, as well as the related comorbidities and how these affect the quality of life of the patient. In addition, KS has characteristics with other developmental disorders; differential diagnosis is essential. This paper describes the advanced genetic testing methodology and essential diagnostic criteria for KS. In order to give people with KS a comprehensive management plan, we also examine new and existing therapeutic modalities, such as hormone replacement therapy, methods for preserving fertility, and psychosocial interventions. This review aims to educate medical professionals and researchers on the most recent advancements in the diagnosis and treatment of Klinefelter syndrome by recognizing the complicated and multifaceted character of this disorder.
Keywords
Klinefelter syndrome, Male, Extra chromosomes, Abnormal sexual development, Chromosomal disorder, XXY.
Introduction
XXY male, XX male, XXYY male, XXXY male, XXXXY male, Klinefelter syndrome (KS). Harry F. Kleinfelter initially identified Klinefelter's syndrome in 1942 as an endocrine condition marked by gynecomastia, hypogonadism, small hard testes, and higher-than-normal follicle-stimulating hormone (FSH) concentrations. In 1959, the cause of the condition was identified as an extra X chromosome.[2] The karyotypes 47, XXY, and 20% of higher-grade chromosome aneuploidies, 46, XY/47, XXY mosaicism, or aesthetically defective X chromosomes are seen in about 80% of KS males, according to current studies.[3] The most prevalent sex-chromosome abnormality is KS, believed to affect roughly 1 in 600 newborn males. [4] Male Klinefelter syndrome, 47,XXY (KS), is the most common chromosomal abnormality in males, occurring in around 150 out of every 100,000 individuals. 1942 saw the first description of it. [5] Patients with Klinefelter syndrome have an elevated risk of mental impairment, psychological abnormalities, and criminal behavior, according to alarming findings from early studies on individuals in cells and mental health facilities. [6] Klinefelter's syndrome is still poorly understood in a large number of cases. According to Abramsky and Chapple's [7] calculations, 26% of diagnosed cases occurred in childhood or adulthood due to gynecomastia, infertility, or hypogonadism, while 64% of predicted cases remained undiagnosed. Less than 10% of presented diagnoses for Klinefelter's syndrome are made before puberty, according to large Danish national registry research, confirming the illness's widespread underdiagnosis. [8] Traditionally, the "prototypic" male with Klinefelter syndrome has been characterized as tall, with broad hips, narrow shoulders, gynecomastia, tiny testes, and a testosterone deficit, as well as a diminished IQ. [9] Since then, a different phenotype has been identified, where individuals exhibit fewer clinical characteristics than those shown in the traditional phenotype.[10] As a result, the diagnosis is frequently made by pediatric neurologists or psychiatrists who also conduct fragile X screening in addition to chromosome analysis. The characteristic tall stature of KS boys arises from a significant increase in height velocity due to increased leg growth between the ages of 5 and 8 years; otherwise, it is very difficult to identify any physical distinctions between KS boys and normal boys. Moreover, there are no differences in the pubertal growth spurt's timing or magnitude compared to typical boys. Small, firm testes and varying signs of androgen insufficiency are characteristics of KS boys that are most frequently found among azoospermic patients who seek infertility clinics, but only after puberty.[12] Urologists are well positioned to manage the reproductive and sexual function of patients with Klinefelter syndrome throughout the long term. Therefore, we think it's critical to give translational scientists and practicing clinicians a current understanding of the etiology and treatment of Klinefelter syndrome. In men with Klinefelter syndrome, this study focuses on recent advances in reproductive biology and medicine [13].
