Abstract
Gender discrepancies play a pivotal role in shaping the trajectory of type-2 diabetes, impacting its etiological underpinnings, subsequent complications, approaches to medical treatment, and patient adherence and retention. A robust body of research consistently underscores that women diagnosed with type 2 diabetes face a disproportionately higher risk of developing cardiovascular issues, particularly concerning macro vascular complications, which often culminate in elevated rates of cardiovascular disease mortality. This increased vulnerability is further compounded by the cessation of hormonal protection post-menopause, leaving women more susceptible to adverse cardiovascular events. In response to these gender-specific challenges, there is a pressing need for targeted investigations into treatment modalities and prevention strategies, especially tailored to address the needs of vulnerable subgroups. This includes overweight individuals, those grappling with reproductive health conditions, and individuals with a history of gestational diabetes mellitus (GDM). Developing and implementing targeted preventive interventions and intensified, sex-specific prevention approaches hold significant promise for mitigating risks and improving outcomes in these high-risk populations. Nevertheless, the realization of effective and gender-sensitive treatment strategies necessitates further exploration through rigorous clinical trials. By diving deeper into gender-specific nuances and needs, healthcare providers can better design and deploy tailored interventions that not only bridge existing gender disparities but also optimize outcomes and quality of life for individuals navigating the complexities of type 2 diabetes management. This comprehensive approach stands to revolutionize diabetes care, paving the way for more equitable and patient-centric healthcare delivery.
Keywords
Gender discrepancies, macrovascular complications, post-menopause, gestational diabetes mellitus
Introduction
Sex refers to the biological characteristics linked to femininity and masculinity, whereas gender is a social construct that divides people into men and women. Biological variations and social institutions work together to produce health inequities. Comprehending these intricacies is crucial in tackling healthcare disparities and advocating for comprehensive methods of well-being.1In several non-communicable illnesses, including diabetes, gender variations have a clinically important influence on the etiology, epidemiological research, diagnosis and therapy. To improve the basic and societal advantages of research, publishers, investors, and health organizations push for the inclusion of sex and gender concerns in all stages of scientific research. This endeavor presents a chance to enhance healthcare equality and maximize research results.2,3,4Diabetes affects men and women differently, with women having particular difficulties as they age. Nevertheless, males are the primary subject of diabetic research. Women may be under diagnosed because of increased postprandial hypoglycemia, especially those over 60. Improving diabetes diagnosis, care and treatment results for everyone depends on addressing gender-specific elements of the disease5.People with type 2 diabetes have lately seen gains in their longevity, regardless of gender, despite the ongoing financial load6.Males have a greater lifetime risk of type 2 diabetes, with notable differences across decades and between areas and genders. The pathogenesis, clinical presentation, diagnosis and treatment responses of type 2 diabetes are influenced by genetic and hormonal variables, which also account for the gender disparities in clinical outcomes.7,8 Sex hormone variations affect the risk of cardio metabolic diseases such as type 2 diabetes. The outcomes of type 2 diabetes are significantly influenced by gender variations in lifestyle choices, behavior patterns, and attitudes towards prevention and treatment.9 The purpose of this study is to shed light on the relationship between gender and diabetes by exploring inequities, identifying risk factors and analyzing the consequences for healthcare. Illustration of gender specific complication is shown in fig 1

Fig. 1. Illustration of the most important sex differences in the complications that occurs in specific gender during diabetes. Diabetes is one of the major endocrinological disorder in world which shows the need of gender specific medicine which are important and can lead to different paths and treatments for many diseases, with certain traits being especially important in influencing the results of many different types of diseases.
ETIOLOGY
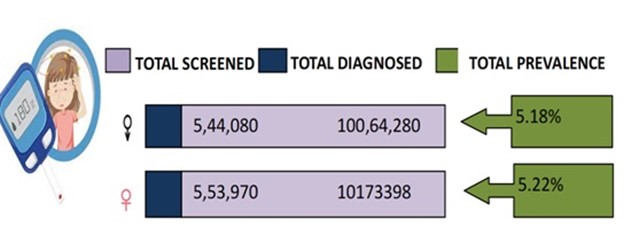
Pacific Islanders, Asian Indians, and Native Americans are more likely to acquire type 2 diabetes, which is a worldwide health problem. From the 1990s to the 21st century, the prevalence of type 2 diabetes has been raising rapidly worldwide.10 The International Diabetes Federation (IDF) estimates that 8.8% of adults worldwide have diabetes, with men having slightly higher rates than women (around 9.6% versus 9.0%). Global estimates for the current year show that 463 million people worldwide have diabetes, and 374 million have impaired glucose tolerance (IGT), a form of pre-diabetes. By 2045, there will likely be 700 million people with diabetes worldwide, of which 548 million will have insulin-dependent diabetes (IGT), a 51% increase from 2019.11 As per the International Diabetes Federation (IDF), the top three countries with the largest number of diabetics in 2019 were China (116.4 million), India (77.0 million), and the United States of America (31.0 million). According to projections, the countries with the greatest diabetes burdens would be China (140.5 million and 147.2 million) and India (101.0 million and 134.2 million) by 2030 and 2045, respectively. The Global Burden of Disease Study emphasizes that in key global countries like China and India, the absolute number of people with diabetes is rising as a result of population growth and aging.12 Graphical representations of gender specific statistics is shown in fig 2.
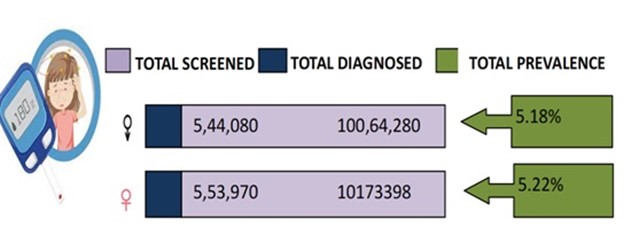
Fig. 2. This figure represents the number of patients screened and number of patients diagnosed with diabetes in this we can illustrate that compared to female, male has more prevalence in developing diabetes.
