Prurigo nodularis (PN) is a chronic inflammatory skin disease characterized by intensely pruritic , hyperkeratosis nodules distributed on the trunk and extension surface of the extremities . PN has a profoundly negative impact on a sleep and quality of life in patient with PN and patient are often recalcitrant to current therapies , highlighting the importance of further research into this severely debilitating condition . this condition can occur in anyone but is a most common in middle age adults is gently affect a person quality of life including sleep disturbance and higher rate of anxiety and depression . patients with severe PN have an increase amount of inflammation in their blood and PN is commonly associated with other medical condition . A dermatologist can usually diagnosis PN on clinical examination sometime a dermatologist will perform the skin biopsy to rule out other diagnoses PN is more common in patient with other medical condition including diabetes , liver , kidney and thyroid problem and certain infection physician will often screen patients with PN for this medical issues . there is no cure for PM the main treatment goal is decreasing itch because the bums fade once the itch improve . the most common initial treatment for mild PN is topical steroid cream or local corticosteroid injection.
prurigo nodularis, Immunoglobulin E , Interleukin-4 , T- cell receptor , T- helper type 2 , Major histocompatibility complex , High affinity IgE receptor , Food and Drug Administration
Prurigo nodularis (PN) is a persistent skin condition characterized by many film , flash to pink nodules that are typically found on the extension region of extremities . this illness can a affect anyone but it is most frequently among middle age individual . prurigo nodularis has a significant impact on a person quality life include sleep problem as well as increase anxiety and the despair levels , patient with several PN have a higher level of inflammation in their blood and PN is frequently connected with other medical disorder. Prurigo nodularis is a skin condition characterized by raised , intensely itchy , often painful bumps on the arms , legs and trunk [1] .
The etiology of PN is hypothesized to be define by cutaneous reaction pattern caused by prolong itching and frequently scratching often known as the ‘ itch- scratch- cycle’ . Although specific pathophysiology of PN is uncertain immunological and neurological abnormalities contribute to the pruritic . cycle . Currently there are no FDA approve targeted therapies of PN . Although the therapeutic goal is to disturb the itch scratch cycle and allow the nodules to heal the uses of off label treatment very widely among clinic and treatment regiment
Sign and Symptoms :-
1] Itchy skin :- The skin frequently itch prior to the appearance of prurigo nodularis irritating lumps. This itch might be persistent or intermittent. In any case, it’s usually quite intense. Some folks have several itching spots. Others have itching that covers a large area of their skin.

Figure No 1 :- Itchy skin
2] Skin may burn or sting :- Instead of itching, some patients report that their skin burns or stings. While it is uncommon, some patients have reported feeling bugs crawling on their skin.

Figure No 2 :- Skin may burn or sting
3] Itchy bumps (nodules ) develop :- Repeated scratching, plucking, or rubbing causes itchy pimples. Itchy lumps typically occur around six weeks after your skin begins to itch, burn, or sting. Typically, the bumps appear evenly on both sides of the body.

Figure No 3 :- Itchy bumps (nodules ) develop
4] Itchy bumps vary in color , size & number :- The pimples may be the color of your skin, pink, red, or brownish black. The size might range from that of a pinhead to greater than a US quarter. It is possible to have a few bumps or over 100 on your skin. For the most part, this figure lies somewhere around the middle. Raised, itchy patches might form on the skin.

Figure No 4 :-Itchy bumps vary in color , size & number
5] Scratching can change the skin :- Frequent scratching might lead to additional bumps and elevated regions of irritable skin. The more you scratch, the itchier your skin may get. Some people scratch until the irritating bumps or patches rupture and bleed, or the skin becomes too painful to touch. All this scraping can result in alterations. Dark patches may occur. The skin can feel pebbly, rough, and thick.

