Abstract
The therapeutic advantages and potential side effects of beta-blockers, a family of drugs primarily used to treat cardiovascular problems, have been extensively researched. The goal of this review is to present a thorough analysis of the clinical uses, pharmacological mechanisms, and relative effectiveness of different beta-blockers. Their importance in managing arrhythmias, hypertension, heart failure, and post-myocardial infarction treatment is highlighted. The review also discusses the complexity of choosing a beta-blocker depending on patient-specific variables like pharmacokinetics and concomitant diseases. There is also a discussion of new research regarding the use of beta-blockers for non-cardiovascular diseases like anxiety and migraine prevention. The purpose of this study is to provide guidance for future research directions in the optimization of beta-blocker medication and to inform clinical practice by compiling existing research findings.
Keywords
beta blockers, Adernegenic, Metaprolol, Propranolol, Pharmacokinetics, Bioavailability, blood brain barrier
Introduction
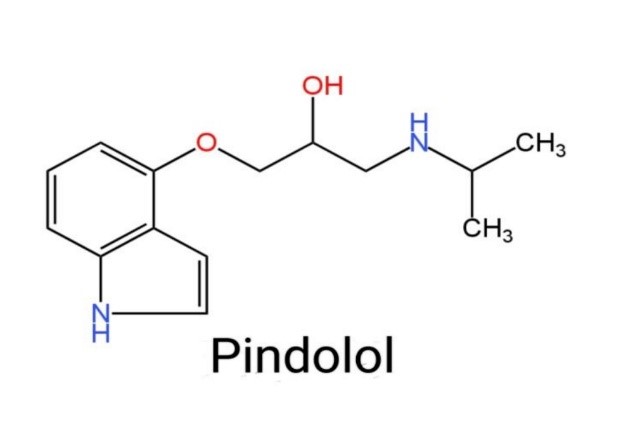
B- androgenic blockers are one of the most prescribed commonly as hypertension medications.[1] More than a dozen novel B-adernegenic blockers for the treatment of Hypertension have been Launched Since the availability of propranolol in 1976. Several beta-adrenergic blockers with different pharmacological qualities have been developed, which he may be grouped into three generations based on the differences in Pharmacological properties.[1] B-adrenergic blockers classification:- B-blockers differ in terms of B1/B2 – adernergic receptor Selectivity and Vasodilator activity, which has led to their classification as First, second, and third generation agents. First-generation B-blockers (propranolol, pindolol, etc.) are termed as non-selective because they exert equal blockade of B1- and B2 receptors. The second-generation beta-blockers (such as atenolol, metaprolol, bisoprolol, betaxolol, facebutolol, etc.), are referred to as selective because they have a higher. Affinity for B1-than B2-adernergic receptors. Finally, Vasodilatory properties distinguish third-generation B-blockers (labetalol, Carvedilol, nebivolol, etc.) from first – and second generation B-blockers. This class of B-blockers has varying selectivity for B1-receptors and acts as a vasodilator by blocking a1- adreno receptors and activating B3- aderenergic receptors. This class is the most effective for Lowering blood pressure.
Traditional B-blockers
The first B-blocker introduced into clinical practice was propranolol.[2]Synthesized by Sir James Black and colleagues, propranolol I was initially developed more than 50 years ago for the treatment of Angina.[2]However, its clinical utility was to some extent limited by it’s lack of B1- adernoceptor specificity; propranolol and the other traditional agents have equal affinities for blocking the B1 and B? receptors.[3] The development of Cardioselective B-blockers Such as atenolol, and metoprolol, which selectively block the B1compared with the B2 receptors[3], was therefore a significant therapeutic advance.
B-Adrenergic receptors (B-AR) and their associated Guanine nucleotide regulatory protein (G-protein/ adenylyl cyclase (AC) signal transduction pathways are central to the overall regulations of cardiac function. In particular, B-AR stimulation is a primary Control point for modulation of heart rate and myocardial contractility. However, B-AR signalling pathways undergo a number of adaptive and potential maladaptive regulatory changes as a consequence of heart failure.[4,5] This should not be surprising given that one of the best correlative makers for the degree and prognosis of chronic heart failure is plasma nor-epinephrine[6], an endogenous Ligand for adrenergic receptors.
