Abstract
The Buccal drug delivery system includes drug administration through the buccal mucosa, mainly composed of the lining of the cheeks. Buccal drug delivery leads direct access to the systemic circulation through the internal jugular vein bypasses drugs from the hepatic first pass metabolism leading to high bioavailability. Buccal route is an attractive route of administration for systemic drug delivery. basic components of buccal drug delivery system are bioadhesive polymers, Backing membrane, Permeation enhancers. Novel drug dosages forms such as Bio adhesive tablet, films, gel, wafers, etc. and various method used in the preparation of novel buccal drug delivary system. The objective of this article is to review buccal drug delivery by studies on current approaches.
Keywords
Buccal drug delivary system, Targeted, Mucoadhesive/ bioadhesive, approaches
Introduction
Since traditional dosage forms are typically linked to challenges in getting a prescribed dose to the target place in a timely manner, targeted medicine delivery to specific body parts has emerged as one of the major endeavors of the modern world. This has led to increased demands in recent years for the development and assessment of new medication delivery methods. Actually, there are greater benefits to transmucosal medication delivery routes—such as the nasal, rectal, vaginal, ocular, and oral cavities—than to peroral drug administration. [1]
The buccal mucosa offers a promising alternative to other transmucosal routes and a novel idea for regulated drug administration. When compared to alternative non-oral transmucosal medication administration routes, it offers superior accessibility and high patient satisfaction. Additionally, because the drug avoids the hepatic first pass metabolism and enters the systemic circulation directly, without the need for acid hydrolysis in the GI tract, the buccal mucosa has a higher bioavailability. [1,2] medicine delivery methods that use the bio adhesion of specific water-soluble polymers, which become sticky when hydrated, to target a medicine to a specific area of the body for prolonged periods of time are known as mucoadhesion systems, People Know about the new things, we are discussing novel dosages forms and current approaches of buccal/ Mucoadhesive drug delivery. with some new composition or new technique.[3]
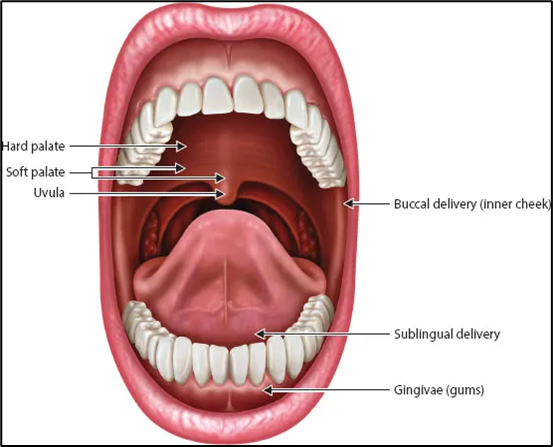
Mucoadhesive Drug administration System in Oral Cavity: There are several categories of drug administration through the oral cavity's membranes, including: (Fig. 1)
1) Sublingual Delivery: medications enter the bloodstream through the mucosal membrane that lines the floor of the mouth.
2) Buccal Delivery: medications are inserted between the cheeks and gums to pass through the mucosal barrier and into the bloodstream.