Figure No 5 :- Scratching can change the skin
6] Dark- spot , light spot or scars can appear as bumps clear :- Without therapy, the itch and pimples might persist for months or years (A). As the bumps fade, you may notice flat black areas (B) spot lighter than your natural skin color or scars where the lumps were

Figure No 6 :- Dark- spot , light spot or scars can appear as bumps clear
7] Nodules :- Hard, firm, and rounded nodules on the skin, usually 1-3 cm in diameter.
8] Itching :- Severe itching (pruritus) is a hallmark symptom, leading to scratching and skin damage.
9] Skin thickening :- Repeated scratching causes skin thickening .
10] Pigmentation :- Post-inflammatory hyperpigmentation (PIH) may occur due to chronic inflammation.
11] Skin dryness :- Dry, scaly skin (xerosis) is common.
12] Bleeding :- Scratching can lead to bleeding and crusting. [2] [3] [4] [5]
Etiology :
The exact incidence of PN remaining unknown . the majority of PN patient present between the age of 51 and 65 years , however many cases in other age groups have also been documented . The precise sequence of events leading to the final clinical picture is still up for debate, despite the fact that the function of the unhindered itching-scratching cycle is widely accepted. PN is characterized by persistent pruritus and is believed to arise in patients with chronic prurigo of several etiologies, such as neuropsychiatric, systemic, infectious, and dermatological, in response to recurrent scratching.[7] [8]. Anecdotal evidence points to the involvement or causal relationship between HIV, mycobacteria, Helicobacter pylori, hepatitis C, and Strongyloides stercoralis .[9] PN lesions result in an increase in the number of sensory structures of the epidermis ( Markel cell ) dermis ( papillary dermal nerves ) . [10] Prurigo nodularis is not communicable. It could be caused by an excess of nerve or immune cells in your skin. Other conditions may cause itchiness on the skin's surface, resulting in pimples from repeated scratching and irritation. Prurigo nodularis can sometimes be caused by medications, such as certain forms of chemotherapy.
prurigo nodularis etiology is multi factorial involving genetic , environmental and immune system facto
Genetic factor :
1] Family history : PN can run in families , Suggesting a genetic predisposition
2] Atopic dermatitis / eczema : individual with atopic dermatitis are more likely to develop PN
Environmental factors:
1. Allergies: Allergic reactions to substances like insect bites, metals, or plants.
2. Irritants: Exposure to harsh soaps, detergents, or chemicals.
3. Climate: Extreme temperatures, humidity, or dryness.
Immune system factors:
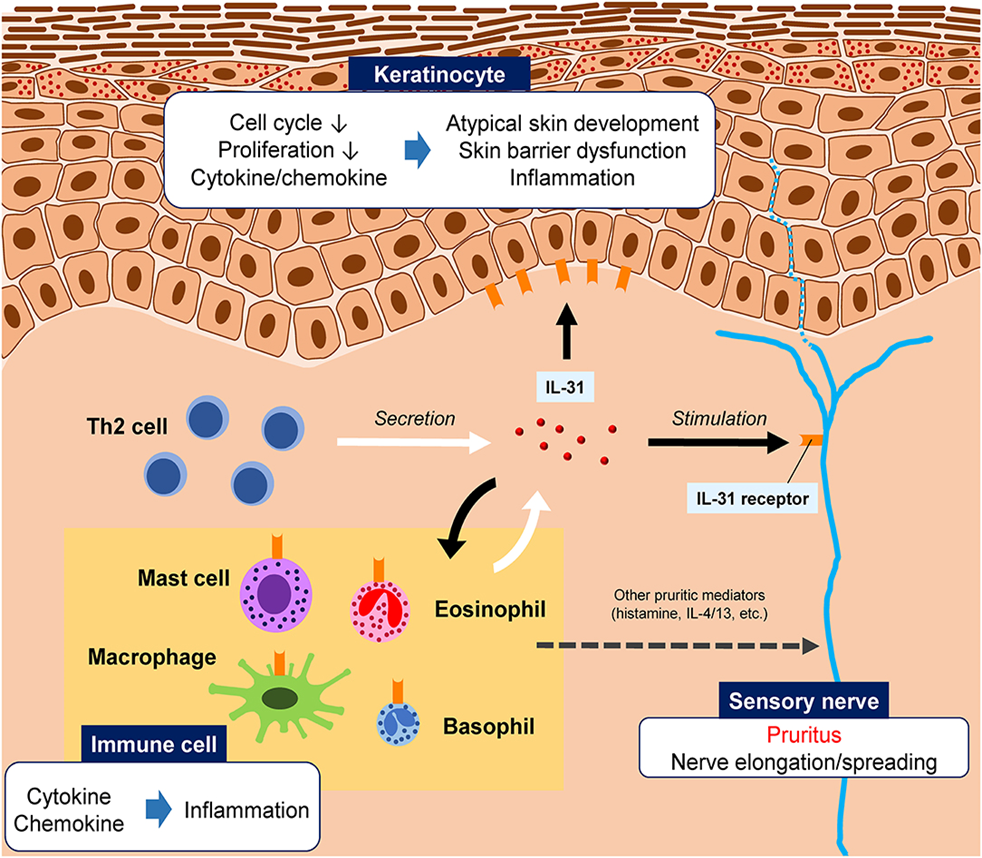
1. Abnormal immune response: Overactive immune cells lead to inflammation and skin lesions.