B-adrenergic receptors and mechanism of action:-
B1 and B2 receptors are the most prevalent adrenergic receptor found in human Cardiovascular tissues.The heart and kidneys have most B1 -adrenergic receptions while the gastrointestinal tract liver, uterus ,vascular smooth muscle and skeletal muscle have B2- receptors.[7,8]The B1 and B2 receptor agonist, are individually linked to the activation of adenylyl cyclase and the production of cyclic adenosine monophosphate (c AMP) via, their interaction with the heterotrimeric G-protein Gs alpha. Adenylyl cyclase starts a c-AMP dependent pathway signalling Gs, which leads to potentiation of the receptor’s action.[9] Targeted stimulation of the B1receptor in the heart, increases heart rate and contractility (AV) nodal, and Ventricular muscle firing. The Stroke Volume and cardiac output will also increase as these two variables rise. Cardiac output is calculated as the sum of strike volume and heart rate. As stroke volume or heart rate rises as a result of targeted B1, receptor activation, Cardiac output will also increase and ultimately be responsible for the increasing perfusion to tissues throughout the body. The smooth muscle cells in the juxtaglomerular apparatus of the kidney contract and release renin due to B1 receptor activation. This effect will Ultimately raise blood volume due to the angiotensin-2 and aldosterone action.[10].

Fig 1:Beta adrenergic blocking drugs stopping the binding of the epinephrine with the receptors
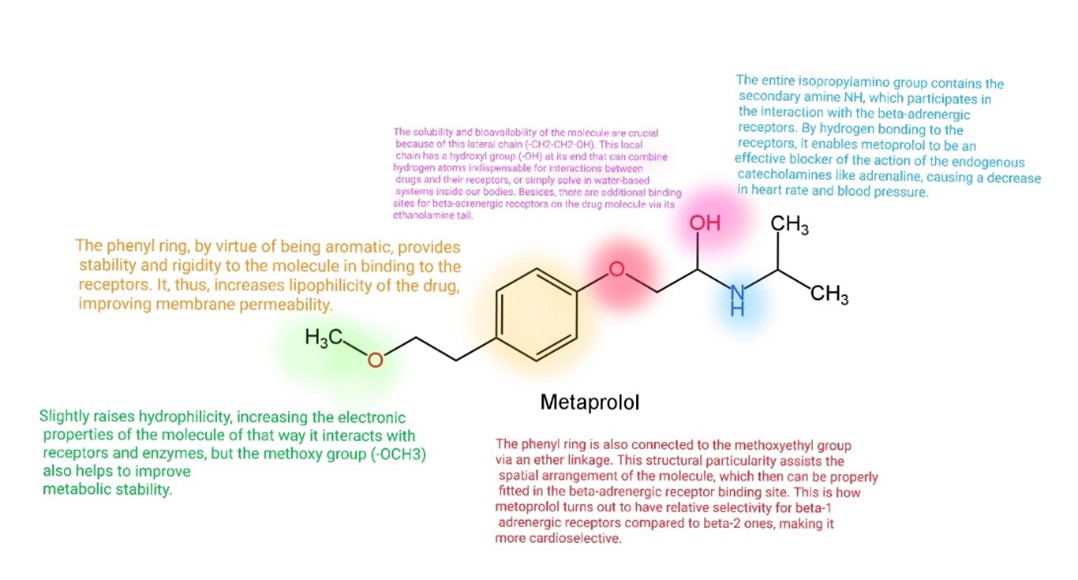
SAR (Structural Activity Relationship) of B (Beta) Aderenergic blockers.
Structure activity relationship of B-blockers is based on Adrenergic agonists because B-blockers have structural similarities as adrenergic agonists .The basic modifications in structure of adrenergic agonists to exert B-antagonist activity as follows:-
Fig 2 :Basic model of beta blockers
- Replacement of – OH’ group at R4 by – So? NH? or -CH?OH or other groups produce, antagonist, activity.
- Removal of -OH’ group at R3 also give antagonist activity
- The 2-Carbon chain is important for activity
- Addition of – OCH2 between side chain & aromatic ring also produce, better antagonist properties.
- The larger Aryl group at N-Shows, B-antagonist activity.
- Aromatic ring may be phenyl or heteroaromatic.
- Replacement of phenyl by naphthyl or substituted naphthyl produces non- selective B-blockers.
- Asymmetric (Chiral) Carbon is essential
- R-isopropyl, t-butyl, Aryl, alkyl increases polarity.