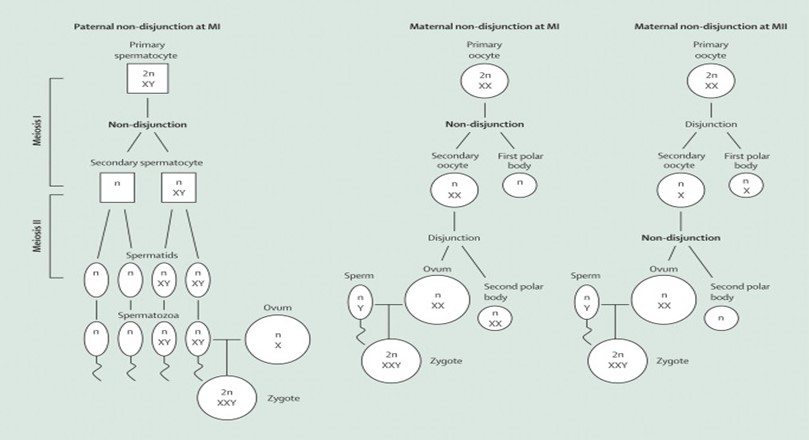
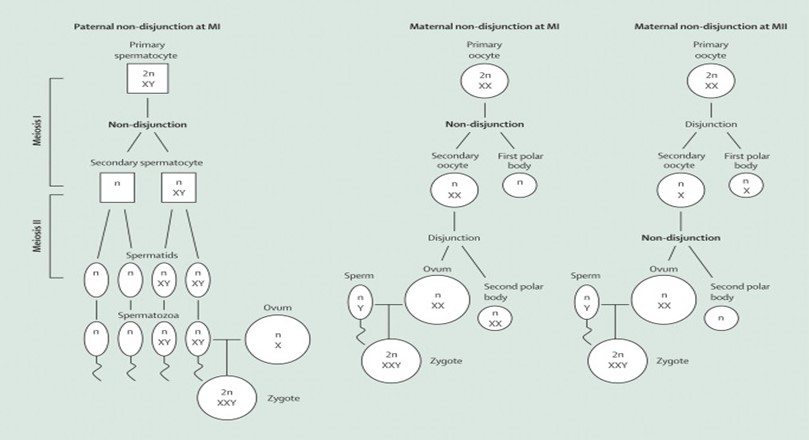
Fig 1: shows three different scenarios where these errors, called non-disjunctions, can happen
. Paternal non-disjunction: During sperm formation, the X and Y chromosomes fail to separate properly, leading to sperm with both an X and Y chromosome. If this sperm fertilizes a normal egg, the resulting zygote will have the XXY pattern.
Maternal non-disjunction at Meiosis I: During the first division in egg formation, both X chromosomes go into one egg instead of separating. If this egg, with two X chromosomes, is fertilized by a Y-bearing sperm, the zygote will have an XXY pattern. Maternal non-disjunction at Meiosis II: In the second division of egg formation, a similar failure to separate occurs, leading to an egg with two X chromosomes. Again, if fertilized by a Y-bearing sperm, the result is an XXY zygote.
PREVALANCE:
Klinefelter syndrome has been characterized as "not uncommon" from the first published study, but its prevalence was not established until multiple large-scale sex-chromosome surveys were conducted on newborn babies.[16] Prevalence of pregnancy Out of 85,650 fetuses examined between 1986 and 2006, 152 were found to have a KS karyotype. Since approximately 51% of births are male fetuses, 43,682 is the denominator used in prevalence calculations. [17]
STATISTICAL METHODS :
The percentage of all male pregnancies is always used to illustrate the prevalence of XYY and XXY. It seems that the distribution of male and female fetuses is 50:50 in research where the total number of pregnancies is the only data provided. Since the bulk of these mosaics are the product of trisomic conceptions and there is evidence that the prevalence of XXX is always expressed as a fraction of all female pregnancies, all analyses include mosaics with a normal and a trisomic cell line. [18]
EPIDMIOLOGY:
Klinefelter syndrome, estimated to occur in 1 in 500–1 in 1000 live births, is the most prevalent numerical chromosomal anomaly among men [34]. The most prevalent type of X chromosome polysomy, known as X disomy, is associated with Klinefelter syndrome (47, XXY). Nonmosaic X chromosomal polysomy affects 90% of men with Klinefelter syndrome [35].