2. Cytokine imbalance: Altered levels of cytokines (e.g., IL-31, IL-13) contribute to PN.
Other contributing factors:
1. Hepatitis B or C
2. HIV/AIDS
3. Kidney disease
4. Liver disease
5. Nutritional deficiencies (e.g., vitamin D, zinc)
6. Stress
7. Hormonal changes
Potential triggers:
1. Insect bites (e.g., mosquito, flea)
2. Skin injuries (e.g., cuts, burns)
3. Medications (e.g., opioids, antidepressants
Evaluation : PN Is a clinical diagnosis patient with PN likely to have a history of chronic several pruritus , which include excoriations and flash colored , pink nodular lesions can extensive surface . Dermoscopy and assist distinguish between PN and HLP in one investigation dermoscopy of HLP revealed pearly white patches with peripheral striation , grey blue global , like apparatus red spots and globules and yel Weigelt et al low structures dermoscopy revealed red spot and globules in PN as well as pearly white patches with peripheral striation [11] [12]
There are various methods of evaluation of PN they are following :-
Biopsy:- Although PN is a clinical diagnosis, biopsies are frequently performed on lesions that do not respond to first-line treatments or have secondary consequences such as bleeding or ulceration.. discovered that PN (n = 136) had characteristic features such as thick orthohyperkeratosis, the hairy palm sign (folliculosebaceous units with a thick and compact cornified layer), irregular epidermal hyperplasia, hypergranulosis, papillary dermis fibrosis, and increased fibroblasts and capillaries. However, these histological features frequently overlap with other scratch-induced diseases, such as lichen simplex. To identify PN from other scratch-induced diseases, clinical and histological results must still be correlated.[25]
Laboratory Evaluation:- As previously stated, PN can frequently be caused by a systemic underlying condition. A complete laboratory work-up is recommended, especially for patients who have no history of underlying dermatoses, such as PN developing from atopic dermatitis. Chronic pruritus should be thoroughly investigated for systemic reasons, including chronic renal failure, liver disease, HIV, and thyroid illness. PN has seldom been associated with gout, iron deficiency anemia, celiac disease, non-Hodgkin's lymphoma, or an infection.
Treatment & Management : PN management demands a diverse strategy. Patients must be instructed on how to reduce scratching of lesions. Furthermore, any psychiatric illness related with scratching and picking at the skin should be identified and treated. Any underlying causes of pruritus should also be addressed. Topical and cycle. systemic treatments for PN aim to break the itch-scratch
General care : Patient with PN should be care advise to ;
- Keeping their nails short , wear protective clothes ( ie . long sleeves and gloves )and keep the nodules covered with bandage .
