Abstract
Over the past three decades, formulation technology has significantly advanced, particularly in drug delivery systems. Innovations include novel dosage forms and new uses for existing drugs, offering benefits like improved patient compliance, sustained drug concentration, reduced dosing frequency, targeted delivery, and minimized side effects. Transdermal drug delivery systems (TDDS) are key developments, allowing controlled, continuous medication administration through the skin, bypassing gastrointestinal degradation and hepatic first-pass metabolism, and enhancing bioavailability and patient compliance. The FDA approves roughly one transdermal product every 2.2 years, with the first patch approved four decades ago. This research examines the skin's role as a barrier, clinical trials, patents, commercialization, and the benefits and limitations of TDDS. Various TDDS methods are reviewed, highlighting their advantages, disadvantages, and potential applications. Recent advancements demonstrate TDDS's effectiveness and potential across diverse sectors, emphasizing their transformative impact on drug delivery and therapeutic practices.
Keywords
Transdermal drug delivery systems, Anatomy of skin, Improvement of transdermal administration, Drug delivery systems n
Introduction
A medical survey is a research method used to gather information, data, or opinions from individuals or groups related to various aspects of healthcare, medicine, or medical treatments. These surveys are conducted to understand patterns, trends, preferences, behaviors, or outcomes within the medical field. Medical surveys can cover a wide range of topics, including but not limited to patient satisfaction, treatment effectiveness, medication adherence, healthcare provider practices, disease prevalence, and public health concerns. They are typically designed with specific objectives in mind and employ various techniques such as questionnaires, interviews, or observational studies to collect data. The findings from medical surveys can inform healthcare decision-making, policy development, medical research, and the improvement of healthcare services. According to the World Health Organization report, hypertension is the most common cardiovascular condition in the world and there are about 600 million people at risk for heart attack, stroke and cardiac failure.1,2,3
HYPERTENTION:
High blood pressure (HBP or hypertension) is when your blood pressure, the force of your blood pushing against the walls of your blood vessels, is consistently too high. The blood pressure normal level is below 120/80, where 120 systolic measurement (peak pressure in the arteries) and 80 diastolic measurements (minimum pressure in the arteries). Blood pressure called prehypertension is between 120/80 and 139/89 (to denote increased risk of hypertension), and hypertension 140/90 or above.3
ANTIHYPERTENSIVE:4,5
Antihypertensive drugs are a class of drugs that are used to treat hypertension (high blood pressure)
Hypertension is a primary risk factor for cardiovascular disease, including heart attack, stroke, aneurysm, heart failure and myocardial infarction. Keeping blood pressure under control is important for health preserving and reducing the risk of these dangerous conditions. Evidence suggests that reduction of the blood pressure by 5mmHg can decrease by 34% of the risk of stroke, 21% ischemic heart disease and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.
ANTIHYPERTENSIVE DRUGS: CLASSIFICATION:6,7,8,9,10
Antihypertensive drugs are thiazide diuretics, calcium channel blockers, ACE inhibitors, Angiotensin II receptor antagonists (ARBs), Adrenergic receptor antagonist and vasodilator etc. Therefore, this study was carried out to find the current prescribing pattern of antihypertensive drugs and efficacy of these drugs in maintaining adequate blood pressure control in hypertensive patients in Jewelweed region. Hypertension affects more than 1.28 billion people aged 30–79 years worldwide; a number which has doubled since 1990. The risk factors for hypertension are; family history, age over 65 years, diabetes or kidney disease, unhealthy eating habits, physical inactivity, overweight, smoking, and alcohol consumption In 2011, the health care system in Greenland initiated a lifestyle initiative focusing on quality of care among patients with hypertension, diabetes, and chronic obstructive pulmonary disease (COPD)
what is mean by medical survey?11,12
A medical survey refers to a systematic method of collecting information or data related to medical or healthcare-related topics. These surveys are typically conducted to gather insights into various aspects of healthcare, including patient experiences, treatment effectiveness, healthcare provider practices, disease prevalence, public health concerns, and more. Medical surveys can take different forms, such as questionnaires, interviews, observational studies, or clinical trials, and they are often used to assess trends, attitudes, behaviors, or outcomes within the medical field. The data obtained from medical surveys can be analyzed to inform healthcare policies, improve healthcare services, guide medical research, and enhance patient care.
A medical survey is a systematic collection and analysis of health-related data from a specific group of people. These surveys are conducted to gather information on various aspects of health, such as the prevalence of diseases, health behaviors, and access to healthcare services. The goal is to gain insights that can inform public health policies, improve healthcare services, and guide medical research
Purpose of Medical Surveys:13,14
Medical surveys serve several important purposes:
- Epidemiology:
By collecting data on disease prevalence and incidence, medical surveys help identify health trends and patterns. This information is crucial for understanding the distribution of diseases within a population and identifying risk factors.
- Healthcare Planning:
Data from medical surveys inform healthcare planning and resource allocation. For example, if a survey reveals a high prevalence of diabetes in a community, healthcare providers can prioritize diabetes education, screening, and treatment programs.
- Policy Making:
Policymakers use medical survey data to develop and implement public health policies. For instance, if a survey indicates a rise in smoking rates, policies aimed at reducing tobacco use can be put in place.
- Research:
Medical surveys provide valuable data for researchers studying various health issues. This data can lead to new discoveries and advancements in medical science
- Monitoring and Evaluation:
Surveys help monitor the effectiveness of public health interventions and programs. By comparing data over time, health officials can assess whether a particular intervention is working or needs adjustment.
ANTIHYPERTENSION:
Antihypertension refers to the treatment or management of hypertension, commonly known as high blood pressure. Antihypertensive medications are drugs or therapies specifically designed to lower blood pressure and reduce the risk of associated cardiovascular complications such as heart attack, stroke, and kidney disease. These medications work through various mechanisms to relax blood vessels, decrease fluid volume, or reduce the force of the heart's pumping action. Common classes of antihypertensive medications include diuretics, beta-blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and others. Antihypertensive treatment often involves a combination of lifestyle modifications (such as dietary changes and exercise) along with pharmacotherapy tailored to individual patient needs. The goal of antihypertensive therapy is to achieve and maintain blood pressure within a healthy range to reduce the risk of cardiovascular events and improve overall health outcomes. Antihypertensive medications are drugs used to treat high blood pressure, also known as hypertension. They work by helping to lower blood pressure, reducing the strain on the heart and blood vessels. There are several classes of antihypertensive drugs, each with different mechanisms of action. Some common types include:
- Diuretics:
These medications help the body get rid of excess sodium and water, reducing blood volume and thus lowering blood pressure. Examples include hydrochlorothiazide and furosemide.
- ACE Inhibitors:
ngiotensin-converting enzyme (ACE) inhibitors block the production of a hormone that narrows blood vessels, leading to relaxation of blood vessels and lower blood pressure. Examples include enalapril and lisinopril.
- ARBs (Angiotensin II Receptor Blockers):
These drugs block the action of a hormone that causes blood vessels to narrow, leading to relaxation of blood vessels and decreased blood pressure. Examples include losartan and valsartan.
- Beta-Blockers:
Beta-blockers reduce the heart rate and the heart's output of blood, which lowers blood pressure. Examples include metoprolol and atenolol.
- Calcium Channel Blockers:
These medications prevent calcium from entering the heart and blood vessel cells, causing the blood vessels to relax and widen, lowering blood pressure. Examples include amlodipine and diltiazem.
- Alpha-Blockers:
Alpha-blockers reduce nerve impulses that tighten blood vessels, allowing blood to flow more freely. Examples include doxazosin and prazosin.