BURDEN OF DIABETES IN INDIA
Worldwide, the prevalence of diabetes has increased over the past 30 years, with India bearing a disproportionate share of the burden. An epidemic has caused changes in disease patterns, including a decrease in the death rate from communicable illnesses and an increase in non-communicable diseases (NCDs) and the effect of injuries. Compared to 30% for non-communicable illnesses and 9% for accidents, communicable diseases accounted for 61% of disability adjusted life years (DALYs) in India in 1990. Injuries decreased to 12% and NCDs to 55% by 2016, while DALYs from communicable diseases decreased to 33%. The DALY rate increased fourfold in those with diabetes in particular. Most NCDs have increased since1990; by 2016, diabetes has moved up from 35th to 13th in the DALY rankings.13
RISK FACTORS OF DIABETES BASED ON GENDER
INSULIN RESISTANCE
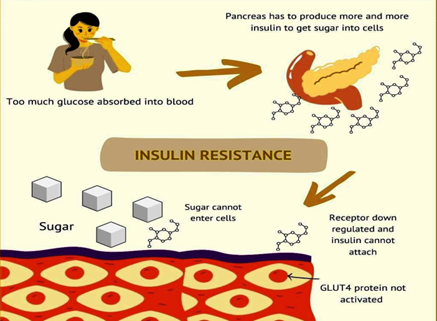
Research shows that before to menopause, women usually have greater skeletal muscle mass, increased insulin production in the liver, and accelerated insulin synthesis. Women's HbA1c and fasting glucose levels are lower than men's due to these reasons.14 Menopause is accompanied by increases in LDL cholesterol, blood pressure and glycated hemoglobin (HbA1c) levels. Un favorable distributional changes in body fat make glucose intolerance (IGT) worse. The physiological benefits that women experience decrease as insulin growth results from proper glucose tolerance (GLT).15 When compared to males of the same age, older women with normoglycemia usually show a ~20% greater glucagon-like peptide-1 (GLP-1) response during an oral glucose tolerance test (OGTT). However, women generate less GLP-1 than males do when they have type-2 diabetes, impaired glucose tolerance (IGT), or impaired fasting glucose (IFG). This shows that gender differences may be involved in modifying GLP-1 levels when women's glucose tolerance diminishes.16 Furthermore, the risks of cardiovascular disease (CVD) and total mortality are comparable for young women with over type-2 diabetes and males17. Studies have indicated that women diagnosed with type-2 pre-diabetes are at an increased risk of elevated stress levels and key metabolic risk factors. Changes in body mass index, body fat percentage, fasting blood glucose levels, and lipid profiles are some of these causes.18, 19 It is important to note that, particularly in younger women, especially those who are premenopausal, a diagnosis of non-alcoholic fatty liver disease (NAFLD) increases the likelihood of predicting type 2 diabetes.20 Type 2 diabetes and severe non-alcoholic fatty liver disease (NAFLD) in young girls are tightly associated, suggesting a greater risk in females. NAFLD is more common in women who have hypoglycemia because of serious metabolic risk factors.21 Insulin resistance cycle is represented in fig 3.
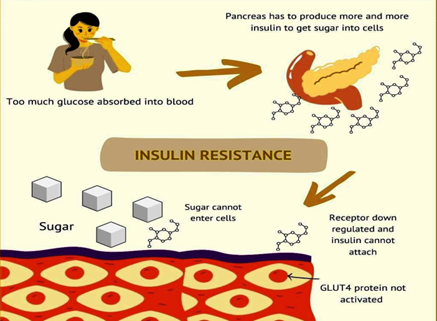
FIG 3: This figure represents cycle of insulin resistance which occurs during diabetes. In people with insulin resistance, cells in muscles, body fat, and the liver start resisting, or ignoring, insulin’s signal to absorb glucose from the bloodstream and transport it into cells. When this happens, glucose essentially gets stuck in the bloodstream, as it’s unable to enter the cells. This causes blood sugar levels to rise and causes fatigue and tired due to which they feel hungry again.
EFFECT OF ENDOCRINE
The primary purpose of the hormones that control sex is to Diabetes mellitus associated with sexual dimorphism 15, 22, 23.Premenopausal women's estrogen increases insulin sensitivity and production, preventing diabetes. Because early menopause lowers estrogen levels, diabetes risk increases. Hormone replacement medication can make treating diabetes more difficult, even while it helps with menopausal symptoms.23, 24 Male hormones like testosterone affect insulin sensitivity and the absorption of glucose by cells via controlling glucose metabolism, male and female metabolic results differ in part because of this.25 Men's testosterone levels improve the function of GLP-1, lower inflammation for the health of cells, and raise insulin release when glucose is present. In males with type 2 diabetes, there is an independent correlation between mortality and high sex hormone binding globulin (SHBG) levels and low free testosterone.26 The health effects of elevated levels of SHBG are attributed to tissue availability reduction and testosterone bioactivity modulation. On the other hand, insulin resistance and the onset of type 2 diabetes are linked to low SHBG levels.15 The association between intra hepatic fat storage and type 2 diabetes is mediated by SHBG, with a greater effect shown in females.27 Conversely, increased testosterone levels in females cause oxidative stress, beta cell malfunction, insulin hyper secretion, and mitochondrial dysfunction.25As a result, type 2 diabetes is more common in males with low testosterone levels. On the other hand, women who have high amount of testosterone are more likely to develop type 2 diabetes. Evidence of this association may be seen in the up to four-fold increased likelihood of glucose swings in women with polycystic ovarian syndrome (PCOS) and excess testosterone.15,28It is significant that studies have shown that SHBG, obesity and testosterone levels are the main determinants of PCOS. Nevertheless, neither type 2 diabetes nor cardiovascular disease CVD is directly brought on by PCOS.29 Intramuscular testosterone therapy, as opposed to a placebo, decreased or reversed type 2 diabetes in overweight guys aged 50 to 74 who had low testosterone levels or poor glucose tolerance by 41% over the course of two years. Males with type 2 diabetes who are obese and have low testosterone levels should think about the advantages and disadvantages of testosterone supplementation. It is also important to screen for hypogonadism in these individuals.30
EFFECT DURING PREGNANCY
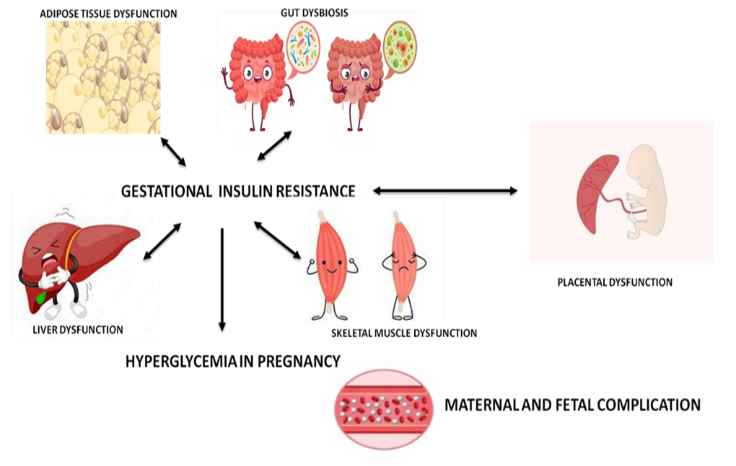