- X=H Called “Aryl ethanol amines, produces non- Selective blockers with ‘R’ configuration.
- X=-OCH Called ‘Aryl oxypropanolamines. Active in “s-configuration.
B-blockers are of two types of structure:-
Arylethanol amines:-
The first B-blocker was produced after changing groups of 3,4 hydroxy groups of Isoproterenol to dichloro groups, Dichloroisoproterenol. It is not true antagonist, so not used clinically now. Since DCI (Dichloroisoproterenol), a classic Bblocking agent, it also a partial B-agonist and it cannot be used as a hypotensive agent. DCI turned out to be Carcinogenic. Replacement of the electron rich hydroxyl grouped with an electron rich phenyl at 3,4 positions gives pronethalol, which it even better B-blocker than dichloroisoproterenol.
Aryloxypropanolamines :-
Pronethalol, an arylethanolamine, was withdrawn from clinical testing because of reports that it caused thymic tumors in mice. However, within two years of this report, Black and Co-workersdiscovered, a potent B-blocker propranolol, a close structural relative of pronethalol.
The three generations of beta blockers-
Table 1 : Advantages , disadvantages ,properties,Pharmacokinetics of the three generations of beta blockers

Three generations of beta blockers structures-

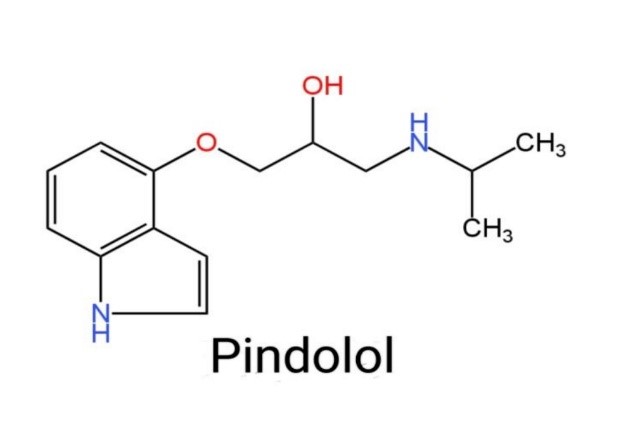
Fig 3: structure of propranlol and pindolol

Fig 4: structure of second generation beta blockers metaprolol, atenolol, acebutolol, celiprolol, betaxolol, bisprolol
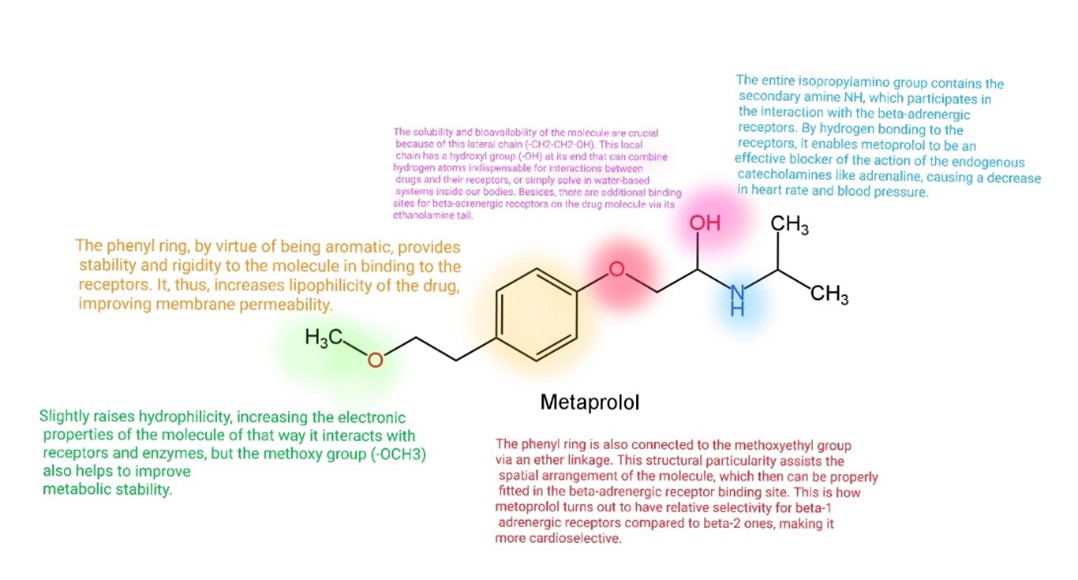
Fig 5:Activity of different groups in metaprolol
Third generation

Fig 6:Third generation beta blockers structures labetalol, nebivol, carvedilol

Fig 6: Functions of carvadiol
PHARMACOKINETIC BEHAVIOR
Administration
Beta-blockers are given orally, intravenously, or ophthalmically; it can also be injected intramuscularly.Dosages come in a variety of ranges depending on the medication involved. Outpatient prescriptions include once-a-day dosing, like some of the longer-acting beta-blockers such as metoprolol succinate. However, most beta blockers are typically dosed at least twice per day. Some beta-blockers have a half-life of approximately 4 hours, like propranolol, which is dosed up to 3 or 4 times a day depending on the indication and dose.[22]
Absorption-
Passive diffusion is typically used to absorb ?-blockers from the gastrointestinal tract. Their absorption is therefore not regarded as stereoselective.Nonetheless, certain ?-blockers that travel through intestinal secretion, such tanilolol, might be somewhat streoselective. However, the majority of ?-blockers do not have a stereoselective secretion mechanism.[18,19]
Distribution-
Since they are basic medications, ?-blockers can bind to plasma albumin and ?1-glycoprotein.Because the proteins are chiral, ?-blockers may bind to them in a stereoselective manner. If there is a higher free fraction of some ?-blockers in plasma, such as acebutolol, pindolol, and sotalol21–23, then the binding of these blockers to plasma proteins doesn't seem to be selective.The majority of the time, neither the tissue uptake itself nor the ?-blockers' binding to it is stereoselective. (R)-propranolol was shown to be more concentrated in the heart, muscles, and rat lungs as opposed to (S)-propranolol.24 One possible explanation for this apparent stereoselectivity could be a greater drug-free fraction of (S)-propranolol in the plasma. Similar to this, the main factor causing the stereoselective binding of propranolol enantiomers to plasma is an apparent stereo selective in the drug's RBC distribution. It has been observed that hydrophilicity and hydrophobicity demonstrate stereoselectivity during both release and storage from adrenergic nerve terminals. 25The effect of this stereoselectivity on the concentration of active enantiomers at the binding sites could have significant ramifications.[19].