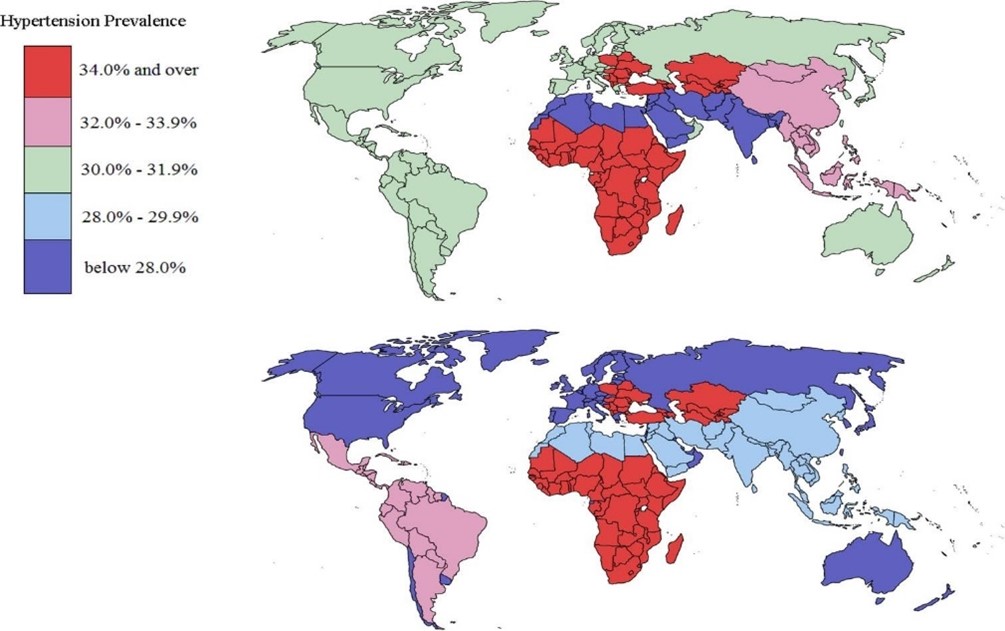
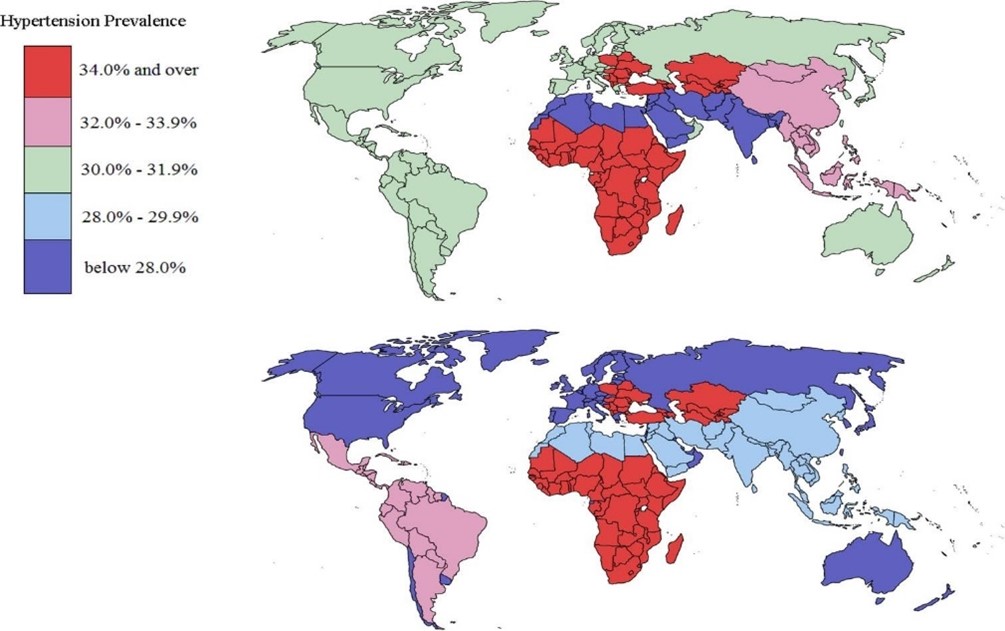
worldwide problem of hypertension:
Hypertension, or high blood pressure, is a significant global health issue affecting people of all ages, ethnicities, and socioeconomic backgrounds. Here are some key points highlighting the worldwide problem of hypertension:
- Prevalence:
Hypertension is widespread, affecting millions of people worldwide. According to the World Health Organization (WHO), around 1.13 billion people globally have hypertension.
- Impact on Health:
Hypertension is a major risk factor for various cardiovascular diseases, including heart disease, stroke, and kidney disease. It can also contribute to other health problems such as vision loss, cognitive decline, and peripheral artery disease.
- Global Burden of Disease:
Hypertension is one of the leading causes of premature death and disability worldwide. It is responsible for a significant proportion of the global burden of disease and is associated with substantial healthcare costs.
- Risk Factors:
Several factors contribute to the development of hypertension, including unhealthy diets high in salt and low in fruits and vegetables, lack of physical activity, obesity, tobacco use, excessive alcohol consumption, and genetic predisposition.
- Challenges in Detection and Treatment:
Many people with hypertension are unaware of their condition because it often presents with no symptoms. Even when diagnosed, hypertension management can be challenging due to factors such as medication adherence, access to healthcare services, and lifestyle modifications.
- Health Inequalities:
Hypertension disproportionately affects certain populations, including older adults, people with lower socioeconomic status, and certain ethnic groups. Disparities in healthcare access and quality contribute to these inequalities.
- Global Initiatives:
Various global initiatives, led by organizations like the WHO, aim to address the burden of hypertension through awareness campaigns, promotion of healthy lifestyles, strengthening health systems, and improving access to affordable and effective antihypertensive treatments.
- Lifestyle Changes:
Lifestyle modifications such as adopting a healthy diet, engaging in regular physical activity maintaining a healthy weight, reducing salt intake, limiting alcohol consumption, and avoiding tobacco use are key strategies in preventing and managing hypertension.
- Pharmacological Interventions:
Antihypertensive medications play a crucial role in managing hypertension and reducing the risk of associated complications. However, challenges such as medication adherence, side effects, and access to affordable medications remain. As of my last update in January 2022, global statistics on the prevalence of hypertension and the ratio of individuals receiving antihypertensive treatment may vary by region and country. However, I can provide some general insights:
worldwide antihypertension ratio:
- Prevalence of Hypertension:
Hypertension is a widespread health issue globally, affecting millions of people of all ages. According to the World Health Organization (WHO), around 1.13 billion people worldwide have hypertension. The prevalence varies across regions, with higher rates observed in low- and middle-income countries.
- Treatment Rates:
While the exact ratio of individuals receiving antihypertensive treatment worldwide is not readily available, it's important to note that there are significant gaps in hypertension detection, treatment, and control, particularly in low- and middle-income countries. Many people with hypertension are either undiagnosed or inadequately treated.
- Disparities:
Access to healthcare services, affordability of medications, and awareness of hypertension contribute to disparities in treatment rates. In many countries, certain populations, such as older adults, individuals with lower socioeconomic status, and rural communities, may have limited access to healthcare resources, leading to lower treatment rates.
- Global Initiatives:
Various global initiatives, led by organizations like the WHO and other health agencies, aim to improve hypertension detection, treatment, and control worldwide. These initiatives focus on raising awareness, strengthening health systems, promoting healthy lifestyles, and improving access to affordable medications.
- Pharmacological Treatment:
Antihypertensive medications are a cornerstone of hypertension management. Common classes of medications include diuretics, beta-blockers, calcium channel blockers,angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor blockers (ARBs). However, adherence to medication regimens can be challenging, and factors such as cost, side effects, and healthcare access can affect treatment rates.
- Lifestyle Modifications:
Lifestyle changes, including adopting a healthy diet, engaging in regular physical activity, maintaining a healthy weight, reducing salt intake, limiting alcohol consumption, and avoiding tobacco use, are essential components of hypertension management and can complement pharmacological treatment.
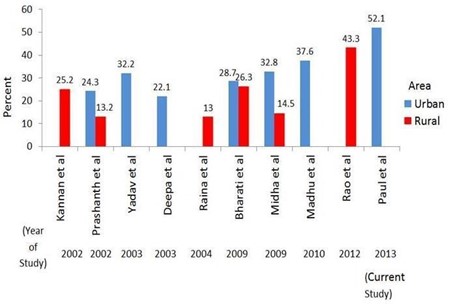
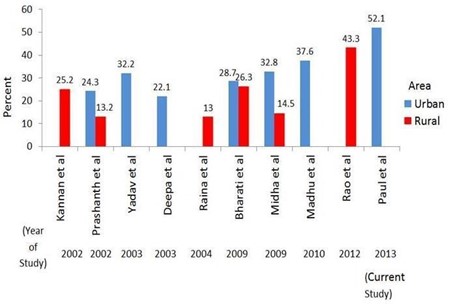
ANTIHYPERTENSION PROBLEM IN INDIA:
Hypertension, or high blood pressure, is a significant health issue in India, with a considerable portion of the population affected by this condition. Here are some key points regarding the antihypertension problem in India:
- Prevalence:
Hypertension prevalence in India has been steadily increasing over the years, fueled by urbanization, sedentary lifestyles, dietary changes, and aging population. According to various studies, the prevalence of hypertension in India varies across different regions and demographic groups, but overall estimates suggest that around 25-30% of adults in India have hypertension.
- Awareness and Diagnosis:
One of the challenges in addressing hypertension in India is low awareness and underdiagnosis. Many individuals with hypertension are unaware of their condition due to the asymptomatic nature of the disease. Lack of routine blood pressure screenings and limited access to healthcare services in rural areas contribute to underdiagnosis.