- Bothe the gentle cleansers and apply emollients throughout day to keep skin moisturized
- Use calamine lotion and lotion containing menthol and camphor to provide itch relief
- Stay in a cool , comfortable environment
- Reduce trace [1]
Specific care :
1] Topical therapies :
- Topical anti-inflammatory therapies . eg- ( topical corticosteroid , intralesional corticosteroid , topical calcineurin inhibitor , tacrolimus , pimecrolimus
- Topical analgesics . eg – ( anesthetics , cryotherapy , the transient receptor potential vanilloid 1 ,agonist capsaicin )
- Topical antiproliferative agents . eg – ( coal tar , vitamin D derivative , like calcipotriene
2] Ultraviolet phototherapy :
- (Narrowband , ultraviolet B light , psoralen plus ultraviolet A & laser therapies , excimer laser )
3] Systemic therapies :
- Antihistamines
- Conventional immunosuppressants ; ( oral corticosteroids , cyclosporin , methotrexate , azathioprine , thalidomide)
- Neuromodulating therapies ; ( opioid modulators like naloxone , naltrexone and nalbuphine , neurokinin-1, receptor , antagonist like aprepitant and serlapitant , antidepressant like paroxetine , fluvoxamine and duloxetine , gabapentinoids
- Immunomodulating therapies ; ( biologics like dupilumab , nemolizumab and oral janus kinase inhibitor ) [13]
Topical and intralesional therapy :-
- Although no randomized trial have been conducted topical therapy for PN include class 1 corticosteroids intralesional corticosteroid topical calcineurin inhibitor topical capsaicin and topical vitamin d analogue
- Triamcinolone acetonide injection at dosage ranging from 10mg/ml to 20mg/ml have been demonstrated to flatten lesion and alleviate itch [14] [15] [16]
- Pimecrolimus 1% is equally effective as hydrocortisone and can be used on a long – term basis [17]
- Calcipotriol ointment has higher efficacy than betamethasone valerate 0.1 [18]
- Low methanol concentration (<5>
Antihistamine and leukotriene inhibitor :
- High dose nonsedating antihistamine can be taken throughout by first generation sedating antihistamine at night a combination of fexofenadine and montelukast produce satisfactory outcome [19]
- Common antihistamine side effect include sleepiness , dizziness , and weakness
Phototherapy and excimer laser :
- Phototherapy with psoralen-ultraviolet-A (PUVA), including bath and topical PUVA, long-wavelength UVA, narrowband UVB, and monochromatic excimer light at 308 nm, has been utilized and proved to treat PN nodules.
- Narrow band. UVB phototherapy effectively improves PN at an average dose of 23.88-26.00 j/cm2.
- Excimer lasers are more effective than topical clobetasol.[20]
Oral immunosuppressant :
- As with topical medicine , no randomized trial have been reported utilizing this systemic medication the advantages vs hazard of the drug mostly weight before initiative treatment [21]
- Patience with several recalcitrant PN should consider receiving oral immunosuppressive treatment
- A Retrospective analysis conducted at a single institution found that cyclosporin at a mean dose of 3.1 mg/ kg improve medical outcomes and reduce pruritus
- Treatment with azathioprine and cyclophosphamide has also be shown to be effective
- Methotrexate doses ranging from 3to 10 mg/ kg weekly resulted in full or partial remission lasting 2.4 months .These patients had a mean duration of response of 19 months
- Oral tacrolimus therapy significantly reduced pruritus in a patient previously treated with cyclosporin [22]
Novel Treatment :
- Thalidomide is an immunomodulatory drug that also functions as a central and peripheral depressive and a tumor nacrosis factor Alpha inhibitor the theraphetic efficiency against PN is assumed to originate from its neurotoxic effects
- Lenalidomide a more potent molecular version of thalidomide is beneficial in PN and has a decrease risk of peripheral neuropathy [23]
- Both selective serotonin reuptake inhibitor and tricyclic antidepressants can be used to treat chronic pruritus it is equally cruci al for patient to be seen with mental health specialists
- Naloxone and naltrexone have antipruritic action by blocking Mu-opioid receptors on nociceptive neurons and interneurons , which suppresses itch.