Pregnant women may exhibit mild underlying metabolic disorders, which can lead to a high rate of gestational diabetes mellitus (GDM) development, ranging from 5% to 16% in women.15 The majority of women who have GDM, an atypical illness, are obese and insulin-resistant. But skinny women with low beta cell counts could also be impacted since their ability to compensate for pregnancy-induced insulin resistance may be diminished.31 GDM diagnosis rates are greater in older women and in several ethnic groups. However, variations in screening techniques, genetic origins, body composition, weight gain and cultural standards all contribute to diagnostic variability.32 GDM particularly in females, is one of the major risk factors for the development of type 2 diabetes. A recent meta-analysis found that the relative risk (RR) of type 2 diabetes in women with GDM is 8.3 (95% CI 6.5, 10.6). In comparison to women from other groups, the yearly increase in type 2 diabetes diagnoses following pregnancy is 12%. During follow-up, the diagnostic rate rises by 18% per BMI unit, and in white European women, it decreases by 57%.33,34 Intervention strategies alongside diabetes prevention efforts effectively reduce type 2 diabetes prevalence. However, many women with a history of GDM develop type 2 diabetes. Even those with prediabetes or normo glycemia who had previous pregnancies still have a 70% higher GDM prevalence over three years.35 Women at high risk for gestational diabetes should start preventative programs and continue to check their blood sugar levels. Type 2 pre gestational diabetes, which is currently the most prevalent kind worldwide, has significantly increased due in part to the global increase in obesity.36The most thorough analysis of these pregnancies found difficulties in maintaining glycemic control during pregnancy, low rates of contraceptive usage, poor preconception care, subpar glycemic control, a greater prevalence of co morbidities, and pregnancy-related problems.37 The illness caused intrauterine mortality in one out of every four mothers. Thus, improved and individualized prenatal care is especially important for young girls with early-onset type 2 diabetes, as is preconception counseling. The diagrammatic representation of GDM is given in fig 4.
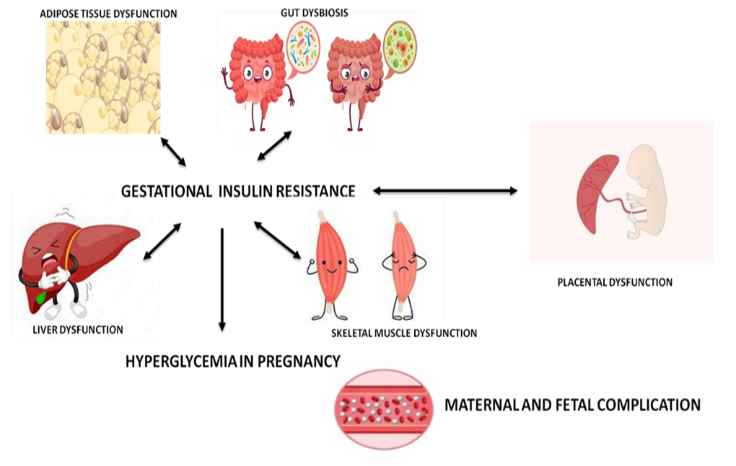
Fig. 4. This diagram represents gestational diabetes and influence of liver adipose and placental dysfunction how it effects on glucose uptake during pregnancy.
PHYSIOLOGICAL FACTOR
Particularly for women, low income, low social and occupational standing and little education are significant risk factors for the development of type 2 diabetes.38,39 Especially for men in industrialized countries, a rise in family wealth has a higher effect on lowering the risk of type 2 diabetes and positively correlates with its incidence rates.40 Income has a complex relationship with type 2 diabetes that varies by country and is impacted by the Human Development Index (HDI).15 Women's attempts to prevent and cure type 2 diabetes are hampered by limited access to healthcare in developing countries because of issues with infrastructure, finances, cultural norms, and public awareness. Empowering women, expanding access to healthcare, and boosting diabetes education via teamwork are the solutions.41 High perceived stress levels are strongly linked to an increased risk of diabetes, particularly in males, according to research conducted in Japan. This emphasizes how important it is for diabetes preventive and management programs to include thorough stress management techniques.42 Diabetes is less common in males who have demanding occupations and satisfying positions, but type 2 diabetes in women is associated with a lack of decision-making authority. This discrepancy highlights the intricate relationship between work-related factors and health outcomes, emphasizing the need for focused measures to lessen workplace stress, particularly in the case of women's health.15,43 Anxiety and low self-efficacy are closely correlated with sedentary behavior, particularly in women with type 2 diabetes. For these women, increasing physical activity and decreasing time spent inactive can have a major positive impact on mental health outcomes.44 Long nights increase the risk of type 2 diabetes by (1.46), especially in women. Additionally, female shift workers are more vulnerable. Given the gender-specific impact of lengthy night shifts on the development of type 2 diabetes, this emphasizes the significance of taking these factors into account in programs aimed at preventing diabetes and improving occupational health for women46.In conclusion, women are more likely than males to develop type 2 diabetes as a result of psychological risk factors. It is imperative that metabolic disorders be screened for early, especially in women, to lower the incidence of type 2 diabetes. Strategies tailored to the gender of the patient are crucial for controlling and avoiding diabetes and related health problems.47, 48 Women are more likely to suffer from depression, particularly after menopause. Women with type 2 diabetes frequently have greater rates of melancholy and participate in less activities that focus on finding solutions, which has an impact on their self-care. Treating mental health issues such as depression is essential for women with type 2 diabetes to effectively manage their self-care.49 Women are more likely to suffer from depression, particularly after menopause. Women with type 2 diabetes frequently have greater rates of melancholy and participate in less activities that focus on finding solutions, which has an impact on their self-care. Treating mental health issues such as depression is essential for women with type 2 diabetes to effectively manage their self-care.50
For an efficient diagnosis and care that is treatment-focused, it is essential to distinguish between pre diabetes and diabetic distress. This strategy may enhance type 2 diabetes patients results and medication compliance while offering complete support for both diabetes management and general well-being.