3) Local Delivery: medication is administered directly into the mouth.[4]
Anatomy of the oral mucosa
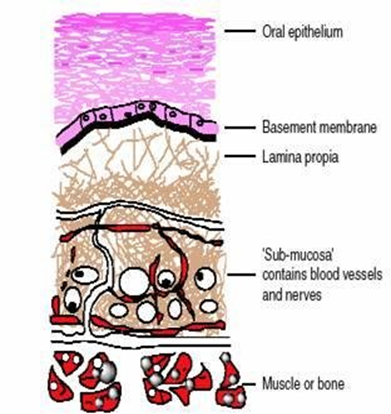
The outermost layer of stratified squamous epithelium, the basement membrane, and the connective tissue made up of the lamina propria and submucosa are the three layers that make up the oral mucosa (Fig. 2). The intestinal mucosa has a lower permeability than the buccal mucosa, which is 4–4000 times larger than the skin epidermis.[5] The order of permeability in the oral cavity is sublingual, buccal, and palatal. [6,7]
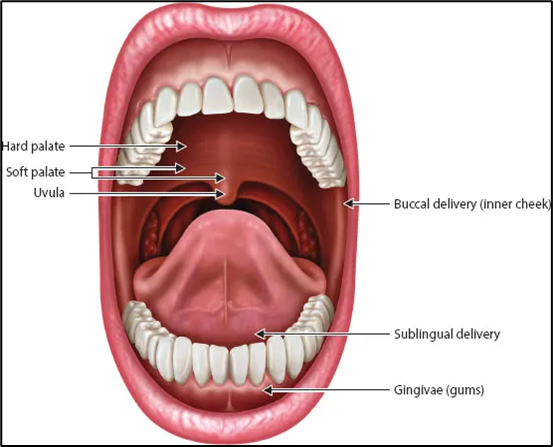
Fig. 1: Anatomy of the oral cavity
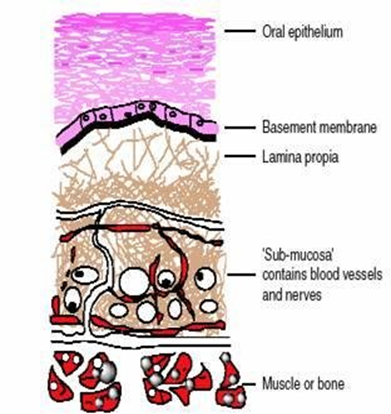
Fig. 2: Buccal mucosa
A. Structure: This oral mucosa is anatomically divided into;
1. Epithelium
2. Connective tissues and the basement membrane
1) Epithelium: The epithelium is made up of roughly 40–50 layers of 500–800 ?m thick stratified squamous epithelial cells. The oral mucosa's epithelium protects tissues and acts as a barrier to keep outside substances out.
2) Connective Tissue and Basement Membrane: The connective tissues and the basal layer of epithelium are separated by the basement membrane (BM), a continuous layer of extracellular materials. Although connective tissue and the basement membrane may restrict the mobility of some macromolecules and complexes, they are not thought to affect the diffusion of the majority of substances of pharmacological significance.
B. Buccal Mucosa Environment: Saliva produced by the salivary glands and mucus secreted by the major and minor salivary glands as part of saliva are characteristics of the oral cavity. [4, 8]
Table 1: Function of saliva and mucus
|
Function of Saliva
|
Function of Mucus
|
|
• Protective fluid for all tissues of oral cavity.
• Continuous mineralization
/ Demineralization of tooth enamel.
• To hydrate oral mucosal dosage forms.
|
• Made up of proteins and carbohydrates
• Cell-cell adhesion, Lubrication
• Bio adhesion of mucoadhesive drug
delivery systems Pathways of Drug absorption
from buccal mucosa.
|
C. Mucus Composition:
The sublingual gland, parotid gland, and other salivary glands are among the glands in the oral cavity that typically secrete oral mucus. Goblet cells or certain exocrine glands that work with mucus cells secrete the mucus, which is a translucent gel.[9]
Table 2: Composition of oral mucus cavity [10]
|
Components
|
Percentage
|
|
Water
|
95%
|
|
Glycoproteins and lipids
|
0.5-5%
|
|
Mineral salts
|
61%
|
|
Free proteins
|
0.5-1%
|
Mechanism of buccal absorption:
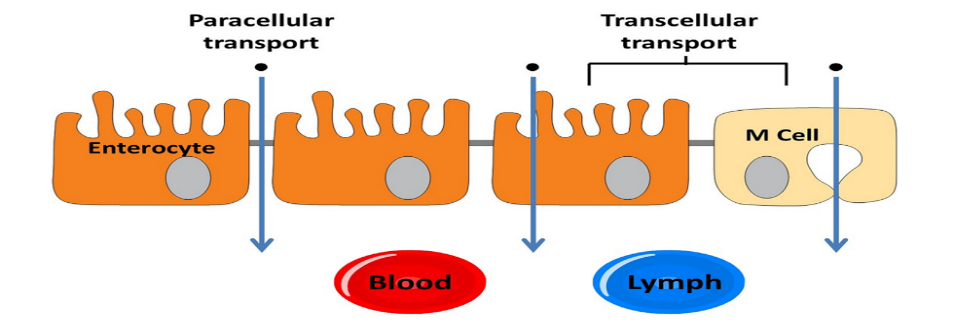
The non-ionized species passively diffuses the medication into the buccal region. A concentration gradient primarily controls the process of passive diffusion through the epithelium's intercellular gaps. The buccal mucosa is thought of as a lipoidal barrier that prevents drugs from passing through.[11]
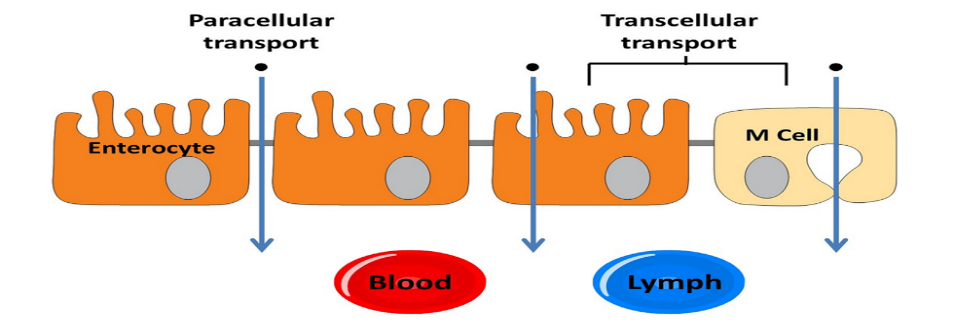
Fig. 3: Drug transport across oral epithelium