The metabolic process
The majority of ?-blockers are eliminated either renal excretion of unaffected substances or hepatic metabolism. While more hydrophilic ?-blockers, such sotalol and atenolol, are removed without affecting urine quality, lipophilic ?-blockers, like propranolol, are mostly eliminated by metabolism. Stereoselectivity in the ?-blocker metabolism process is possible. The active enantiomer is rapidly eliminated while the inactive enantiomer accumulates and vice versa. Cytochrome P-450 complex can be inhibited or activated by ?-blocker enantiomers.Carvalho et al. reported that the concentrations of labetalol's (RR) and (SR) enantiomers in blood plasma were lower. Research conducted on individuals in good health revealed that metoprolol administration led to a greater concentration of the (R)-enantiomer than its antipode.[19,20]
Renal excretion
Changes in renal function can lead to the accumulation of both enantiomers of ?-blockers in the plasma, which are largely removed in their unaltered state. Renal excretion exhibits a marked stereoselectivity that favours (R)-metoprolol. Due to stereospecific clearance of the (S)-enantiomer in the urine, atenolol and pindolol showed a greater concentration of the less active (R)-enantiomer. Specifically, when compared to the (S)-enantiomer, the plasma concentration of (R)-pindolol is higher. In general, beta-blockers have variable pharmacokinetic properties. Absorption from the gastrointestinal tract leads to peak plasma concentration within 1-3 h. Propranolol is most extensively protein-bound, 93%, compared with timolol, 10%; metoprolol, 12%; nadolol, 25%; and atenolol, 3%. 13 This difference in its protein-binding property makes propranolol more likely to displace other protein-bound drugs effectively compared with other beta-blockers. In plasma, beta-blockers bind albumin and a?-acid glycoprotein. These two chemical forms of the drugs have bioavailabilities of 30% for propranolol, 50-75% for timolol, 50% for metoprolol, 20%-30% for nadolol, and 50% for atenolol.13 The reason for the low. 14 Beta-blockers' large volume of distribution ranges from 0.7 to 5.6 L/kg, suggesting physiochemical properties; that is, lipophilicity or hydrophilicity of drugs, which may influence the duration of ?-receptor blockade and, subsequently, tissue concentration because of extravascular penetration and diffusion across biologic barriers like the blood–brain barrier. 13 Discussion More specifically, the great distribution volume of beta-blockers is an indication of their lipophilic nature, which is the reason for their ability to penetrate tissues more readily, thus having a longer duration compared to those molecules with a lower volume of distribution, depending on the target. Beta-blockers can be found in the brain tissue despite potentially low cerebrospinal fluid concentration, thus an indication that beta-blockers cross the blood–brain barrier. Atenolol, metoprolol and propranolol are all present in very small amounts in breast milk. Nadolol is present to a greater extent and its use is therefore contraindicated during lactation.[19,21]
Pharmacological characteristics:-
The physlochemical properties of molecules are of significant importance for Therapeutic and side effects. Although beta blockers have similar Pharmacotherapeutics effects, they may have different pharmacokinetic properties gastrointestinal absorption rate, first pass effect, lipid solubility hepatic biotransformation sate, the pharmacological activity of metabolites and clearance sate. According to thean properties, beta blockers are divided into two major groups-agents eliminated from the body by hepatic metabolism and those excreted unchanged by the kidneys. First class beta blackens, such as propransit Or metoprolol, are almost completely absorbed in the small intestine, metabolized by the liver, and have a high solubility in lipids. In Contrast, beta-blockers in the other category, such as atenolol Or sotalol, are less or all soluble in lipiis, incompletely absorbed and excreated unchanged by the kidney.Schematic representation of the difference between lipophilic and hydrophic beta-blockers: chemical formula, partition coefficient (log P), physical properties, and permeability through a biological membrane.