With a prevalence of one in 500 males, XXY aneuploidy is the most prevalent sex chromosome abnormality in humans [36]. Less frequently occurring sex chromosomal aneuploidies are 48,XXYY and 48,XXXY, which are found in 1 in 17,000 to 1 in 50,000 male births. One in every 85,000 to 100,000 male births is the incidence of 49,XXXXY [37]. Reports have also been made on 46,XX male cases.
ETIOLOGY:
47,XXY is the most prevalent KS karyotype (more than 90%). There have been descriptions of mosaic karyotypes 46, XY/47, and other aneuploidies 48, XXXY, and 49, XXXXY. Post-zygotic or meiotic nondisjunction typically brings about the acquisition of the additional X chromosome randomly. [19] It is not possible for KS to be inherited or inheritable.
There seems to be a correlation between the amount of extra X chromosomal material present and the overall severity of the condition. [20]The most frequent cause of Klinefelter syndrome is one extra copy of the X chromosome in each cell (XXY).
- Mosaic Klinefelter syndrome, which has an extra X chromosome in some cells but fewer symptoms
- Multiple extra copies of the X chromosome, an uncommon condition that causes a severe form
SYMPTOMS:
Atrophic testes, gynecomastia, and varying degrees of hypogonadal symptoms are typical clinical signs of Klinefelter syndrome. It is possible that some people may not exhibit these common clinical symptoms.
GYNAECOMASTIA:
In typical guys going through puberty, gynecomastia is a common occurrence that can be extremely harmful. Researchers propose that boys with Klinefelter syndrome may experience gynecomastia due to a lower testosterone level and a comparatively increased estrogen level. Gynecomastia may resolve with testosterone therapy, while some individuals prefer to have the breast tissue surgically removed. [21]
HYPOGONADISM:
In comparison to males with normal hormone levels, those affected with Klinefelter syndrome may experience delayed or decreased development of typical male secondary sexual traits, such as decreased growth of their beards, lower muscular mass, and decreased amounts of secondary body hair. (22)
DIABETES AND THE METABOLIC SYNDROME:
Numerous case studies have indicated a correlation between Klinefelter syndrome and diabetes; however, the reasons for this correlation are still unknown. studies on the epidemiology of both morbidity and mortality. (23)
DEVELOPMENT ABNORMALITIES:
KLINEFELTER SYNDROME AND CARDIOVASCULAR RISK:
In their analysis of a cohort of 4865 subjects, which consisted of 4033 controls and 832 KS, Bojesen and colleagues found that KS patients were more likely to have peripheral vascular disease (SMR, 7.9; 95% CI, 2.9–17.2), pulmonary embolism (SMR, 5.7; 95% CI, 2.5–11.3), ischemic heart disease (SMR, 0.7; 95% confidence interval, CI, 0.5–0.9), and intestinal thrombosis resulting in intestinal vascular insufficiency (SMR, 12.3; 95% CI, 4.0–28.8) [24]. However, SMR was significantly lower in both mosaic and non-mosaic KS, but not in men with more than three sex chromosomes. Swerdlow and colleagues reported that the SMR was significantly higher for all of the aforementioned diseases except for ischemic heart disease [25].
KLINEFELTER SYNDROME AND THROMBOSIS/LEG ULCERS:
Even in the absence of a trigger, patients with KS are more likely to experience thrombosis or develop leg ulcers. Furthermore, as numerous case reports have demonstrated, the co-existence of one or more thrombophilic diseases—such as diabetes, hypertension, or obesity—that are more common in Kansas can increase this risk, though these disorders are not the primary causes. A worse prognosis is the hallmark of the relationship between KS and thrombophilic diseases. In the absence of a triggering event, Lapecorella and colleagues described the case of a 39-year-old patient with KS who experienced a severe deep vein thrombosis and pulmonary embolism. Double heterozygosis for Leiden factor V and G20210A prothrombin mutations was linked to this illness [26]. In fact, the literature reports a variety of thrombosis and leg ulcer cases caused by different mechanisms. Following TRT, certain recurring leg ulcer patients that were linked to immunological diseases (positive antinuclear factor, antiphospholipid antibodies, and cryoglobulins) but did not have venous insufficiency have recovered [27].