MICROVASCULAR COMPLICATION
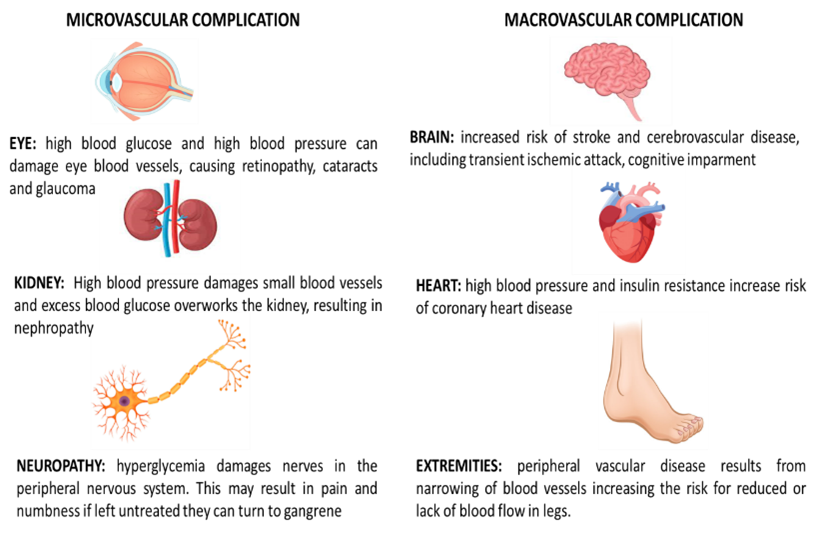
Evidence for gender difference in micro vascular disease is sparse and inconclusive men with type 2 diabetes who have higher risk of sensory neuropathy, nephropathy and worse retinal microvascular parameters than men with normoglycemia, as it is not evident in women. However, in patient with type 2 diabetes have greater risk of renal failure when compared with women. Women with diabetes mellitus have more neuropathic pain and nerve injury than men. More recently no gender difference has been observed in diabetic retinopathyrepresented in fig 5.
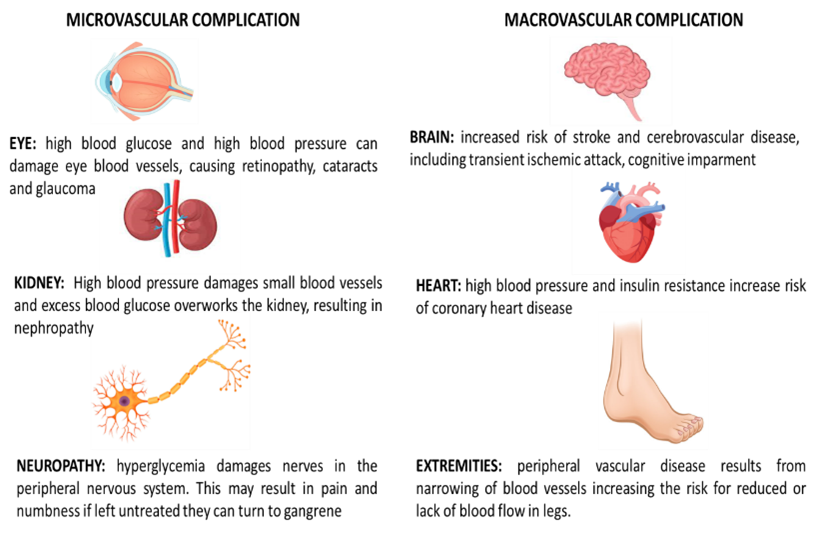
Fig. 5. This figure illustrates the major microvascular and macrovascular complication caused during diabetes and their effect.
MACROVASCULAR COMPLICATION
For both men and women, CVD is the main cause of death, and type 2 diabetes increases the risk of dying young. The effect of diabetes on the risk of CVD varies by gender. Understanding these differences enables treatments to be more suited for desired results.15, 31 Type 2 diabetes increases the absolute risk of dying from CVD in males, but it dramatically increases the RRof CVD mortality in women. These differences draw attention to the gender-specific factors that should be taken into account when evaluating and controlling cardiovascular risk in people with type 2 diabetes.,23,31,51 Independent research, however, found that the sexes were comparable.53 Type 2 diabetes and not sex dimorphism were found to have causal impacts on the risk of coronary heart disease (CHD) in a recent Mendelian randomization analysis (MRA). This implies that gender variations have no effect on the relationship between type 2 diabetes and the risk of CHD.54 The higher risk of death linked to type 2 diabetes is most noticeable in women between the ages of 35 and 59. Particularly in this age range, type 2 diabetes has a significant negative influence on death rates. Therefore, early detection and focused healthcare measures are crucial.52 Particularly for women, who have a higher incidence of type 2 diabetes and are more likely than men to be diagnosed with advanced atherosclerosis at onset, early screening and intervention strategies are essential for managing diabetes-related complications and lowering the risk of unfavorable outcomes associated with advanced atherosclerosis and other CVDs.55 Adolescent female obesity exacerbates cardio metabolic risk factors and is associated with the emergence of type 2 diabetes. It is essential to implement weight management and lifestyle modifications at an early age to lower the risk of type-2 diabetes and related health issues.30 Females had higher subclinical inflammation and coagulopathy starting in early adulthood, even in cases of acute dysglycemia. Early treatment of women with dysglycemia is essential to lower the risk of cardiovascular issues and other unfavorable health effects related to these physiological alterations.31 Younger women with type 2 diabetes are more likely to develop CVD because of coagulopathy linked to dysglycemia and inflammation. Effective prevention and treatment of CVDs in this population depend on the early identification and control of these variables.54, 56 Women with type 2 diabetes have higher cardiovascular risk factors after menopause. Treatments tailored to each patient's gender are necessary to lower the death rate from heart disease.57 Women with type 2 diabetes have higher cardiovascular risk factors after menopause. Treatments tailored to each patient's gender are necessary to lower the death rate from heart disease.54 Heart problems are more common in women with type 2 diabetes because they frequently take their cardiovascular medications less religiously than men do. Customized care is essential for improved adherence and health results.58 Compared to males, women with type 2 diabetes or impaired glucose tolerance (IGT) frequently overlook controlling blood pressure, LDL cholesterol, and exercise, which raises their risk of CVD. Personalized care is necessary to enhance women's cardiovascular risk reduction.59
DISPARITIES BETWEEN THE SEXES IN PHARMACEUTICAL THERAPY AND MANAGEMENT
There is little data on how lifestyle changes affect men's and women's cardio metabolic health. Males may lose weight and fat more quickly than females, which might increase the total advantages of cardio metabolic processes. To comprehend gender-specific reactions and adjust therapies appropriately more research is required.15,60 After two years, men in direct weight management programs exhibit longer-lasting type 2 diabetes remissions, perhaps as a result of their larger weight loss. Personalized treatments and continued assistance are essential for long-term health gains, especially in men with type 2 diabetes.61 Gender discrepancies in treatment techniques lead to under treatment of women with type 2 diabetes, which in turn contributes to disparities in health outcomes. To overcome this difference and guarantee the best care possible for women with type 2 diabetes, customized treatment programs and increased access to care are crucial.62 Metformin is frequently recommended to reduce blood sugar levels, however research indicates that women may take this prescription less religiously than males. For women with type 2 diabetes to experience better results, it is imperative to address medication adherence concerns and customize treatment regimens. 