The metabolic problem
Effects on glucose metabolism-
In this respect, the diabetogenic effect of non-selective beta-blockage results from a decrease in pancreatic insulin secretion and decreased insulin sensitivity secondary to a reduced peripheral blood supply, increased body weight, and increased gluconeogenesis through glycogenolysis secondary to unopposed alfa 2 activity. The term “new onset diabetes” is vaguely defined and, in many cases, not defined at all by the authors. A large meta-analysis investigated the prevalence of NOD in a hypertensive population treated with BBL and found that the investigated BBL was either not or only moderately selective. Beta-block- age resulted in an approximately 30% increased risk of NOD compared to placebo and a 20% increased risk compared to CCB and RAAS-i. When comparing BBL to thiazide diuretics, data are less uniform, reporting neutral17.18 to less diabetogenic effects 16 of BBL, Data concerning diabetogenic effects of non-thiazide diuretics are lacking. The diabetogenic profile of BBL does not represent a class effect. Receptor selectivity is important with decreasing negative metabolic impact with increasing Bl-selectivtiy20. BBL with vasodilating activity also show little or no metabolic side effects. There is no concordance regarding the implications of antihypertensive therapy-induced diabetes on major endpoints. The negative effect of hyper-glycaemia on cardiovascular end points could be balanced at least in part by the antihypertensive action of the treatment, also assuming general negative prognostic significance of new diabetes in patients with hypertension under treatment .[16]
Lipid metabolism
First- and second-generation BBL are considered “atherogenic” because they exert an unfavourable effect on the distribution of the different subgroups. Of lipids (reducing HDL, increasing LDL and triglyceride). The lipase responsible for degraded triglycerides is inhibited by unopposed A-AR stimulation in beta-blockade. HDL-lowering possibly is ISA-dependent 13, Third-generation BBL exert a neutral or positive effect on the lipid profile. Data concerning impact on outcome are lacking.[16,17]
Contraindications-
Traditionally, beta-blockers have been absolutely contraindicated in asthmatic patients. More recently, societies have come into agreement that cardio-selective beta-blockers, also referred to as beta-1 selective, are permissible in asthmatics but non-selective betablockers are not. Non-selective beta-blockers should not be used in patients with asthma.Those patients who have either acute or chronic bradycardia and/or hypotension have relative contraindications to beta-blocker usage.Certain beta-blockers are contraindicated in patients with a history of specific medical conditions. The drug sotalol should not be used in patients with a diagnosis of long QT syndrome or who have had torsades de pointes in the past. Beta-blockers are relatively contraindicated in patients with Raynaud’s phenomenon since the medication will exacerbate this condition.[22]
Toxicity
The antidote overdose for beta-blockers is glucagon. It is particularly useful for cardiotoxicity that is induced by beta-blockers. Cardiac pacing is a second line when glucagon may fail, and this may comprise of either transcutaneous or transvenous pacing.[22].