DIFFERTIAL DIAGNOSIS:
A small sample of blood or other tissue is used to determine the karyotype, which is used to diagnose Klinefelter syndrome. The ability to identify speech issues and academic challenges that call for speech treatment and educational help makes early recognition of the syndrome crucial. Furthermore, treatment or prevention of the long-term effects of gonadal insufficiency is made easier by early detection. Some people with Klinefelter syndrome may be able to avoid becoming infertile in the future by avoiding the testicular damage brought on by protracted luteinizing hormone (LH) hyperstimulation. [28]. 47,XXY boys may present with a range of mild age-related clinical symptoms if the diagnosis is not detected during pregnancy. Males with 47,XXY may undergo chromosomal assessments in infancy to check for cryptorchidism, tiny phallus, or hypopadias [29]. The school-age youngster may have behavioral/social issues, learning impairments, or language delays [30]. Adults are frequently examined for breast cancer or infertility [31].
Variability is often observed in the physical signs of Klinefelter syndrome. A karyotype investigation may be recommended for a male who is undiagnosed if he exhibits the following characteristics:
- Tiny testicles
- Gynecomastia
- Prolonged limbs and legs
- Delay in development
- Impaired language and speech
- Academic problems or learning disabilities
- Difficulties with psychology
- Problems with behavior
It is necessary to take into account additional hypogonadism causes, such as Kallmann syndrome [32].
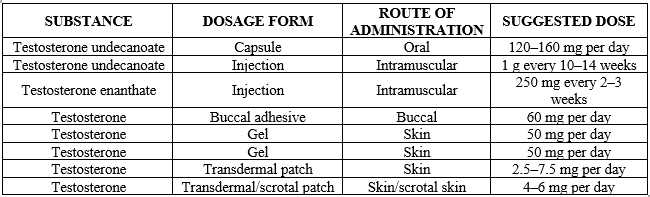
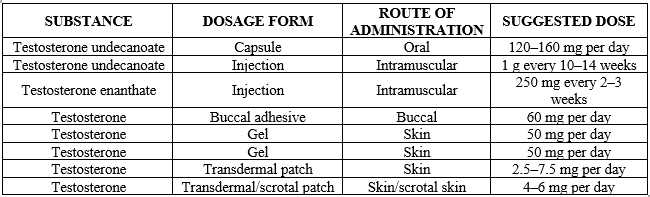
Table 1: Management for Klinefelter syndrome [33]
DISCUSSION:
Our understanding of knowledge is evolving, and it now has many features due to the addition of a wealth of new information in recent years. [34] Our personal experience and published findings suggest that most boys with Klinefelter syndrome are born with spermatogonia, which undergo extensive apoptosis most likely during early puberty, and that the loss of spermatogonial cells in males with the illness proceeds gradually [35, 36]. Over 97% of men with Klinefelter syndrome are infertile; hence, every attempt should be made to preserve fertility in children who have been identified with the condition [37]. For instance, the rate of breast cancer deaths in males with Klinefelter's syndrome is comparable to that in women [38]. Klinefelter's syndrome affects about 2 out of every 50 men who have breast cancer [39], which is comparable to the proportion among the men with SLE in this study. Patients with Klinefelter's syndrome may have elevated serum levels of rheumatoid factor [40]. Infertility may exist in males with 46, XX, as well as decreased testosterone levels and elevated LH and FSH levels [41].
CONCLUSION:
In conclusion, Klinefelter syndrome is a genetic condition resulting from an extra X chromosome in males, leading to a range of physical, reproductive, and developmental challenges. Although there is no cure, early diagnosis and tailored treatments such as testosterone replacement therapy, educational support, and fertility assistance can help manage symptoms and improve quality of life. With appropriate care and intervention, individuals with Klinefelter syndrome can lead fulfilling lives. Klinefelter syndrome, characterized by the presence of an extra X chromosome in males, presents various challenges, including physical, reproductive, and cognitive issues. Early diagnosis and intervention are crucial for managing these challenges. Treatment options such as testosterone replacement therapy, educational support, and fertility treatments can significantly improve the quality of life. Although the syndrome can impact different aspects of a person's life, many individuals with Klinefelter syndrome can lead healthy and fulfilling lives with the right support and care.