The enzymes, which include aminopeptidase, carboxypeptidase, and esterase, are usually found on the mucosal surface or inside intracellular compartments. They can act as an extra barrier to medications that penetrate the buccal epithelium. A medicine may or may not interact with all of the enzymes that are present in the mouth cavity, depending on the kind of transport route. However, in contrast to the gastrointestinal tract, the mouth cavity has a less severe enzymatic barrier. The onset of a clinical impact occurs when the drug or drugs diffuse across different biological membrane barriers to reach the target site at the desired concentration. Drugs must either stay at the target site in the buccal area to provide a pharmacological effect or travel through the mucosal epithelial layers to reach systemic circulation after buccal delivery. [12]
Theories of Adhesion: A variety of theories have been put out to explain the mechanism of mucoadhesion, a complex phenomenon. Table 3 provides a summary of these theories, which are helpful in comprehending how mucoadhesive polymers adhere to biological membranes.[13]
Table 3: Theories of mucoadhesion.
|
Theory
|
Comments
|
|
Diffusion Theory
|
? It describes the diffusion of polymer toward the adhesive surface, The diffusion process is governed by its concentration gradient at the applied surface, The penetration of the mucoadhesive polymer depends on the diffusion coefficient
|
|
Electronic Theory
|
? It describes the transfer of electrons across the applied surface, Adhesion occurs due to differences in electronic distribution and attractive forces result in the formation of an electric double layer at the interface
|
|
Adsorption Theory
|
? It suggests that forces (van der Waals forces, hydrogen bond, ionic bond, and covalent bond) at the surface are responsible for the adhesive contact developed between a mucoadhesive polymer and the mucosa
|
|
Wetting Theory
|
?This applies to liquid systems
? It explains the ability of the liquid system to spread on the applied surface
|
|
Fracture Theory
|
? Describes the force required to separate the two layers after adhesion is completed
? Used to measure the adhesion between rigid or semi-rigid mucoadhesive system
|
Basic components of buccal drug delivery system: The basic components of buccal drug delivery system are
- Drug substance
- Bio adhesive polymers
- Backing membrane
- Permeation enhancers
Drug substance
Prior to creating mucoadhesive drug delivery systems, it is necessary to determine if a local or systemic effect and quick or extended release are the desired outcomes. Pharmacokinetic characteristics should guide the choice of an appropriate medication for the development of buccoadhesive drug delivery systems.
Characteristics of drug substance:
- The conventional single dose of the drug should be small.
- The drugs having biological half-life between 2-8 hrs are good candidates for controlled drug delivery.