- Aprepitant and serlopitant , which are NK1r antagonists , may block substance p- mediated signaling in the development of PN . In PN patients treated with aprepitant monotherapy , itch was significantly reduced.
Differential Diagnosis:-
Several skin conditions can mimic PN. We review a number of unusual illnesses that have been reported in the literature as PN masqueraders. These diagnoses are frequently made after the patient has become resistant to treatment and has been further investigated
a] Pemphigoid Nodularis : Pemphigoid nodularis is a rare variant of bullous pemphigoid that has features of both prurigo nodularis and bullous pemphigoid. Compared to PN, pemphigoid nodularis is often characterized by larger plaques often with large areas of central erosion, ulceration, and/or blistering .On biopsy, there is also evidence of subepidermal clefting, and direct immunofluorescence (DIF) shows linear deposition of IgG and C3 at the basement membrane zone.[26]
b]Actinic Prurigo:- Actinic prurigo is a rare kind of photodermatosis characterized by acute eruptions of extremely pruritic papules or nodules, which are sometimes accompanied by cheilitis and conjunctivitis. This syndrome is more common in young girls, and they show severe photosensitivity to UVA and UVB.[27]
c] Hypertrophic Lichen Planus. :- Hypertrophic lichen planus (HLP) might appear clinically similar to PN, with hyperkeratotic plaques and nodules primarily affecting the shin and ankles. Histopathology can be extremely similar, with both showing epidermal hyperplasia, hypergranulosis, compact hyperkeratosis, and an increased number of fibroblasts and capillaries. However, basal cell degeneration is limited to the terminals of the rete ridges, and band-like infiltration is frequently lacking in HLP compared to PN.[28]
d] Neurotic Excoriations :- Neurotic excoriations, commonly known as dermatotillomania, can produce excoriations with slightly elevated patches similar to PN lesions. Neurotic excoriations is a psychiatric disease characterized by frequent plucking of the skin.
Due to similar morphologies , PN is often confused with and must be clinically separated from
-
- HLP
- Pemphigoid nodularis
- LS chronicus
- Keloid
- Dermatofibroma
- Foreign body reaction [27]
Complication :