34,63 Research has shown that, even with the same bioavailability, men's HbA1c levels decline more than women's do. This highlights the need for more study to comprehend and resolve these discrepancies in diabetes care and raises the possibility of gender-specific variations in treatment responsiveness.65 Metformin treatment and lifestyle modifications provide robust protection against the development of type 2 diabetes in women with a history of gestational diabetes mellitus. This emphasizes how crucial early intervention is to stop or postpone the emergence of type 2 diabetes in this population.66 Medication containing SGLT-2 inhibitors improves glucose metabolism more in men than in women. Men with type 2 diabetes use it more often than women, despite the fact that it lowers the risk of renal and heart disease. Comprehending how gender reacts to therapy is essential to ensuring that everyone has fair access to high-quality care.67, 68 A gender-pooled meta-analyses found that SGLT-2 inhibitors (SGLT-2Is) provide comparable cardiovascular benefits in both men and women with type 2 diabetes. This demonstrates how well they work to improve heart health in both sexes.69 Regardless of gender or type 2 diabetes statuses, people with heart failure with preserved ejection fraction (HFpEF) had comparable cardiovascular benefits and a lower chance of dying from cardiovascular disease. This implies that some medications, independent of gender or diabetes status, have benefits that are similar for people with HFpEF.70 Dapagliflozin shows promise as a therapy option for people with HFpEF or moderately improved heart failure, independent of gender, since it helps both male and female patients.71 The outcome was probably impacted by the larger proportion of women, including those with the highest ejection %. Furthermore, evidence points to a higher incidence of UTIs and vaginal infections among female SGLT-2 inhibitor users.72 Comparable safety and efficacy for men and women was shown by a recent investigation that identified no gender differences in blood flow efficacy, amputation risk, fracture risk, urinary tract infections, or vaginal infections among treated patients.69 Women's risks of fracture and ketoacidosis have been linked to canagliflozin use; this emphasizes the significance of careful patient monitoring and taking risk factors into account, particularly for female patients. Healthcare professionals should carefully consider the advantages and disadvantages of canagliflozin therapy, especially for women who are more likely to experience fractures or ketoacidosis, and look into other treatment alternatives.73,74 GLP-1 receptor agonists, or GLP-1RAs, frequently cause women to lose more weight than males. Healthcare professionals who provide GLP-1RA medicines to patients with type 2 diabetes should take these gender-specific reactions into account.49, 75-78 Even though different GLP-1RAs consistently lower HbA1c levels, there are gender-specific variations in how the body reacts to these drugs. GLP-1RA therapy usually results in more weight reduction in women than in men. This emphasizes the significance of gender-specific treatment strategies to maximize type 2 diabetes patients’ outcomes.75,77 For female patients with type 2 diabetes, the combination of eventide with metformin seems to be very beneficial, providing better glucose control and weight management. Combination treatment targets several mechanisms related to metabolic control and glucose management, offering encouraging outcomes for females with type 2 diabetes.Gastrointestinal side effects are a typical adverse effect of GLP-1 receptor agonists (GLP-1RAs), and they are more common in women. There might be vomiting, diarrhea, and nausea. It is essential to continuously evaluate and manage treatment-related symptoms, particularly in females with type 2 diabetes who are using GLP-1RAs. Modifications in the amount or timing of medications may reduce gastrointestinal distress and improve treatment compliance and efficacy.49 Gliptin treatment for type 2 diabetes patients does not appear to affect HbA1c reduction or major adverse cardiovascular events (MACE) differently depending on a patient's gender. Gliptins are safe and effective for both men and women, as evidenced by their constant advantages for cardiovascular health and glycemic management in both genders.81 The main points of the paper should be summarized and explained to the reader in the conclusion of the research paper. Although conclusions do not usually give new information that has not been included in the article, they frequently recast questions or provide a fresh perspective on an issue.82 The study highlights the higher risk of hypoglycemia in males with normal body weight diabetes who receive pre-mixed insulin after continuous subcutaneous insulin infusion (CSII), especially in Asian patients. Individualized diabetes care must emphasize customized techniques for a variety of patient demographics, taking gender, weight, and ethnicity into account to maximize treatment results. 83 Normal-weight women might need to watch how they regulate their insulin. The efficacy and safety of type 2 diabetes drugs, such as statins, ACE inhibitors, and ARNIs, vary depending on the gender. For the management of type 2 diabetes and associated complications, individualized treatment programs are crucial.47 The risk of melancholy and osteoporosis associated with higher medicine doses is particularly high in postmenopausal women. This emphasizes the importance of glycemic control and overall health outcomes while managing type 2 diabetes through dosage evaluation. To balance the advantages and disadvantages of medicine, careful observation and individualized care are crucial.84,85
FUTURE PERSPECTIVE
Research on gender and sex differences is crucial for understanding the psychological effects and scientific foundations of type 2 diabetes, enabling more personalized care based on gender, sex, age, and ethnicity. Raising awareness among high risk populations, like younger patients and people of colour, is essential, particularly when glycaemic control deviates from target ranges. Customized screenings and therapies are imperative, especially for those with lower body mass indexes or early-onset type 2 diabetes, to prevent cardiovascular complications. Key strategies for women include weight management, cardio-renal medications, and lifestyle changes, with a focus on controlling blood pressure in obese women to reduce cardiovascular risks. Healthcare providers must address risk factors early to mitigate arterial co morbidities, especially in women who may have shorter treatment windows. Multi factorial treatment adhering to guidelines is essential for all individuals with type 2 diabetes, but stress and diabetes-related anxiety, particularly in women, hinder self-care. Enhanced screening tools, mental health support, and gender-specific research are needed to address these challenges. Public education initiatives can increase awareness about type 2 diabetes and its management, prioritizing gender-sensitive strategies for improved outcomes.