- Treatment Gaps:
Even among those diagnosed with hypertension, there are significant treatment gaps in India. Access to affordable healthcare services and medications remains a challenge, particularly in rural and underserved areas. Additionally, adherence to treatment regimens can be an issue due to factors such as cost, side effects, and lack of awareness about the importance of long-term management.
- Risk Factors:
Several risk factors contribute to the high prevalence of hypertension in India, including unhealthy diets high in salt and fats, low levels of physical activity, tobacco use, alcohol consumption, obesity, stress, and genetic predisposition. Urbanization and rapid socioeconomic changes have also led to lifestyle modifications that increase the risk of hypertension.
- Health Impact:
Hypertension is a major risk factor for cardiovascular diseases, including heart attacks, strokes, and kidney disease. It contributes significantly to the burden of non-communicable diseases (NCDs) in India and poses a substantial economic burden on individuals, families, and the healthcare system.
- Government Initiatives:
The Indian government has recognized the growing burden of NCDs, including hypertension, and has initiated various programs and policies to address this issue. These efforts include the National Programmed for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS), which aims to promote health education, early detection, and treatment of NCDs, including hypertension.
- Community Interventions:
Non-governmental organizations (NGOs) and community health workers also play a vital role in raising awareness about hypertension, promoting healthy lifestyle behaviors, conducting screenings, and facilitating access to healthcare services in remote and underserved areas.As of my last update in January 2022, specific data on the ratio of individuals receiving antihypertensive treatment in India may vary depending on the source and the timeframe of the study. However, I can provide some general insights into the status of hypertension treatment in India:
Antihypertensive ratio in India:
- Treatment Coverage:
Despite the high prevalence of hypertension in India, there are significant gaps in treatment coverage. Many individuals with hypertension remain undiagnosed, and even among those diagnosed, a substantial proportion may not receive appropriate treatment or achieve adequate blood pressure control.
- Healthcare Access:
Access to healthcare services and medications can be challenging for a significant portion of the Indian population, particularly in rural and underserved areas. Factors such as affordability, availability of healthcare facilities, and awareness about hypertension management play a crucial role in determining treatment coverage.
- Government Programs:
The Indian government has implemented various health programs and initiatives aimed at addressing non-communicable diseases (NCDs), including hypertension. These programs often focus on improving access to healthcare services, promoting awareness about NCDs, and providing affordable treatment options.