REFERENCE
- Klinefelter HF, Reifenstein EC, Albright F. Syndrome characterized by gynecomastia, aspermatogenesis without Leydigism, increased excretion of follicle stimulating hormone. J Clin Endocrinol 1942; 2: 615–27.
- Jacobs PA & Strong JA. A case of human intersexuality having a possible XXY sex-determining mechanism. Nature 1959; 183: 302–303.
- Lanfranco F, Kamischke A, Zitzmann M et al. Klinefelter’s syndrome. Lancet 2004; 364: 273–283.
- Bojesen A, Juul S & Gravholt CH. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. The Journal of Clinical Endocrinology and Metabolism 2003; 88: 622–626.
- Klinefelter HF, Reifenstein EC, Albright F 1942 Syndrome characterized by gynecomastia, aspermatogenesis without a-Leydigism, and increased excretion of follicle-stimulating hormone. J Clin Endocrinol 2:615– 627
- Maclean N and Mitchell JM (1962) A survey of sexchromosome abnormalities among 4,514 mental defectives. Lancet 1: 293–296
- Abramsky L, Chapple J. 47,XXY (Klinefelter syndrome) and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling. Prenat Diagn 1997; 17: 363–68.
- Bojesen A, Juul S, Højbjerg Gravholt C. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab 2003; 88: 622–26.
- Smyth CM and Bremner WJ (1998) Klinefelter syndrome. Arch Intern Med 158: 1309–1314
- Simpson JL et al. (2003) Klinefelter syndrome: expanding the phenotype and identifyig new research directions. Genet Med 5: 460–468
- Ratcliffe S. Long-term outcome in children of sex chromosome abnormalities. Archives of Disease in Childhood 1999; 80: 192–195.
- Robinson A, Bender BG, Borelli JB et al. Sex chromosomal aneuploidy: prospective and longitudinal studies. Birth Defects Original Article Series 1986; 22: 23–71.
- Paduch DA, Fine RG, Bolyakov A, Kiper J. New concepts in Klinefelter syndrome. Current Opinion in Urology. 2008 Nov 1;18(6):621-7.
- Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E. Klinefelter's syndrome. The Lancet. 2004 Jul 17;364(9430):273-83.
- Bonomi M, Rochira V, Pasquali D, Balercia G, Jannini EA, Ferlin A., Klinefelter ItaliaN Group (KING). Klinefelter syndrome (KS): genetics, clinical phenotype and hypogonadism. J Endocrinol Invest. 2017 Feb;40(2):123-134.
- Nielsen J and Wohlert M (1990) Sex chromosome abnormalities found among 34,910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Birth Defects Orig Artic Ser 26: 209–223
- Australian Bureau of Statistics. Births Australia 2006. Canberra: ABS, 2006: (ABS Cat. No. 3301.0.)
- Hassold T : Mosaic trisomies in human spontaneous abortions. Hum Genet 1982; 61: 31–35.
- Davis S, Howell S, Wilson R, Tanda T, Ross J, Zeitler P, Tartaglia N. Advances in the Interdisciplinary Care of Children with Klinefelter Syndrome. Adv Pediatr. 2016 Aug;63(1):15-46. [PMC free article] [PubMed]
- Bonomi M, Rochira V, Pasquali D, Balercia G, Jannini EA, Ferlin A., Klinefelter ItaliaN Group (KING). Klinefelter syndrome (KS): genetics, clinical phenotype and hypogonadism. J Endocrinol Invest. 2017 Feb;40(2):123-134. [PMC free article] [PubMed].