CONCLUSIONS
Type 2 diabetes is influenced by gender variations in its onset, complications, and management. Because of hormonal fluctuations, women with type 2 diabetes are more likely to experience cardiovascular problems, particularly after menopause. For sensitive populations, such as overweight people and those with a history of gestational diabetes, customized preventative interventions are required. To create specialized type 2 diabetes treatment plans depending on gender and other variables, more investigation and testing are required.
REFERENCES
- Marino, M.; Masella, R.; Bulzomi, P.; Campesi, I.; Malorni, W. and Franconi, F. (2011) Nutrition and human health from a sexgender perspective. Mol. Aspects Med., 32(1), 1-70
- Schiebinger L, Klinge I, Sánchez de Madariaga I, Paik H, Schraudner M, Stefanick M. Gendered innovations in science, health & medicine, engineering, and environment. 2011-2017. http://genderedinnovations.stanford.edu/index.html (accessed 31- 01-2018).
- Heidari S, Babor TF, de Castro P, Tort S, Curno M. Sex and Gender Equity in Research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 2016; 1(2).
- Canadian Institutes of Health Research. Sex, gender and health research guide: a tool for CIHR applicants. 2018. http://www.cihrirsc.gc.ca/e/32019.html (accessed 01-02-2018).
- DECODE Study Group (2003) Age- and sex-specific prevalences of diabetes and impaired glucose regulation in 13 European cohorts. Diabetes Care 26(1):61–69. https://doi.org/10.2337/ diacare.26.1.61
- . Tomic D, Morton JI, Chen L et al (2022) Lifetime risk, life expectancy, and years of life lost to type 2 diabetes in 23 high-income jurisdictions: a multinational, population-based study. LancetDiabetes Endocrinol 10(11):795–803. https://doi.org/10.1016/ S2213-8587(22)00252-2
- Kautzky-Willer A, Harreiter J, Pacini G (2016) Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev 37(3):278–316. https://doi.org/10. 1210/er.2015-1137
- Mauvais-Jarvis F, Bairey Merz N, Barnes PJ et al (2020) Sex and gender: modifiers of health, disease, and medicine. Lancet 396(10250):565–582. https://doi.org/10.1016/S0140-6736(20) 31561-0
- Nielsen MW, Stefanick ML, Peragine D et al (2021) Genderrelated variables for health research. Biol Sex Differ 12(1):23. https://doi.org/10.1186/s13293-021-00366-3
- Mohan V, Pradeepa R. The Global Burden of Diabetes and Its Vascular Complications (Chapter 1). In: Mechanisms of Vascular Defects in Diabetes Mellitus. Advances in Biochemistry in Health and Disease. Kartha CC, Ramachandran S, Pillai RM (Eds). Springer International Publishing AG 2017. 2017; p. 3 – 23
- International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels, Belgium: International Diabetes Federation; 2019.
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011;378:31–40
- Indian Council of Medical Research, Public Health Foundation of India, and Institute for Health Metrics and Evaluation. India: Health of the Nation’s States - The India State-Level Disease Burden Initiative. New Delhi: ICMR, PHFI and IHME; 2017.Available from:https://www.healthdata.org/sites/default/files/files/policy_report/2017/India_Health_of_the_Nation's_States_ Report_2017.pdf.
- Goossens GH, Jocken JWE, Blaak EE (2021) Sexual dimorphism in cardiometabolic health: the role of adipose tissue, muscle and liver. Nat Rev Endocrinol 17(1):47–66. https://doi.org/10.1038/ s41574-020-00431-8.
- Kautzky-Willer A, Harreiter J, Pacini G (2016) Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev 37(3):278–316. https://doi.org/10. 1210/er.2015-1137
- Færch K, Torekov SS, Vistisen D et al (2015) GLP-1 response to oral glucose is reduced in prediabetes, screen-detected type 2 diabetes, and obesity and influenced by sex: the ADDITIONPRO study. Diabetes 64(7):2513–2525. https://doi.org/10.2337/ db14-1751
- Kautzky-Willer A (2021) Does diabetes mellitus mitigate the gender gap in COVID-19 mortality? Eur J Endocrinol 185(5): C13–C17. https://doi.org/10.1530/EJE-21-0721
- Ramezankhani A, Azizi F, Hadaegh F (2020) Sex differences in rates of change and burden of metabolic risk factors among adults who did and did not go on to develop diabetes: two decades of follow-up from the tehran lipid and glucose study. Diabetes Care 43(12):3061–3069. https://doi.org/10.2337/dc20-1112
- Du T, Fernandez C, Barshop R et al (2019) Sex differences in cardiovascular risk profile from childhood to midlife between individuals who did and did not develop diabetes at follow-up: the bogalusa heart study. Diabetes Care 42(4):635–643. https:// doi.org/10.2337/dc18-2029
- Kim Y, Chang Y, Ryu S, Wild SH, Byrne CD (2022) NAFLD improves risk prediction of type 2 diabetes: with effect modification by sex and menopausal status. Hepatology 76(6):1755–1765. https://doi.org/10.1002/hep.32560
- Succurro E, Marini MA, Fiorentino TV et al (2022) Sex-specific differences in prevalence of nonalcoholic fatty liver disease in subjects with prediabetes and type 2 diabetes. Diabetes Res Clin Pract 190:110027. https://doi.org/10.1016/j.diabres.2022.110027
- Tramunt B, Smati S, Grandgeorge N et al (2020) Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 63(3):453–461. https://doi.org/10.1007/s00125-019-05040-3
- Mauvais-Jarvis F, Clegg DJ, Hevener AL (2013) the role of estrogens in control of energy balance and glucose homeostasis. Endocr Rev 34(3):309–338. https://doi.org/10.1210/er.2012-1055
- Anagnostis P, Christou K, Artzouchaltzi AM et al (2019) early menopause and premature ovarian insufficiency are associated with increased risk of type 2 diabetes: a systematic review and meta-analysis. Eur J Endocrinol 180(1):41–50. https://doi.org/10. 1530/EJE-18-0602