- Through oral route drug may exhibit first pass effect or presystemic drug elimination.
- The drug absorption should be passive when given orally. [14]
Bio adhesive polymers
In buccoadhesive medication delivery systems, bioadhesive polymers are essential. Additionally, polymers are employed in matrix devices, which control the length of drug release by embedding the drug in the polymer matrix. The most varied family of polymers are bioadhesive polymers, which offer significant advantages in patient care and treatment. The medicine is delivered into the mucous membrane through a core layer or rate-controlling layer. The oral drug delivery system is greatly enhanced by bioadhesive polymers that stick to the mucin/epithelial surface.
Characteristics of an ideal mucoadhesive polymer
- It should be inert and compatible with environment
- It should adhere quickly to moist tissue surface.
- The polymer and its degradation products should be non-toxic.
- The polymer must not decompose on storage or during the shelf life of dosage form.
- It should allow easy incorporation of drug in to the formulation.
- The polymer should be economic and easily available in the market. [15]
Backing Membrane:
A significant part of the bioadhesive in mucus membranes is the backing membrane. Inert materials that are impermeable to the medication and penetration enhancer should be utilized as backing membranes. This type of impermeable barrier on buccal bioadhesive patches improves patient compliance and stops medication loss. The following compounds are frequently used in backing membranes: polycarbophil, carbopol, magnesium stearate, HPMC, HPC, and CMC.
Permeation Enhancers:
Permeation enhancers are substances that help substances pass through the buccal mucosa. The drug's physicochemical characteristics, the site of administration, the kind of vehicle, and additional excipients all influence the enhancer's choice and effectiveness. [12]
Novel buccal dosage forms: The novel type of buccal drug delivary are show in following chart.

- Buccal mucoadhesive tablets: It is necessary to wet the dry dosage forms known as buccal mucoadhesive tablets before applying them to the buccal mucosa. As an illustration, consider a double-layered tablet with an inner core of cocoa butter that contains insulin and a penetration enhancer (sodium glycocholate) and an adhesive matrix layer made of HPC and polyacrylic acid.
- Patches and Films: Buccal patches are made of two laminates, which are cut into the necessary oval shape after an impermeable backing sheet is coated with an aqueous solution of the adhesive polymer. "Zilactin" is a new mucosal adhesive film made of three organic acids and an alcoholic HPC solution. Even when it is challenged with fluids, the film that is placed to the oral.
- Semisolid Preparation: Solid bioadhesive dosage forms are more patient-acceptable than bioadhesive gels or ointments, and the majority of the dosage forms are only utilized for oral cavity localized medication therapy. Orabase, one of the first oral mucoadhesive delivery methods, is made up of finely crushed pectin, gelatin, and NaCMC that are dissolved in ethylene polymer and a mineral oil gel base. It can be left at the application site for 15 to 150 minutes.
- Powders: A considerable increase in residence time compared to an oral solution is observed when HPC and beclomethasone in powder form are sprayed into the oral mucosa of rats. Additionally, 2.5% of beclomethasone is kept on the buccal mucosa for more than 4 hours. [16]
- Micro particles: The most significant carriers of antibacterial medications or other bioactive agents for oral infectious disorders are micro or nanoscale particles, particularly nanoparticles, whose sizes are estimated in micrometers and nanometers.[17]
Tablets are not as advantageous as microparticles. Microspheres' physical characteristics allow them to come into close touch with a sizable mucosal surface. The success of these microspheres is restricted by their brief residence duration at the site of absorption, despite the fact that they can also be administered to less accessible locations including the nasal cavity and GI tract and that they produce no local irritation at the site of adhesion.[18]
Nanoparticles: chitosan and dextran sulfate-based mucoadhesive nanoparticles made by the ionic gelation technique. The diameter of the nanoparticles was adjusted between 110 and 360 nm in order to improve their properties and accelerate their commencement of action.
- Wafer: Wafer is a new method for delivering drugs to the periodontal area. This is used to treat infections caused by microbes.
- Lozenges: These oral medications include antibiotics, corticosteroids, local anesthetics, antifungals, and antimicrobials. Because of the first large release of the drug in the oral cavity and the subsequent rapid fall to subtherapeutic levels, lozenges require numerous daily doses.[17]
Advantages: Buccal routes of drug delivery offer a large number of advantages over the other route of drug administration.