Scratching PN lesion can cause secondary infection resulting in ulceration of abscess formation and cellulitis it is critical to watch for clinical symptoms of infections such as erythema , discomfort, warmth and fever if secondary infection is suspected it is vital to common adequate tropical or systemic antibiotic medication to cover the skin flora PN can cause a number of problems, including: PN increases the risk of cardiovascular illnesses, including coronary heart disease, congestive heart failure, and death. Other medical conditions. PN may be related with various medical problems such as chronic kidney and liver disease, diabetes, chronic obstructive lung disease, HIV, and chronic hepatitis C. PN can be linked to mental health issues such as anxiety and depression. PN can coexist with other inflammatory skin conditions, including atopic dermatitis, plaque psoriasis, lichen planus, and dermatitis herpetiformis. Delusional infestation is a possible complication of PN [25 ] [26 ]
Monoclonal Antibody :-
The dupilumab and nemolizumab are the example of human monoclonal antibody suggest in the treatment of Prurigo nodularis
Dupilumab ;-
Dupilumab is a human monoclonal IgG4 antibody directed against the interleukin ( IL4 ) receptor alpha chain ( IL4R alpha ) and inhibit signaling of both IL -4 and IL -13
Dupilumab also show the efficacy in pruritus with several identified etiology . This include six cases of uremic pruritus and one of the cholestatic pruritus . [28]
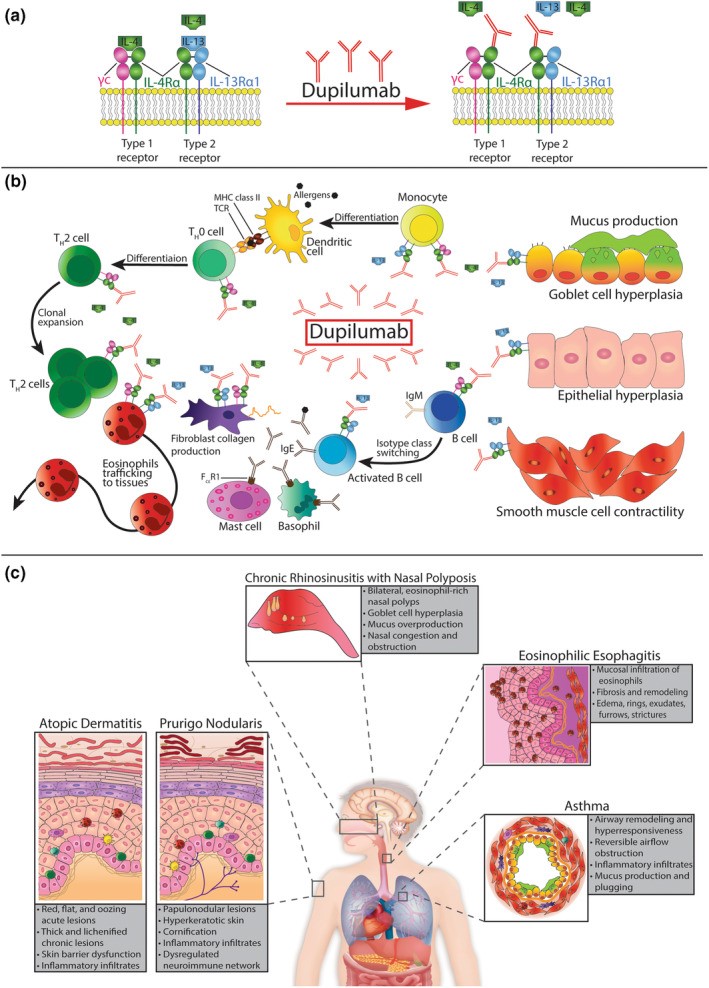
MOA :- The mechanism action within the type 2 inflammatory cascade
Dupilumab mechanism of action occurs inside the type 2 inflammatory cascade.
A] Dupilumab binds to the common IL-4 receptor subunit alpha (IL-4R?) of type 1 and type 2 receptors, which target IL-4 and IL-13.
B] Monocytes, TH0 cells, TH2 cells, fibroblasts, eosinophils, and B cells all express type 1 receptors. The type 2 receptor is present on monocytes, fibroblasts, eosinophils, activated B cells, epithelial cells, goblet cells, and smooth muscle cells. Dupilumab reduces type 2 inflammation by blocking the IL-4/IL-13 axis, which is a main cause of inflammation. IL-4 increases the differentiation and clonal proliferation of TH2 cells, leading to increased production of IL-4 and IL-13. IL-4 and IL-13 stimulate type 2 inflammatory activities, including eosinophil trafficking to tissues, B cell isotype change to IgE, and collagen formation by fibroblasts. IL-13 is mainly responsible for mucus formation, goblet cell hyperplasia, and smooth muscle cell contraction.
C] Type 2 inflammatory illness shares similarities but has distinct etiology and symptoms. Dupilumab is beneficial in treating these disorders because they share common underlying type 2 inflammatory pathways. MHC class II is a major histocompatibility complex that presents antigens. TCR is a T cell receptor, while Fc?R1 is a high-affinity IgE receptor. [29]


 Sakshi Manal *
Sakshi Manal *
 Rahul Mohan
Rahul Mohan
 Dr. Kawade Rajendra.
Dr. Kawade Rajendra.






 10.5281/zenodo.14247765
10.5281/zenodo.14247765