- Xu W, Morford J, Mauvais-Jarvis F (2019) Emerging role of testosterone in pancreatic beta-cell function and insulin secretion. J Endocrinol 240(3):R97–R105. https://doi.org/10.1530/JOE-18- 0573
- Ramachandran S, Hackett GI, Strange RC (2019) Sex hormone binding globulin: a review of its interactions with testosterone and age, and its impact on mortality in men with type 2 diabetes. Sex Med Rev 7(4):669–678. https://doi.org/10.1016/j.sxmr.2019.06. 006
- Simons P, Valkenburg O, van de Waarenburg MPH et al (2023) Serum sex hormone-binding globulin is a mediator of the association between intrahepatic lipid content and type 2 diabetes: the Maastricht study. Diabetologia 66(1):213–222. https://doi.org/10. 1007/s00125-022-05790-7
- Escobar-Morreale HF (2018) polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol 14(5):270–284. https://doi.org/10.1038/nrendo.2018.24
- Zhu T, Goodarzi MO (2022) Causes and consequences of polycystic ovary syndrome: insights from mendelian randomization. J Clin Endocrinol Metab 107(3):e899–e911. https://doi.org/10. 1210/clinem/dgab757
- Wittert G, Bracken K, Robledo KP et al (2021) Testosterone treatment to prevent or revert type 2 diabetes in men enrolled in a lifestyle programme (T4DM): a randomised, double-blind, placebo-controlled, 2-year, phase 3b trial. Lancet Diabetes Endocrinol 9(1):32–45. https://doi.org/10.1016/S2213-8587(20)30367-3
- Harreiter J, Fadl H, Kautzky-Willer A, Simmons D (2020) Do women with diabetes need more intensive action for cardiovascular reduction than men with diabetes? Curr Diab Rep 20(11):61. https://doi.org/10.1007/s11892-020-01348-2
- Yuen L, Wong VW, Simmons D (2018) Ethnic disparities in gestational diabetes. Curr Diab Rep 18(9):68. https://doi.org/10. 1007/s11892-018-1040-2
- McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P (2019) Gestational diabetes mellitus. Nat Rev Dis Primers 5(1):47. https://doi.org/10.1038/s41572-019-0098-8
- Dennison RA, Chen ES, Green ME et al (2021) the absolute and relative risk of type 2 diabetes after gestational diabetes: A systematic review and meta-analysis of 129 studies. Diabetes Res Clin Pract 171:108625. https://doi.org/10.1016/j.diabres.2020.108625
- Ratner RE, Christophi CA, Metzger BE et al (2008) Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab 93(12):4774–4779. https://doi.org/10.1210/jc.2008-0772
- Murphy HR, Moses RG (2022) Pregnancy outcomes of young women with type 2 diabetes: poor care and inadequate attention to glycemia. Diabetes Care 45(5):1046–1048. https://doi.org/10. 2337/dci21-0059
- Today Study Group (2021) Pregnancy outcomes in young women with youth-onset type 2 diabetes followed in the TODAY study. Diabetes Care 45(5):1038–1045. https://doi.org/10.2337/dc21- 1071
- Kautzky-Willer A, Dorner T, Jensby A, Rieder A (2012) Women show a closer association between educational level and hypertension or diabetes mellitus than males: a secondary analysis from the Austrian HIS. BMC Public Health 12:392. https://doi.org/10. 1186/1471-2458-12-392
- Rivera LA, Lebenbaum M, Rosella LC (2015) The influence of socioeconomic status on future risk for developing Type 2 diabetes in the Canadian population between 2011 and 2022: differential associations by sex. Int J Equity Health 14:101. https://doi.org/ 10.1186/s12939-015-0245-0
- Wu H, Bragg F, Yang L et al (2019) Sex differences in the association between socioeconomic status and diabetes prevalence and incidence in China: cross-sectional and prospective studies of 0.5 million adults. Diabetologia 62(8):1420–1429. https://doi.org/10. 1007/s00125-019-4896-z
- The Lancet Diabetes Endocrinology (2017) Sex disparities in diabetes: bridging the gap. Lancet Diabetes Endocrinol 5(11): 839. https://doi.org/10.1016/S2213-8587(17)30336-4
- Kato M, Noda M, Inoue M, Kadowaki T, Tsugane S (2009) Psychological factors, coffee and risk of diabetes mellitus among middle-aged Japanese: a population-based prospective study in the JPHC study cohort. Endocr J 56(3):459–468. https://doi.org/ 10.1507/endocrj.k09e-003
- Eriksson AK, van den Donk M, Hilding A, Ostenson CG (2013) Work stress, sense of coherence, and risk of type 2 diabetes in a prospective study of middle-aged Swedish men and women. Diabetes Care 36(9):2683–2689. https://doi.org/10.2337/dc12- 1738
- Indelicato L, Dauriz M, Bacchi E et al (2018) Sex differences in the association of psychological status with measures of physical activity and sedentary behaviour in adults with type 2 diabetes. Acta Diabetol 55(6):627–635. https://doi.org/10.1007/s00592- 018-1132-0
- Silva-Costa A, Rotenberg L, Toivanen S et al (2020) Lifetime night work exposure and the risk of type 2 diabetes: results from the longitudinal study of adult health (ELSA-Brasil). Chronobiol Int 37(9-10):1344–1347. https://doi.org/10.1080/07420528.2020. 1804923
- Gao Y, Gan T, Jiang L et al (2020) Association between shift work and risk of type 2 diabetes mellitus: a systematic review and doseresponse meta-analysis of observational studies. Chronobiol Int 37(1):29–46. https://doi.org/10.1080/07420528.2019.1683570
- Kautzky-Willer A, Thurner S, Klimek P (2017) Use of statins offsets insulin-related cancer risk. J Intern Med 281(2):206–216. https://doi.org/10.1111/joim.12567
- Deischinger C, Dervic E, Leutner M et al (2020) Diabetes mellitus is associated with a higher risk for major depressive disorder in women than in men. BMJ Open Diabetes Res Care 8(1). https:// doi.org/10.1136/bmjdrc-2020-001430
- Kautzky-Willer A, Harreiter J (2017) Sex and gender differences in therapy of type 2 diabetes. Diabetes Res Clin Pract 131:230– 241. https://doi.org/10.1016/j.diabres.2017.07.012
- Perrin NE, Davies MJ, Robertson N, Snoek FJ, Khunti K (2017) The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med 34(11):1508–1520. https://doi.org/10.1111/dme. 13448