- Community Interventions:
Non-governmental organizations (NGOs) and community health workers play a vital role in raising awareness about hypertension, conducting screenings, and facilitating access to treatment in remote and underserved areas where healthcare infrastructure is limited.
- Challenges in Treatment:
Challenges such as medication adherence, lifestyle modifications, and addressing underlying risk factors contribute to the complexity of hypertension management in India. Efforts to improve treatment coverage require a comprehensive approach that addresses these challenges at both individual and population levels.
Survey procedure:
Conducting a medical survey focused on antihypertension involves a systematic approach tailored to understanding the prevalence, management, and impact of hypertension and its treatments. The procedure begins with clearly defining the objectives of the survey, which may include assessing the prevalence of hypertension, evaluating awareness and adherence to antihypertensive medications, identifying barriers to treatment, or assessing the effectiveness of current treatment strategies. Once the objectives are established, the survey instrument, such as a questionnaire or interview protocol, is developed to collect relevant data. This entails selecting appropriate questions related to hypertension diagnosis, treatment history, medication adherence, lifestyle factors, and barriers to care. The survey methodology is then determined, including sampling techniques and data collection methods. Depending on the target population and research objectives, sampling methods such as random sampling, stratified sampling, or convenience sampling may be employed. Data collection methods may include face-to-face interviews, telephone interviews, online surveys, or mailed questionnaires, chosen to maximize participation and data quality. Prior to conducting the main survey, the survey instrument is often pilot-tested with a small sample to identify any issues with clarity, comprehensiveness, or relevance. Feedback from pilot testing is used to refine the survey instrument before full-scale implementation. Once the survey is administered to the target population, data collection proceeds according to the predetermined methodology. This may involve contacting participants, administering the survey instrument, and collecting responses. Attention is paid to maintaining confidentiality, obtaining informed consent, and ensuring data accuracy throughout the process. After data collection, the collected data is cleaned, coded, and analyzed using appropriate statistical methods. Analysis may involve examining descriptive statistics, prevalence rates, treatment patterns, associations between variables, or factors influencing medication adherence. The results are interpreted in light of the research objectives and existing literature on hypertension management.