- Salbenblatt JA et al. (1985) Pituitary–gonadal function in Klinefelter syndrome before and during puberty. Pediatr Res 19: 82–86Salbenblatt JA et al. (1985) Pituitary–gonadal function in Klinefelter syndrome before and during puberty. Pediatr Res 19: 82–86
- Smyth CM and Bremner WJ (1998) Klinefelter syndrome. Arch Intern Med 158: 1309–1314
- Bojesen A et al. (2006) Morbidity in Klinefelter syndrome: a Danish register study based on hospital discharge diagnoses. J Clin Endocrinol Metab 91: 1254–126
- Bojesen A, Juul S, Birkebaek N, Gravholt CH (2006) Morbid ity in Klinefelter’s syndrome: a Danish register study based on hospital discharge diagnoses. J Clin Endocrinol Metab 91(4):1254–1260
- Swerdlow AJ, Higgin CD, Schomaker MJ, Wright AF, Jacobs PA (2005) Mortality in patients with Klinefelter’s syn drome in Britain: a cohort study. J Clin Endocrinol Metab 90(12):6516–6522
- Lapecorella M, Marino R, De Pergola G, Scaraggi FA, Spe ciale V, De Mitrio V (2003) Severe venous thromboembolism in a young man with Klinefelter’s syndrome and heterozygosis for both G20210A prothrombin and factor V Leiden mutations. Blood Coagul Fibrinolysis 14(1):95–98
- Igawa K, Nishioka K (2003) Leg ulcer in Klinefelter’s syndrome. J EurAcad Dermatol Venereol 17(1):62–64
- Bojesen A et al. (2003) Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab 88: 622–626 13 Hook EB (1981) Rates of chromosome abnormalities
- Caldwell PD, Smith DW: The XXY (Klinefelter's) syndrome in childhood: detection and treatment. J Pediatr 1972, 80:250-258
- Walzer S, Wolff PH, Bowen D, Silbert AR, Bashir AS, Gerald PS, Richmond JB: A method for longitudinal study of behavioral development in infants and children: the early development of XXY children. J Child Psychol Psychiat 1978, 19:213-229
- Okada H, Fujioka H, Tatsumi N, Kanzaki M, Okuda Y, Fujisawa M, Hazama M, Matsumoto O, Gohji K, Arakawa S, Kamidono S: Klinefelter's syndrome in the male infertility clinic. Hum Reprod 1999, 14:946-952
- Visootsak J, Graham JM. Klinefelter syndrome and other sex chromosomal aneuploidies. Orphanet journal of rare diseases. 2006 Dec;1:1-5.
- Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E. Klinefelter’s syndrome. Lancet 2004; 364:273–283.
- Lue Y, Liu PY, Erkkila K, Ma K, Schwarcz M, Wang C, Swerdloff RS 2010 Transplanted XY germ cells produce spermatozoa in testes of XXY mice. Int J Androl 33:581–587[1]
- Aksglaede L, Wikstrom AM, Rajpert-De Meyts E, et al. Natural history of seminiferous tubule degeneration in Klinefelter syndrome. Hum Reprod Update 2006; 12:39–48.[2]
- Wikstrom AM, Raivio T, Hadziselimovic F, et al. Klinefelter syndrome in adolescence: onset of puberty is associated with accelerated germ cell depletion. J Clin Endocrinol Metab 2004; 89:2263–2270
- Krausz C, Forti G. Sperm cryopreservation in male infertility due to genetic disorders. Cell Tissue Bank 2006; 7:105–112
- Price WH, Clayton JF, Wilson J, Collyer S, De May R. Causes of death in X chromatin positive males (Klinefelter’s syndrome). J Epidemiol Community Health 1985;39:330–6.
- Langlands AO, MacLean N, Kerr GR. Carcinoma of the male breast: report of a series of 88 cases. Clin Radiol1976;27:21–5.
- Engelberth O, Charvat J, Jezkova, Z, Raboch J. Autoantibodies in chromatin-positive men. Lancet 1966;2:1164–7
- Yencilek F, Baykal C: 46,XX male syndrome: a case report. Clin Exp Obst Gyn 2005, 32:263-264.


 R. VIGNESWARAN*
R. VIGNESWARAN*
 10.5281/zenodo.13854529
10.5281/zenodo.13854529