- Drug has high bioavailability because it bypass first pass metabolism.
- In unconscious and trauma patient’s drug can be administered.
- Drug release for prolonged duration of time.
- Some drugs are unstable in acidic environment of stomach can be administered by buccal delivery.
- Drug absorption occurs by passive diffusion.
- Fast onset of action. [18,19]
Disadvantages
- Small surface area (170 cm2).
- Inconvenience of patient when eating or drinking.
- Retard the rate and extent of drug absorption through the mucosa.
- Continuous secretion of the saliva leads to subsequent dilution of the drug. [20]
Ideal characteristics of buccal delivary system
- Should adhere to the site of attachment for a few hours.
- Should provide drug release in a unidirectional way toward the mucosa.
- Should not cause any irritation or inconvenience to the patient.
- Should release the drug in a controlled fashion.
- Should not interfere with the normal functions such as talking and drinking.[21]
METHODS OF PREPARATION
Buccal Tablet: Although alternate methods, such as wet granulation, can sometimes be employed, bioadhesive tablets are typically compressed directly. Tablets intended for buccal administration should dissolve or erode gradually in order to be placed into the buccal pouch. Thus, enough pressure is needed to maintain the tablets' hardness. Additionally, water-impermeable substances like ethylcellulose, hydrogenated castor oil, etc., can be applied to any tablet site—aside from the one that comes into contact with the mucosa—by compression or spray coating.[22]
Buccal Patch: The patches are laminates with three compartments: an impermeable backing layer, a reservoir layer that contains the medicine and allows for regulated release, and a bioadhesive surface for mucosal attachment. Solvent casting and direct milling are the two essential techniques for creating adhesive patches.
Buccal Film: The solvent-casting method, which is typically used to make bioadhesive films, is comparable to laminated patches in terms of both manufacturing process and flexibility. Rolling, solid dispersion extrusion, semisolid casting, solvent casting, and hot-melt extrusion.[23]
The straightforward solvent-casting approach has a few drawbacks, such as a lengthy production time, high cost, and environmental issues because of the solvents used. The hot-melted extrusion technique, which was recently published by Repka and McGinity51, can overcome these obstacles.
Buccal Gel and ointments: Particularly in contrast to tablets and patches, bioadhesive ointments have not been reviewed in the literature as thoroughly as other dosage forms. Gels and ointments are examples of semisolid dose forms that have the advantage of being easily absorbed by the mouth mucosa. Bioadhesive formulations employ a phase transition from a liquid to a semisolid to overcome the inadequate retention of the gels at the application site. The viscosity is improved by this alteration, which leads to a regulated and prolonged release of medications. Another interesting drug delivery method for the buccal region is hydrogels. They are made of polymers that have been hydrated in water, which physically traps drug molecules for later, gradual release through erosion or diffusion. [24]
Nanoparticles: Ionic gelation is used to create mucoadhesive nanoparticles based on chitosan and dextran sulfate.[17]
Method of hot melt extrusion To create a more uniform substance in various forms, such as granules, tablets, or films, a mixture of pharmaceutical ingredients is melted and then forced through an opening in the hot melt extrusion method. Oral disintegrating films, pellets, granules, and controlled release matrix tablets have all been produced via hot melt extrusion. [25, 26]
CURRENT APPROACHES OF BUCCAL DRUG DELIVARY SYSTEM