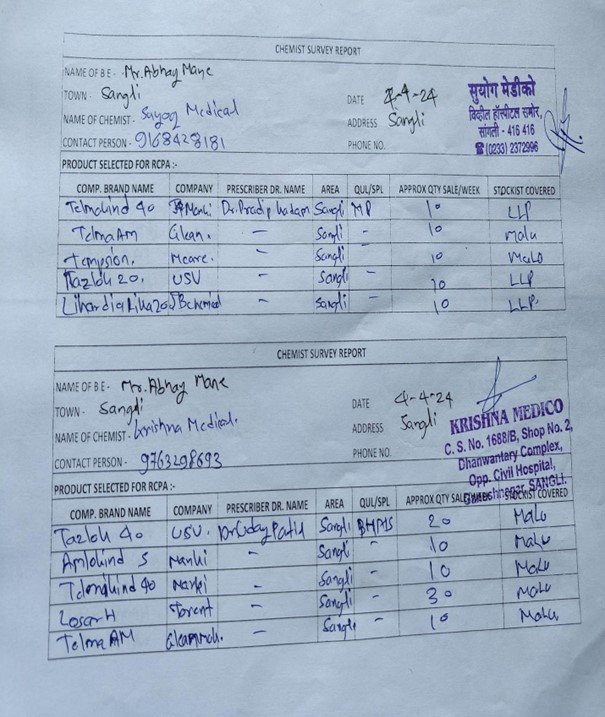
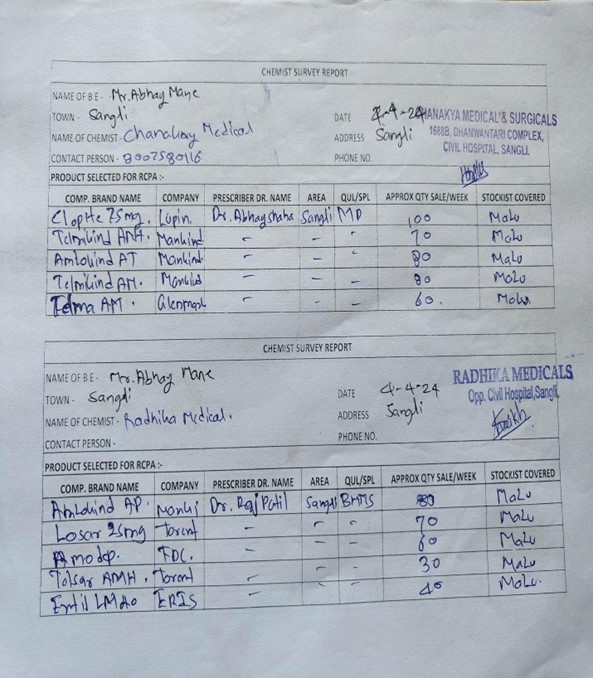
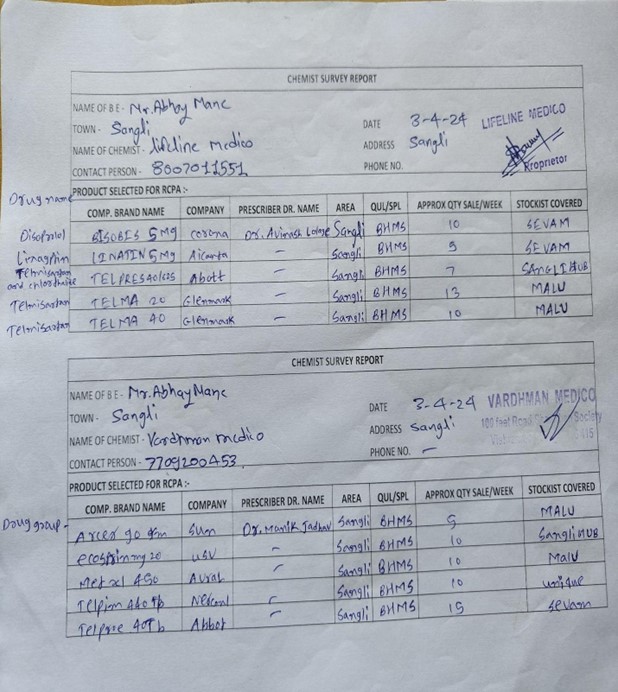
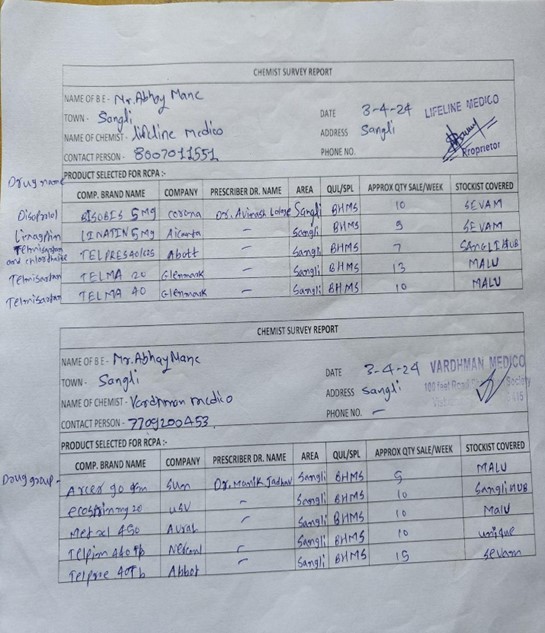
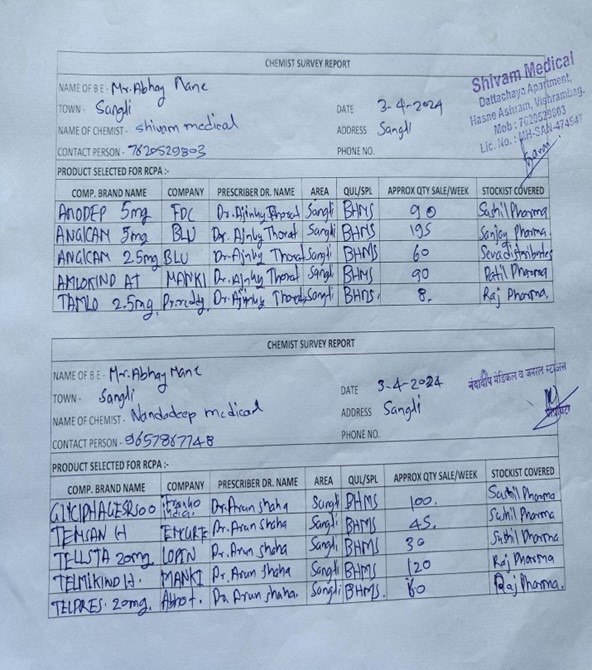
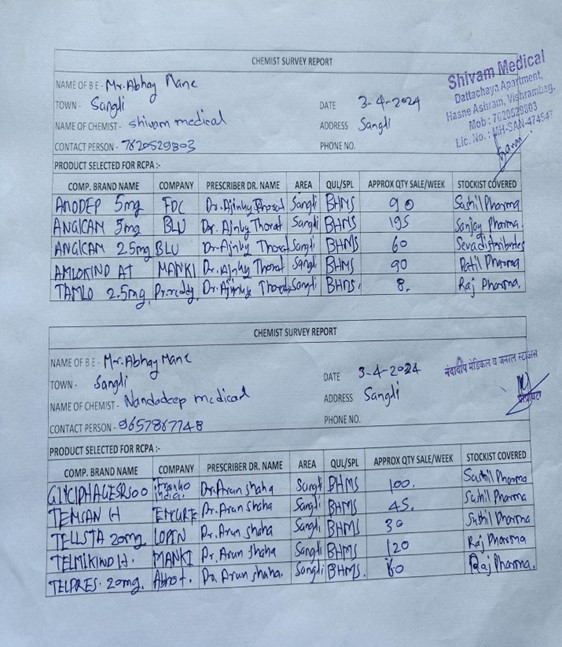
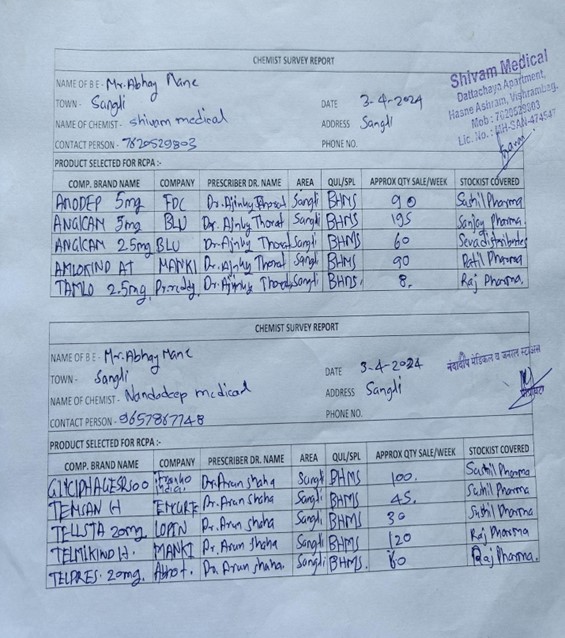
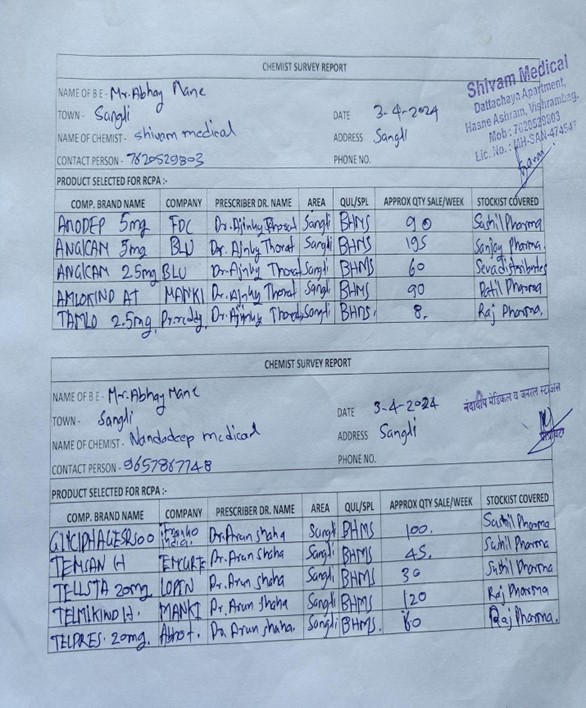
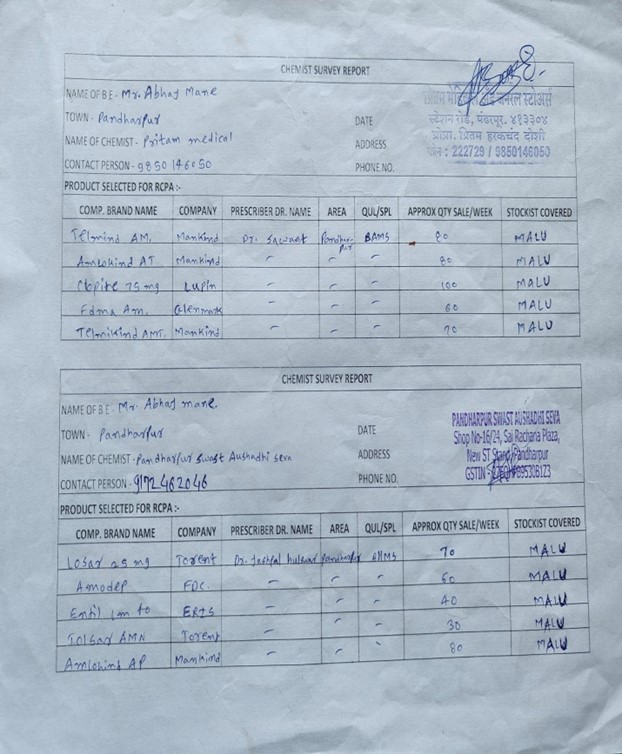
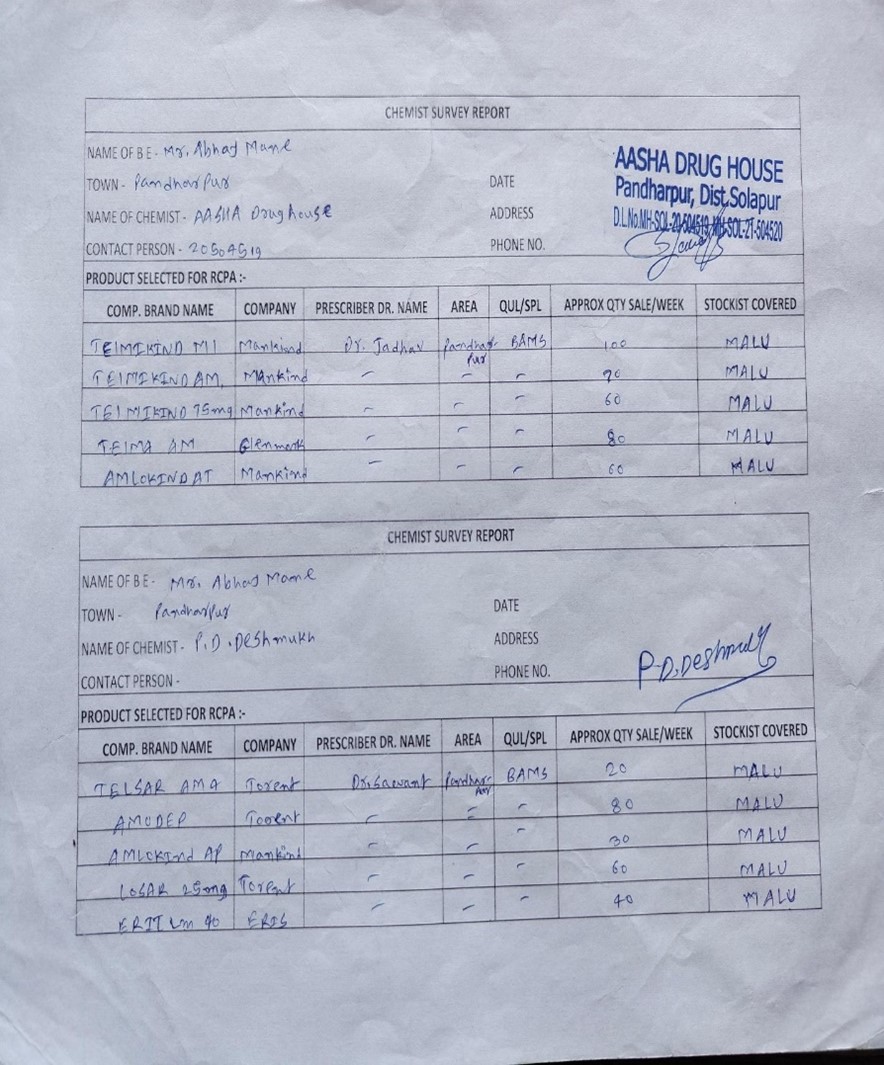
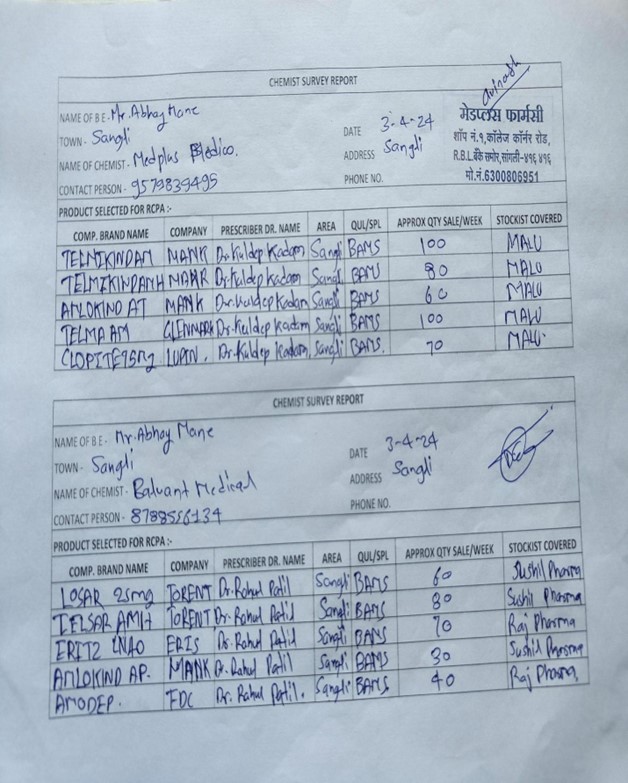
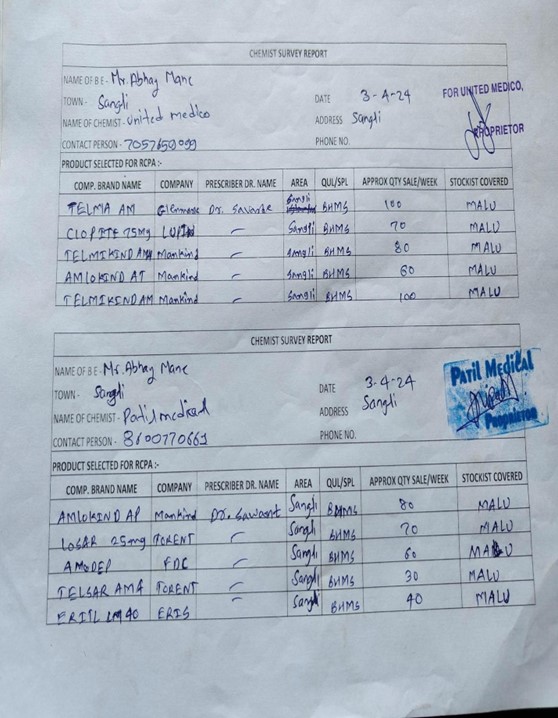
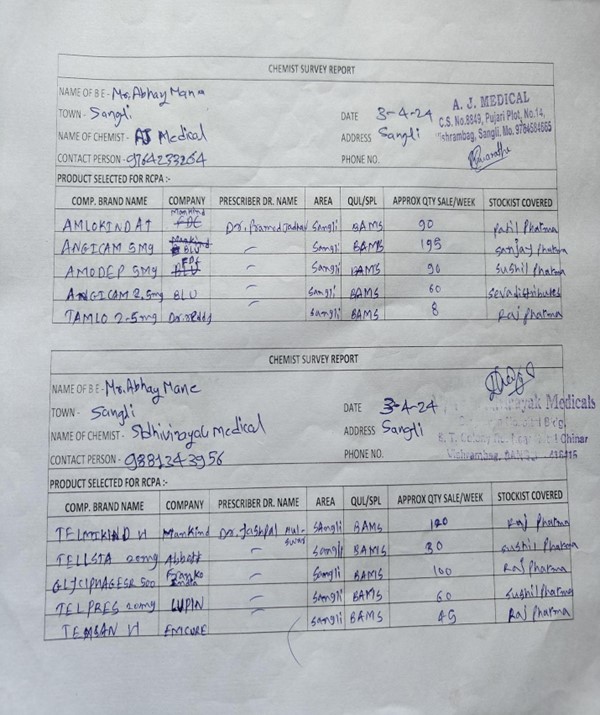
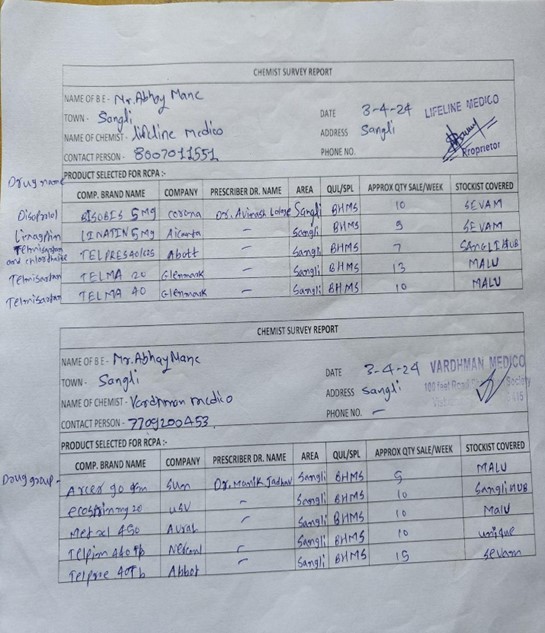
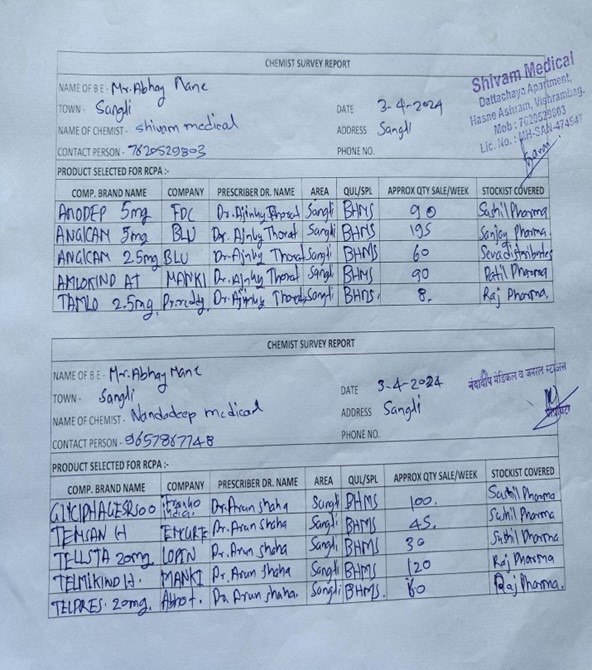
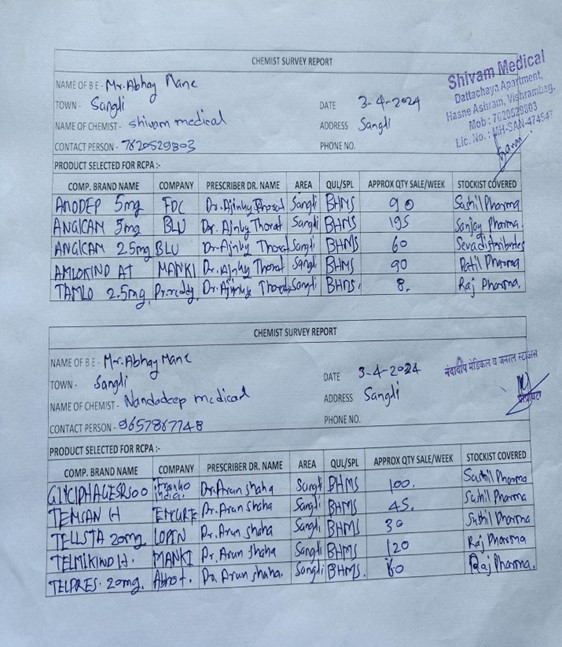
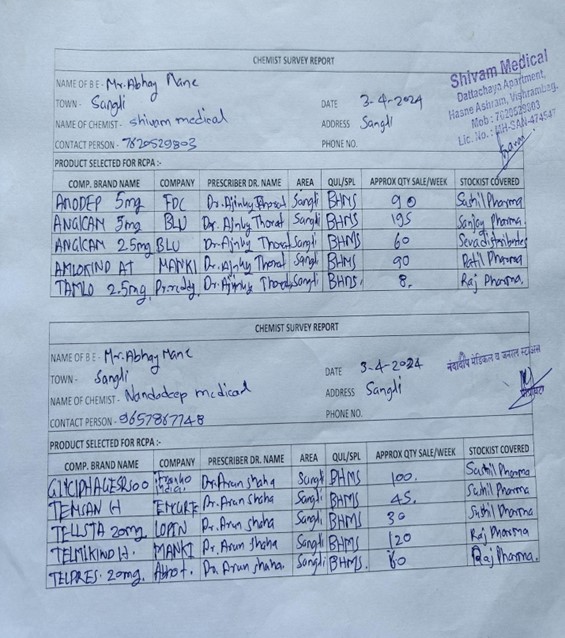
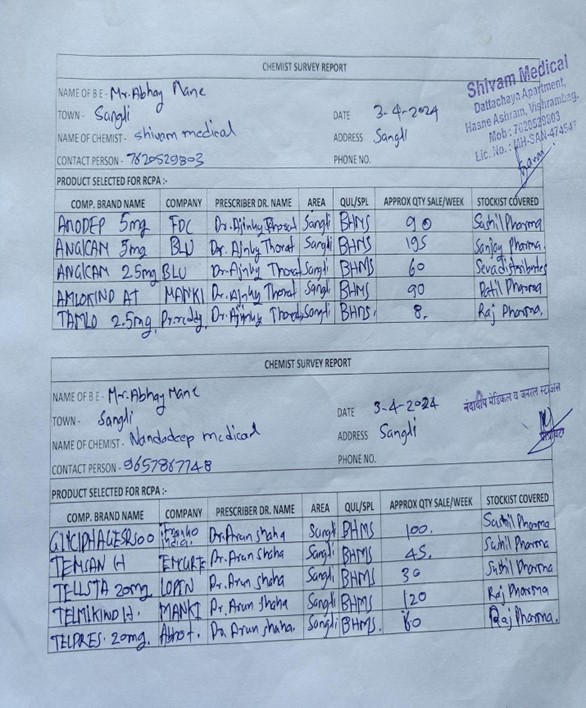
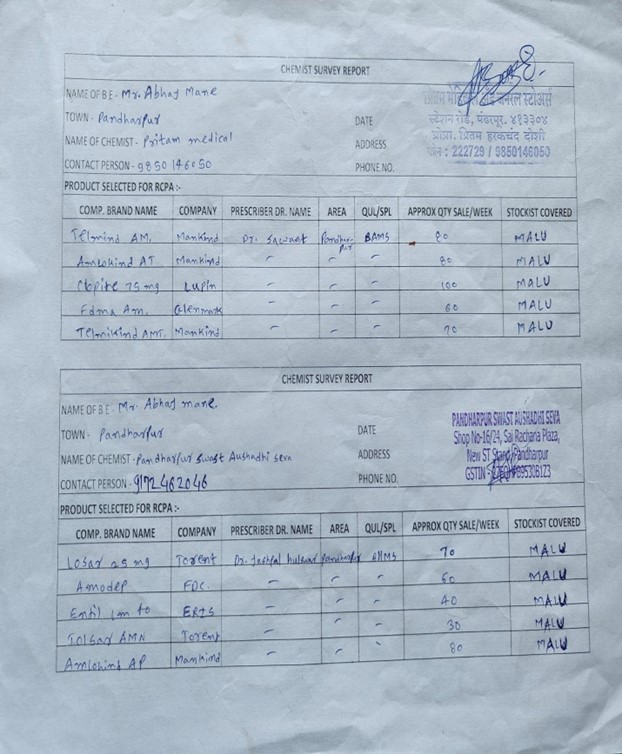
Preparation of format:
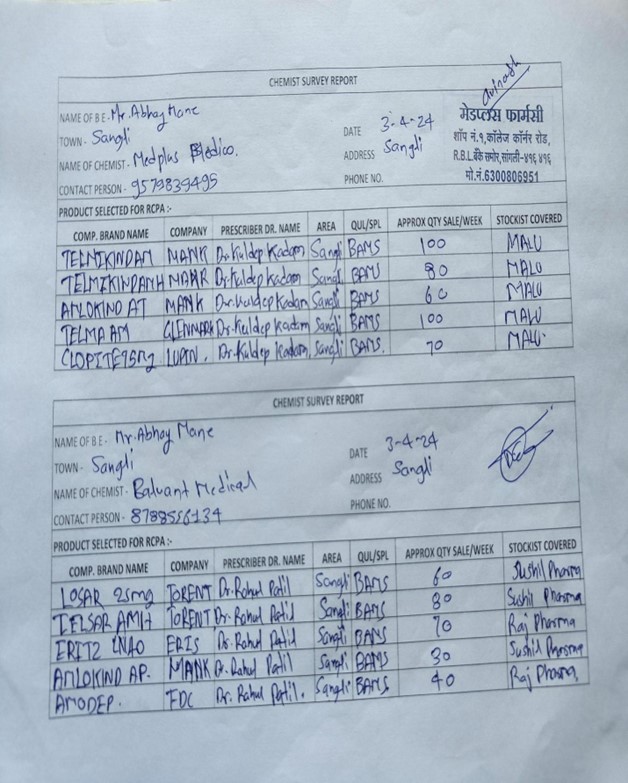
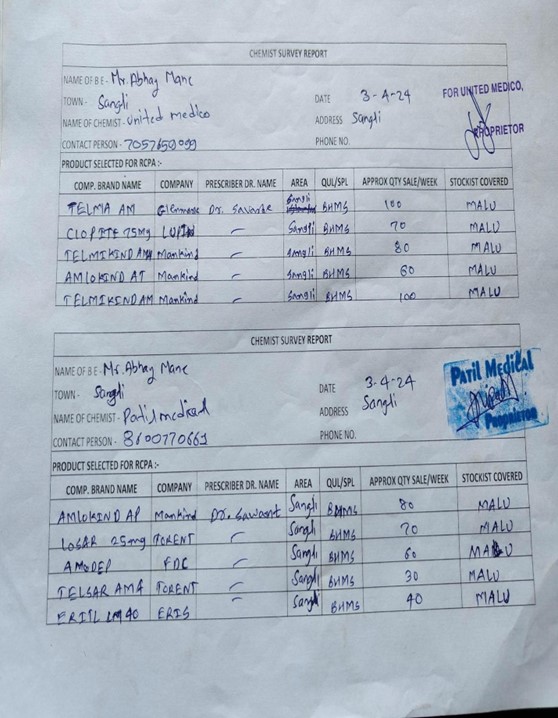
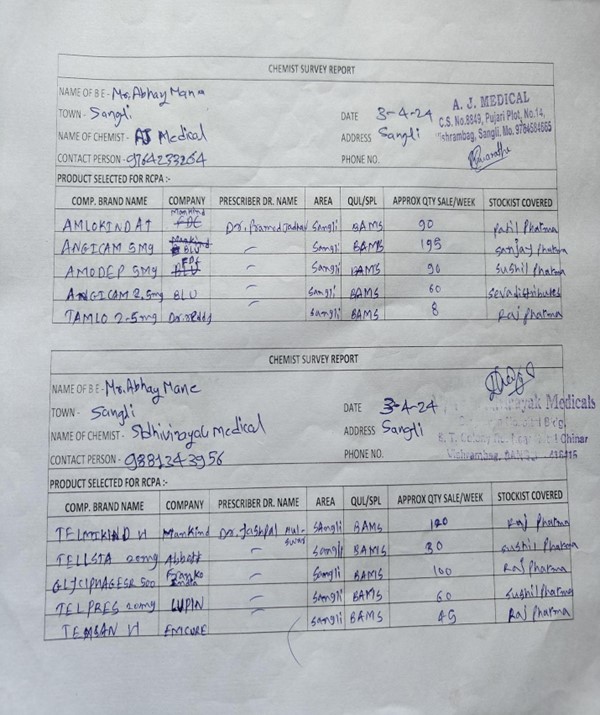
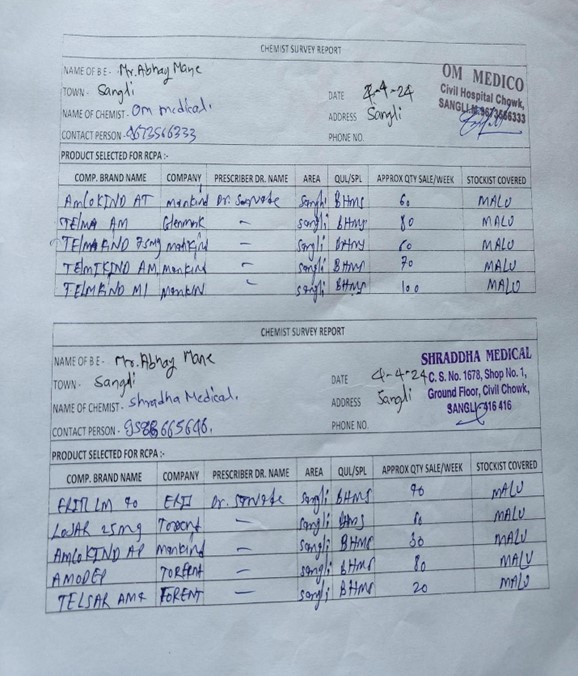
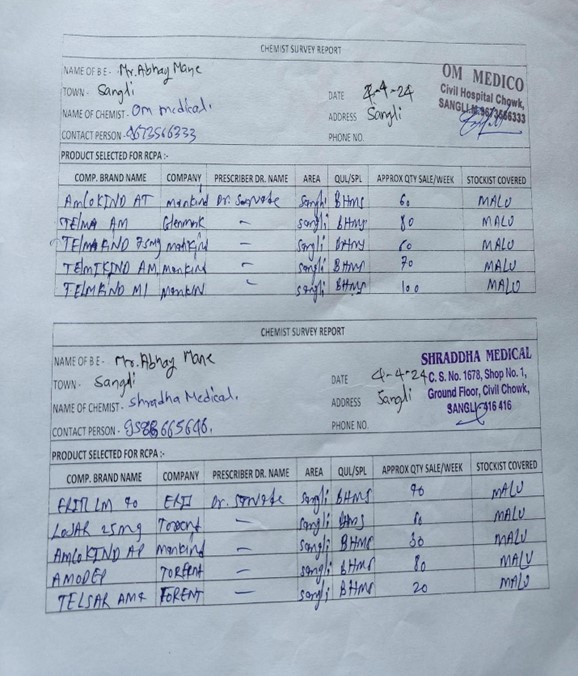
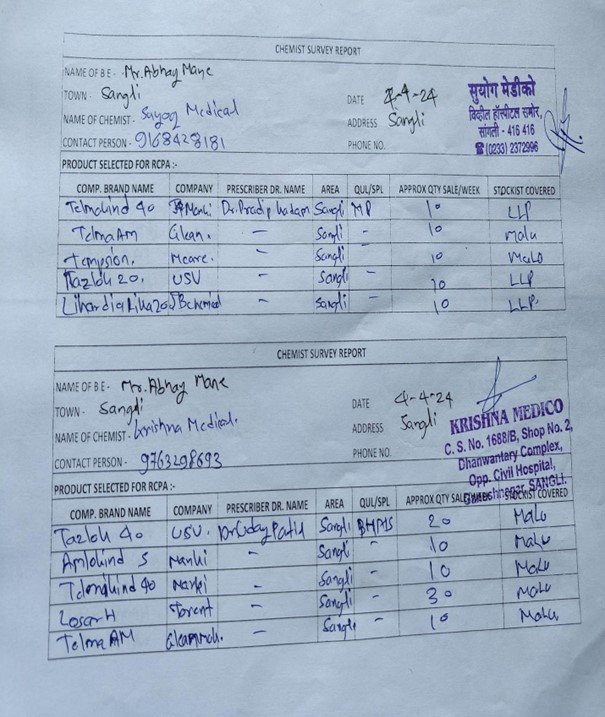
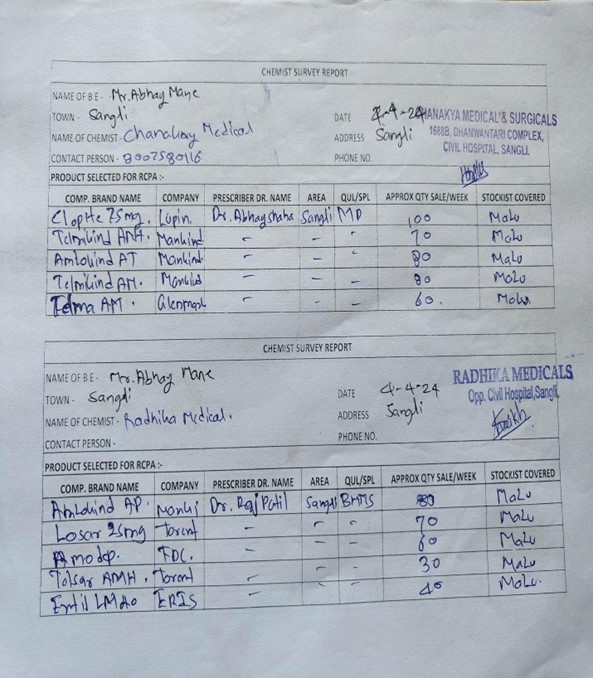
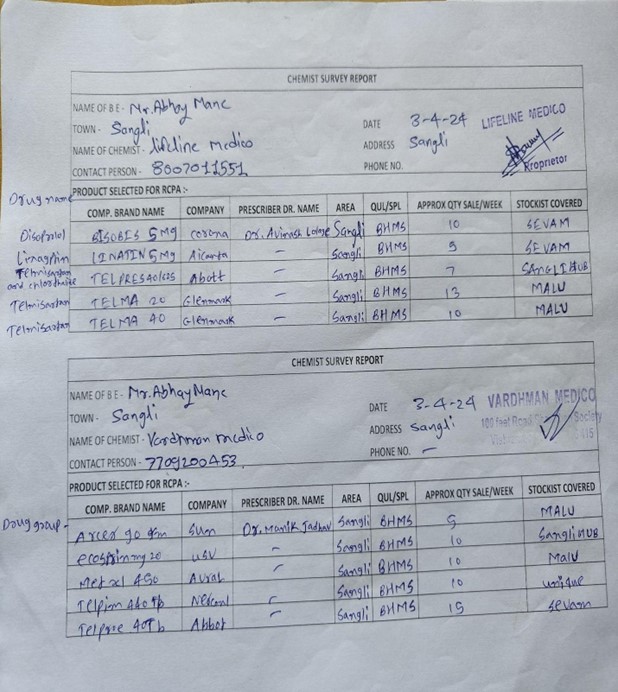
Survey report:

NEED OF WORK:
The need for a survey in the context of antihypertension is multifaceted and crucial for several reasons:
- Understanding Prevalence: Surveys help in estimating the prevalence of hypertension within a specific population or region. This data is essential for healthcare planning, resource allocation, and understanding the burden of the disease.