CNS– Related Side Effects with beta blockers (Metoprolol ,Atenolol, Propranolol).
Central nervous system (CNS) side effects of beta blockers include Vivid and bizarre dreams, hallucinations, Disturbance of sleep and mood, and paranoid psychosis (Fraser and Carr 1976;Fleminger 1978).CNS side –Effects depend on several factors, notably the degree of lipophilicity and protein binding. Highly lipophilic Drugs such as propranolol and pindolol readily penetrate brain tissue, whereas water -soluble agents such as Atenolol do not (cruick-Shank 1980).No Significant CNS side effects were reported with atenolol, but Of metoprolol caused a significant increase in the incidence of Sleep disturbance (p<0>
Lipophillic property
The lipophilic property of some beta-blockers is the ability of the drug to diffuse through the blood-brain. barrier. First, the agent must cross it and attach directly to the beta-adrenergic receptors, the suppression of which it medates, flecond, the drug must also interact with non-adrenergic receptors, blocking their signals or destabilizing the call membrane. Highly lipophilic beta blockers such as propranolol, diffuse rapidly through the brain tissues compared to hydrophilic beta blockers, such as atenolol, which lacks the property.

Fig 7: Propraponal and Atenolol Lipophillic and hydrophobic properties
Beta-blockers and heart failure
Pathophysiology- Myocardial systolic dysfunction is associated with neurohumoral hyperactivity (sympa- thetic nerve system and renin-angiotensine-aldosteron system RAAS amongst others). Although benefi- cial in the early stages of heart failure, by contributing to preservation of inotropy, eventually this results in negative cardiac remod- elling and progression of heart failure. In heart failure increased serum concentrations. In this setting, norepinephrine, angiotensin II, aldosterone, endothelins, vasopressin, and cytokines are increased and exert negative interactions on cardiac structure and function. In the setting of sympathetic hyperactivity, protecting adaptation by downregulation of B1-AR has been described. The role of B2-and B3-AR in heart failure is not so clear. There is no down regulation of B2-AR, with possible antiapoptotic mechanisms attributed to these receptors. Whether or not heart rate lowering per se, besides sympathetic tone reduction, is important is unknown. Temporal course of changes in myocardial structure and function following the initiation of BBL was studied in 26 patients with dilated cardiomyopathy treated with RAAS- Initial titrated initiation of treatment with metoprolol leads to a reduction of the left ventricular ejection fraction and a rise in left ventricular end systolic volume. These variables improved from a duration of therapy of one month and three months onwards respectively. After 18 months, reduced ventricular mass and improved geometry was reported. Next to neurohumoral effects of BBL in heart failure, antiischaemic properties are also to be considered.
Monitoring
Monitoring of pulse and blood pressure is required during treatment with the beta-blockers. With sotalol, the practitioner must monitor QTc interval as sotalol has an impact on QT prolongation. Fatigue and weight gain are other side effects faced due to outpatient beta blocker therapy.[12].
Beta blockers in other diseases-
Migraine
Beta blockers, like propranolol, metoprolol and timolol, have been proven to be effective in preventing migraines. Propranolol especially has been extensively researched and was shown to significantly reduce the frequency of episodic migraines compared with placebo .Studies have suggested that it may decrease the number of headaches by about 1.5 per month, as well as being more likely to lower headache severity and duration . Metoprolol and other beta-blockers also possess similar advantages though some data in favour of some of these drugs is not that strong .Furthermore, beta-blockers are being used to manage anxiety and stress conditions which are common triggers for migraines. These medications thus act by attenuating adrenaline effects hence relieving physical symptoms prompted by anxiety which makes them a dual-purpose therapy for patients suffering from both these conditions concurrently .Although useful for these non-cardiovascular indications, beta-blockers are not appropriate for everyone. Therefore, those having asthma or diabetes or suffering from low BP or certain heart disorders should refrain from using them because they could have unwanted side effects .For more detailed information on effectiveness of beta-blockers in preventing migraine attacks and their wide use particularly in controlling anxiety among other illnesses.[23,24].