Some scientists enumerated the following as obstacles to the development and approval of buccal dosage forms: low dose drugs; the complexity of biology and permeability issues; the need for a unique mechanism to improve drug absorption without causing excessive side effects; the drug's taste and patient acceptability; the possibility of difficult dose titration for in vivo studies; and challenges relating to regulations, authorities, and economic circumstances.[27] There are currently investigations on novel buccal drug delivery formulations because of improved factors and new methods. In general, only a small number of novel buccal drug delivery dosage forms have advanced to the clinical development stage. Adding mucoadhesive ingredients or permeability enhancers to traditional dosage formulations has been the primary tactic.[28] As recombinant DNA technology advances, buccal delivery is considered crucial for creating protein and peptide compositions.[29] Numerous studies on the buccal administration of peptides have been carried out in accordance with recent advancements in buccal drug delivery systems, such as lipophilic gel, buccal spray, and phospholipid vesicles. Current research on development methods includes the formulation of a new insulin liquid aerosol and liquid crystal systems. For buccal drug delivery, nanoparticulate systems (Nanocarrier Technique) have been integrated into a number of dosage forms, such as gels, sprays, tablets, films, and patches. Research and innovation have been particularly busy in the last few years in the development of buccal delivery methods. [30, 31]
CONCLUSION:
Buccal dosage forms offer prolonged contact at the site of administration, low enzymatic activity, economy, high patient compliance, and easy administration and withdrawal. Mucoadhesive polymers may provide an important tool to improve the bioavailability of the active agent by improving the residence time at the delivery site and avoiding pre-systemic metabolism in the GIT and hepatic first-pass elimination. However, the need of safe and effective buccal permeation and absorption enhancers is a crucial component for a prospective future in the area of buccal drug delivery. The safety and efficacy of current treatments may be improved if their delivery rates, biodegradation, and site-specific targeting can be predicted, monitored and controlled. Buccal/mucoadhesive systems may play an increasing role in the development of new pharmaceuticals. Currently solid dosage forms, liquids, spray and gels applied to oral cavity are commercially successful. The future direction of buccal adhesive drug delivery lies in vaccine formulations and delivery of small proteins/peptides.
REFERENCES
- Shirvan AR, Bashari A, Hemmatinejad N. New insight into the fabrication of smart mucoadhesive buccal patches as a novel controlled-drug delivery system. European Polymer Journal. 2019 Oct 1;119:541-50.
- Rao NR, Shravani B, Reddy MS. Overview on buccal drug delivery systems. Journal of pharmaceutical sciences and research. 2013 Apr 1;5(4):80.
- Asane GS, Nirmal SA, Rasal KB, Naik AA, Mahadik MS, Rao YM. Polymers for mucoadhesive drug delivery system: a current status. Drug development and industrial pharmacy. 2008 Jan 1;34(11):1246-66.
- Singh J, Deep P. A review article on mucoadhesive buccal drug delivery system. International journal of pharmaceutical sciences and research. 2013 Mar 1;4(3):916.
- Uddin MN, Allon A, Roni MA, Kouzi S. Overview and future potential of fast dissolving buccal films as drug delivery system for vaccines. Journal of Pharmacy & Pharmaceutical Sciences. 2019 Aug 5;22:388-406.
- Johnston TP. Anatomy and physiology of the oral mucosa. Oral mucosal drug delivery and therapy. 2015:1-5.
- Macedo AS, Castro PM, Roque L, Thomé NG, Reis CP, Pintado ME, Fonte P. Novel and revisited approaches in nanoparticle systems for buccal drug delivery. Journal of Controlled Release. 2020 Apr 10;320:125-41.
- Sharma N, Jain S, Sardana S. Buccoadhesive drug delivery system: a review. Journal of Advanced Pharmacy Education and Research. 2013;3(1-2013):1-5.
- Rhushikesh S, Suresh S. A Review on Mucoadhesive Drug Delivery System. Int. J. Res. Anal. Rev. 2020 Mar;7(1):793-808.
- Sharma M, Sheeba FR, Yadav RP, Patel AK, Kumar Y. Mucoadhesive polymers for buccal drug delivery system: An overview. Asian Journal of Pharmaceutical Research and Development. 2021 Apr 15;9(2):57-64.
- Pathak B, Kumar K. Buccal drug delivery system: a tool for the effective delivery of pharmaceuticals. Universal Journal of Pharmaceutical Research. 2017 May 1.
- Jacob S, Nair AB, Boddu SH, Gorain B, Sreeharsha N, Shah J. An updated overview of the emerging role of patch and film-based buccal delivery systems. Pharmaceutics. 2021 Aug 5;13(8):1206.