- Assessing Awareness and Knowledge: Surveys can gauge the level of awareness and knowledge about hypertension among the population. Understanding awareness gaps helps in designing targeted education and awareness campaigns to promote early detection and management.
- Evaluating Treatment Patterns: Surveys provide insights into the treatment patterns and practices regarding hypertension management, including the use of antihypertensive medications, adherence to treatment regimens, and barriers to treatment access.
- Identifying Barriers to Care: Surveys help in identifying barriers that hinder individuals from seeking appropriate care for hypertension, such as financial constraints, lack of access to healthcare facilities, cultural beliefs, or misinformation.
- Assessing Health Outcomes: Surveys can assess health outcomes related to hypertension management, such as blood pressure control rates, rates of complications (e.g., heart attacks, strokes), and quality of life among individuals with hypertension.
- Informing Policy and Practice: Data from surveys inform policymakers, healthcare providers, and public health professionals about the current status of hypertension management, enabling them to develop evidence-based policies, guidelines, and interventions to improve care and outcomes.
- Monitoring Trends Over Time: Surveys conducted periodically allow for the monitoring of trends in hypertension prevalence, treatment patterns, and health outcomes over time. This information is valuable for evaluating the effectiveness of interventions and identifying areas for improvement.
- Supporting Research: Surveys provide valuable data for research purposes, facilitating studies on various aspects of hypertension, including its risk factors, treatment effectiveness, disparities, and outcomes.
Conclusion of Medical Survey
-
-
-
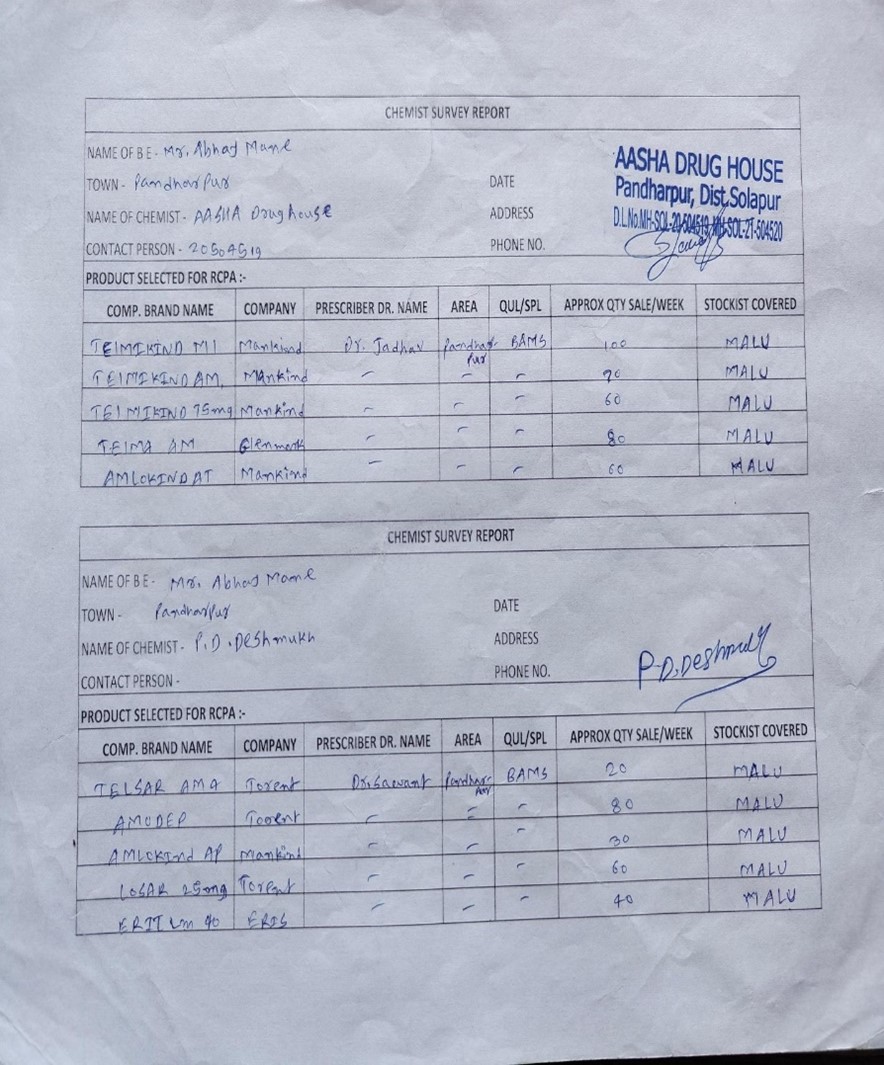
- In the current research work, we have conducted a medical survey on an anti-hypertensive drug.
- The survey focused on some pre-determined parameters such as efficacy and blood pressure control, classes of anti-hypertensive drugs, name of drug, brand name, company name, cost, and some other general parameters.
- A research study which was based on survey data found that Telmisartan is frequently used for the management of hypertension followed by Amlodipine.
- The research also found that ACE inhibitors are recommended as a first-line drug for hypertension in addition to diuretics.
- Telmisartan, an angiotensin II receptor blocker, is used frequently because of its extended duration of action, its use in diabetic neuropathy prevention, its ability to reduce the risk of stroke and heart attack, and it has fewer side effects than ACE inhibitors.
CONCLUTION
In the current research work, we have conducted a medical survey on an anti-hypertensive drug.The survey focused on some pre-determined parameters such as efficacy and blood pressure control, classes of anti-hypertensive drugs, name of drug, brand name, company name, cost, and some other general parameters.A research study which was based on survey data found that Telmisartan is frequently used for the management of hypertension followed by Amlodipine.The research also found that ACE inhibitors are recommended as a first-line drug for hypertension in addition to diuretics.Telmisartan, an angiotensin II receptor blocker, is used frequently because of its extended duration of action, its use in diabetic neuropathy prevention, its ability to reduce the risk of stroke and heart attack, and it has fewer side effects than ACE inhibitor.
REFERENCES
- {Dr. C. Sasi Sulochana1 Dr. Sharmila Jansi Rani, Effectiveness of Hypertension Prevention Program on Information among Employees at Kanaya Kumari District, Tamil Nadu, International Journal of Nursing Education and Research 7(4); 2019: 458-462.}
- {Virani Paras, Virani Kinjal, A Review on New Antihypertensive Agent: Irbesartan, Asian Journal of Research in Pharmaceutical Sciences, 6(1); 2016: 34-36.}
- {Rahul Rawat, Yogesh Joshi, Effect of Antihypertensive Drugs on Homocysteine level among Hypertensive Patients, Asian Journal of Research in Pharmaceutical Sciences, 8(4); 2018: 219-222.}
- {Indu Sharma, Dr. Bharat Parashar, Hitesh Kumar Dhamija, Ritu Sharma An Ayurvedic Arena for Hypertension Treatment, Asian Journal of Pharmaceutical Research, 2(2); 2012: 54-58.}
- {Tripathi K.D., Essentials of Medical Pharmacology, 6th End, Jaypee Brother’s Medical Publishers (P) Ltd;2008: 614-615.}
- {World Health Organization. Hypertension. 2022 [Internet]. [cited 2022 Jan 20]. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension
- {Zhou B, Carrillo-Larco RM, Danae G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021 Sep 11;398(10304):957–9.}
- {Reiss A, Pedersen M. Smoking among patients in the primary health care system in Nuuk, Greenland. Clin Nurs Stud. 2014 Sep 10;2:74.
- {Larsen CVL.Befolkningsundersøgelsen i Grønland 2018 : levevilkår, livsstil og helbred : oversigt over indikatorer for folkesundheden. Kalaallit Nunaanni innuttaasut peqqissusaannik misissuisitsineq 2018. Copenhagen: National Institute of Public Health: [In Danish];2019.
- {Diao, D; Wright, JM; Cundiff, DK; Gueyffier, F (Aug 15, 2012). "Pharmacotherapy for mild hypertension.". The Cochrane database of systematic reviews 8: CD006742. doi:10.1002/14651858. CD006742. pub2. PMID 22895954.}
- {Neil S. Skolnik, Jonathan D. Beck, Mathew Clark, Combination Antihypertensive Drugs: Recommendations for Use Am Fam Physician; 61(10); 2000: 30049-3056.9. Barar F.S.K. Essentials of Pharmacotherapeutics, 4th End, S. Chand and Company Ltd: 298, (2007).}


 Abhay Mane* 1
Abhay Mane* 1
 Pritam Salokhe 2
Pritam Salokhe 2

 10.5281/zenodo.12790440
10.5281/zenodo.12790440