Arrhythmia Management
Arrhythmias, or irregular heartbeats, can range from being harmless to life-threatening. Beta blockers are very effective in treating supraventricular tachycardias (SVTs) like atrial fibrillation and atrial flutter. They help control the heart rate and restore normal rhythm by slowing the conduction through the AV node of the electrical impulse. The ability to reduce automaticity of the sinus node and decrease sympathetic nervous system activity also makes them a cornerstone in arrhythmia management.[25].
Controlling Hypertension
High blood pressure (hypertension) is a major risk factor for cardiovascular diseases such as stroke, heart attack, and heart failure. Beta blockers lower blood pressure by reducing the force of heart contractions and decreasing the heart rate. They also prevent renin secretion from kidneys that is vital for regulation of blood pressure. Although beta blockers are not usually preferred as first-line antihypertensive drugs other classes of antihypertensive drugs are often used, they are especially useful in patients with co-morbidities such as angina or history of MI.[26,27].
Myocardial Infraction:-
The AHA recommends that oral beta blockers therapy be initiated in all patients without contraindications within 24 hours after an myocardial infraction. Bisoprolol (Zebeta), Carvedilol (Coreg) and metoprolol have exhibited a mortality benefit in patients with a reduced LVEF (left ventricular ejection fraction) after an MI. Renin angiotensin- aldesterone system Inhibitors; and angiotensin receptors blockers, angiotensin converting enzyme (ACE) Inhibitors are strongly recommended after an MI in patients with hypertension, diabetes mellitus, an LVEF of 40% or less or chronic kidney disease. Statin therapy ;- role of statins in reducing mortality and ACS in patients with cardiovascular disease.
Heart failure -
Reducing the activation of angiotensin converting enzymeReducing the activation of angiotensin converting enzyme (ACE), by using the ACE inhibitors has been mainstay of heart failure, and using the beta blockers is to be contraindicated in heart failure. The traditional approach to management of heart failure with reduced LVEF is to start with an ACE inhibitors and then to add a beta- blockers. Both ACE inhibitors and angiotensin receptors beta blockers reduce mortality in heart failure.
Arrhythmias:-
A Beta-blockers (propranolol) in combination with Diltiazem should be taken into account in acute management of atrioventricular nodal reentry tachycardia (AVNRT). The AVNRT, leads to cause termination of arrhythmia. Beta-blockers were the most effective in ensuring adequate heart rhythm control in patients with AF( atrial fibrilation) . Furthermore, beta-blockers are anti-ischemic and reduce the mortality by approximately 35%.beta blockers are the first line treatment in management of VA and preventing SCD.
Hypertension-
Beta blockers are the first line treatment for treating cardiac problems, hypertension (high blood pressure), reduced by using beta-blockers i. e Atenolol, metoprolol, by either selective or non selective receptor mechanism.
CONCLUSION:
Numerous trails have shown the efficacy of using betablockers. The SAR reveals the benefits and limitations of betablockers. However utilising betablockers has been associated with some adverse effects. Future research must get past these.
REFERENCE :
- Larochelle P, Tobe SW, Lacourciere Y. Beta blockers in hypertension: Studies and meta-analyses over the years. Can J Cardiol.2014;30(5):16-22. doi:10.1016/j.cjca.2014.02.012.
- Hollenberg NK. The role of beta blockers as a cornerstone of cardiovascular therapy. Am J Hypertens. 2005;18(Suppl 1):165S-168S.
- Bristow MR. Beta-adrenergic receptors blockade in chronic heart failure. Circulation. 2000;101:558-569.
- Bristow MR, Ginsburg R, Umans V, et al. Beta 1- and beta 2-adrenergic receptor sub-populations in non-failing and failing human ventricular myocardium: Coupling of both receptor subtypes to muscle contraction and selective beta 1 receptor down-regulation in heart failure. Circ Res. 1986;59:297-309.
- Bristow MR, Hershberger RE, Port JD, Minobe W, Rasmussen R. Beta 1- and beta 2-adrenergic receptors mediated adenylate cyclase stimulation in non-failing and failing human ventricular myocardium. Mol Pharmacol. 1989;35:295-303.
- Cohn JN, Levine TB, Olivari MT, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311:819-823.
- Wiysonge CS, Volmink J, Opie LH. Beta-blockers and the treatment of hypertension: It is time to move on. Cardiovasc J Afr. 2007;18(6):351-352.