- Rai A, Rawat SS, Rathi R, Raina D, Odeku OA, Singh I. Mucoadhesive Drug Delivery Systems for Pediatric and Geriatric Patients. Fabad Journal of Pharmaceutical Sciences. 2023 Oct 1;48(3):561-84.
- Sheoran R. Buccal drug delivery system: A review. Int J Pharm Sci Rev Res. 2018 May;50(1):40-6.
- Chaudhari VA, Sarode SM, Sathe BS, Vadnere GP. MUCOADHESIVE BUCCAL DRUG DELIVERY SYSTEM: A REVIEW. Pharma Science Monitor. 2014 Apr 1;5(2).
- Reddy RJ, Anjum M, Hussain MA. A comprehensive review on buccal drug delivery system. Am J Advan Drug Deliv. 2013;1:300-12.
- Sandri G, Ruggeri M, Rossi S, Bonferoni MC, Vigani B, Ferrari F. (Trans) buccal drug delivery. Nanotechnology for Oral Drug Delivery. 2020 Jan 1:225-50.]
- Budhrani AB, Shadija AK. Mucoadhesive buccal drug delivery system: a review. American Journal of Pharmtech Research. 2020;10(2):275-85.
- Satyabrata B, Ellaiah P, Choudhury R, Murthy KV, Bibhutibhusan P, Kumar MS. Design and evaluation of methotrexate buccal mucoadhesive patches. Int J Pharm Biomed Sci.2010;1(2):31-6
- Alagusundaram M, Chetty CM, Umasankari K, Anitha P, Gnanprakash K, Dhachinamoorthi D. Buccal Drug Delivery System–An Overview. Research Journal of Pharmacy and Technology. 2009;2(4):653-63.
- Bhandari HP, Yadav J. REVIEW ON MUCOADHESIVE BUCCAL DRUG DELIVERY. Pharma Science Monitor. 2018 Jan 1;9(1).
- Rossi S, Sandri G, Caramella CM. Buccal drug delivery: a challenge already won?. Drug Discovery Today: Technologies. 2005 Mar 1;2(1):59-65.
- Mahajan A, Chhabra N, Aggarwal G. Formulation and characterization of fast dissolving buccal films: A review. Der Pharm Lett. 2011;3(1):152-65.
- Verma S, Kaul M, Rawat A, Saini S. An overview on buccal drug delivery system. International journal of pharmaceutical sciences and research. 2011 Jun 1;2(6):1303.
- Srivastava N, Monga MG. Current status of buccal drug delivery system: a review. Journal of Drug Delivery and Therapeutics. 2015 Vidyasagar N, MallikarjunaRao K, Gnanaprakash K, Divya A, Sowjanya A, Gobinath M. A review on buccal drug delivery system. Journal of Pharmaceutical Research and Development. 2012;1(2):29-35.
- Rao NR, Shravani B, Reddy MS. Overview on buccal drug delivery systems. Journal of pharmaceutical sciences and research. 2013 Apr 1;5(4):80.
- Pather SI, Rathbone MJ, ?enel S. Current status and the future of buccal drug delivery systems. Expert Opinion on Drug Delivery. 2008 May 1;5(5):531-42.
- Boddupalli BM, Mohammed ZN, Nath RA, Banji D. Mucoadhesive drug delivery system: An overview. Journal of advanced pharmaceutical technology & research. 2010 Oct 1;1(4):381-7.
- Puratchikody A, Prasanth VV, Mathew ST, Kumar A. Buccal drug delivery: past, present and future-a review. International Journal of Drug Delivery. 2011 Apr 1;3(2):171.
- Hua S, De Matos MB, Metselaar JM, Storm G. Current trends and challenges in the clinical translation of nanoparticulate nanomedicines: pathways for translational development and commercialization. Frontiers in pharmacology. 2018 Jul 17;9:790.
- GÜNE? M, Karavana SY, Yapar EA. Buccal drug delivery system: an overview about dosage forms and recent studies. Universal Journal of Pharmaceutical Research. 2019.


 Neha D. Naringe*
Neha D. Naringe*
 Dimpal R. Sarkar
Dimpal R. Sarkar
 Pankaj Dhapke
Pankaj Dhapke

 10.5281/zenodo.14259094
10.5281/zenodo.14259094