- Weber MA. The role of the new beta-blockers in treating cardiovascular disease. Am J Hypertens. 2005;18(1):169-176. doi:10.1016/j.amjhyper.2005.09.009.
- do Vale GT, Ceron CS, Gonzaga NA, Simplicio JA, Padovan JC. Three generations of beta-blockers: History, class differences, and clinical applicability. Curr Hypertens Rev. 2019;15(1):22-31. doi:10.2174/1573402114666180918102735.
- Reiter MJ. Cardiovascular drug class: Beta-blockers. Prog Cardiovasc Dis. 2004;47(1):11-33. doi:10.1016/j.pcad.2004.04.004.
- Stoschitzky K. Individual beta-blockers for individual patients. E-Journal of the ESC Council for Cardiology Practice. 2008;6(19).
- Golightly LK. Pindolol: A review of its pharmacology, pharmacokinetics, clinical uses, and adverse effects. Pharm D. 1982.
- Springer J, Jové Q, de Lima Junior EA, et al. Effects of S-pindolol in mouse pancreatic and lung cancer cachexia models. J Cachexia Sarcopenia Muscle. 2023. doi:10.1002/jcsm.13249.
- Artigas F, Celada P, Laruelle M, Adell A. How does pindolol improve antidepressant action? Trends Pharmacol Sci. 2001;22(5):224-229. doi:10.1016/S0165-6147(00)01682-5.
- Gorre F, Vandekerckhove H. Beta-blockers: Focus on mechanism of action. Which beta-blocker, when and why? Acta Cardiol. 2010;65(5):565-570. doi:10.1080/AC.65.5.2056244.
- Gilles TD. Antihypertensive therapy and cardiovascular risk: Are all antihypertensives equal? Hypertension. 1992;19(S1):124-129.
- Wetterich U, Spahn-Langguth H, Mutschler E, Ter-haag B, Rosch W, Langguth P. Stereochemical facets of clinical beta-blockers: An overview. Pharm P Resume. 1996;13:514.
- Vashistha VK, Kumar A. Stereochemical facets of clinical ?-blockers: An overview. Pharmacol Rev. 2020.
- Carvalho TM, Cavalli RC, Marques MP, Da Cunha SP, Baraldi CO, Lanchote VL. Chirality. J Pharm Biomed Anal. 2009;21:738.
- Yan H, Levander T. Stereochemical aspects of beta-blocker action. Eur Neuropsychopharmacol. 1999;10:59.
- Farzam K, Jan A. Beta-blockers. StatPearls. 2023 Aug 22.
- Bousnina S, Hammi A. Physicochemical characterization of metoprolol tartrate loaded by hydroxypropyl cellulose microparticles used for drug delivery systems. Drug Deliv. 2024 Jun 23.
- Liu Z, Wu C, Song D, Wang L, Li J, Wang C, Guo L. Atenolol vs. propranolol for the treatment of infantile hemangiomas: A systematic review and meta-analysis. J Clin Med. 2020 Jun 5.
- Armstrong C, Kapolowicz MR. A preliminary investigation on the effects of atenolol for treating symptoms of anxiety. Mil Med. 2020;185(11-12):e1954-e1960. doi:10.1093/milmed/usaa170.
- Khan Z, Demirta? E, K?ro?lu O, Karata? Y. Beta-adrenergic blockers’ supportive and adverse role in hypertension: A review of three generations. Pak J Med Dent. 2022;11(1). doi:10.36283/PJMD11-1/011.
- Fisker FY, Grimm D, Wehland M. Third-generation beta-adrenoceptor antagonists in the treatment of hypertension and heart failure. Pharmacol Rev. 2015;72(1):123-145.
- Third-Generation Beta-Adrenoceptor Antagonists in the Treatment of Hypertension and Heart Failure Filip Y. Fisker, Daniela Grimm, Markus Wehland First published: 03 March 2015


 KONATHAM PRANUSHA*
KONATHAM PRANUSHA*
 KONATHAM PRANUSHA
KONATHAM PRANUSHA
 KUSAMPUDI PREETHI ALEKHYA
KUSAMPUDI PREETHI ALEKHYA
 N.HARMYA
N.HARMYA
 P.BANDESWARAO
P.BANDESWARAO






 10.5281/zenodo.13863332
10.5281/zenodo.13863332