- Huxley R, Barzi F, Woodward M (2006) Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 332(7533):73–78. https://doi.org/10.1136/bmj.38678.389583.7C
- Prospective Studies Collaboration, Asia Pacific Cohort Studies Collaboration (2018) Sex-specific relevance of diabetes to occlusive vascular and other mortality: a collaborative meta-analysis of individual data from 980 793 adults from 68 prospective studies. Lancet Diabetes Endocrinol 6(7):538–546. https://doi.org/10. 1016/S2213-8587(18)30079-2
- Wright AK, Kontopantelis E, Emsley R et al (2019) Cardiovascular risk and risk factor management in type 2 diabetes mellitus. Circulation 139(24):2742–2753. https://doi.org/10. 1161/CIRCULATIONAHA.118.039100
- Peters TM, Holmes MV, Richards JB et al (2021) Sex differences in the risk of coronary heart disease associated with type 2 diabetes: a mendelian randomization analysis. Diabetes Care 44(2): 556–562. https://doi.org/10.2337/dc20-1137
- Mauvais-Jarvis F, Bairey Merz N, Barnes PJ et al (2020) Sex and gender: modifiers of health, disease, and medicine. Lancet 396(10250):565–582. https://doi.org/10.1016/S0140-6736(20) 31561-0
- Malmborg M, Schmiegelow MDS, Norgaard CH et al (2020) Does type 2 diabetes confer higher relative rates of cardiovascular events in women compared with men? Eur Heart J 41(13):1346– 1353. https://doi.org/10.1093/eurheartj/ehz913
- Hu G, Decode Study Group (2003) Gender difference in all-cause and cardiovascular mortality related to hyperglycaemia and newly-diagnosed diabetes. Diabetologia 46(5):608–617. https:// doi.org/10.1007/s00125-003-1096-6
- Clemens KK, Woodward M, Neal B, Zinman B (2020) Sex disparities in cardiovascular outcome trials of populations with diabetes: a systematic review and meta-analysis. Diabetes Care 43(5):1157–1163. https://doi.org/10.2337/dc19-2257
- Ferrannini G, De Bacquer D, Vynckier P et al (2021) Gender differences in screening for glucose perturbations, cardiovascular risk factor management and prognosis in patients with dysglycaemia and coronary artery disease: results from the ESCEORP EUROASPIRE surveys. Cardiovasc Diabetol 20(1):38. https://doi.org/10.1186/s12933-021-01233-6
- Harreiter J, Kautzky-Willer A (2018) Sex and gender differences in prevention of type 2 diabetes. Front Endocrinol (Lausanne) 9: 220. https://doi.org/10.3389/fendo.2018.00220
- Thom G, Messow CM, Leslie WS et al (2021) Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabet Med 38(8):e14395. https://doi.org/10.1111/ dme.14395
- Manteuffel M, Williams S, Chen W, Verbrugge RR, Pittman DG, Steinkellner A (2014) Influence of patient sex and gender on medication use, adherence, and prescribing alignment with guidelines. J Womens Health (Larchmt) 23(2):112–119. https://doi.org/ 10.1089/jwh.2012.3972
- Nakayama Y, Yamaguchi S, Shinzato Y et al (2021) Retrospective exploratory analyses on gender differences in determinants for incidence and progression of diabetic retinopathy in Japanese patients with type 2 diabetes mellitus. Endocr J 68(6):655–669. https://doi.org/10.1507/endocrj.EJ20-0630
- Pongwecharak J, Tengmeesri N, Malanusorn N, Panthong M, Pawangkapin N (2009) Prescribing metformin in type 2 diabetes with a contraindication: prevalence and outcome. Pharm World Sci 31(4):481–486. https://doi.org/10.1007/s11096-009-9303-2
- Schütt M, Zimmermann A, Hood R et al (2015) Gender-specific effects of treatment with lifestyle, metformin or sulfonylurea on glycemic control and body weight: a german multicenter analysis on 9 108 patients. Exp Clin Endocrinol Diabetes 123(10):622– 626. https://doi.org/10.1055/s-0035-1559608
- Aroda VR, Christophi CA, Edelstein SL et al (2015) The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab 100(4):1646–1653. https:// doi.org/10.1210/jc.2014-3761
- Funck KL, Bjerg L, Isaksen AA, Sandbaek A, Grove EL (2022) Gender disparities in time-to-initiation of cardioprotective glucose-lowering drugs in patients with type 2 diabetes and cardiovascular disease: a Danish nationwide cohort study. Cardiovasc Diabetol 21(1):279. https://doi.org/10.1186/s12933- 022-01713-3
- Eberly LA, Yang L, Eneanya ND et al (2021) Association of race/ethnicity, gender, and socioeconomic status with sodiumglucose cotransporter 2 inhibitor use among patients with diabetes in the US. JAMA Netw Open 4(4):e216139. https://doi.org/10. 1001/jamanetworkopen.2021.6139
- Rådholm K, Zhou Z, Clemens K, Neal B, Woodward M (2020) Effects of sodium-glucose co-transporter-2 inhibitors in type 2 diabetes in women versus men. Diabetes, ObesMetab 22(2): 263–266. https://doi.org/10.1111/dom.13876
- Butler J, Filippatos G, Siddiqi TJ et al (2022) Effects of empagliflozin in women and men with heart failure and preserved ejection fraction. Circulation 146(14):1046–1055. https://doi.org/10.1161/ CIRCULATIONAHA.122.059755
- Solomon SD, McMurray JJV, Claggett B et al (2022) Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 387(12):1089–1098. https://doi. org/10.1056/NEJMoa2206286
- Johnsson KM, Ptaszynska A, Schmitz B, Sugg J, Parikh SJ, List JF (2013) Vulvovaginitis and balanitis in patients with diabetes treated with dapagliflozin. J Diabetes Complicat 27(5):479–484. https://doi.org/10.1016/j.jdiacomp.2013.04.012
- Fadini GP, Bonora BM, Avogaro A (2017) SGLT2 inhibitors and diabetic ketoacidosis: data from the FDA Adverse Event Reporting System. Diabetologia 60(8):1385–1389. https://doi. org/10.1007/s00125-017-4301-8
- Zhou Z, Jardine M, Perkovic V et al (2019) Canagliflozin and fracture risk in individuals with type 2 diabetes: results from the CANVAS Program. Diabetologia 62(10):1854–1867. https://doi. org/10.1007/s00125-019-4955-5
- Gallwitz B, Dagogo-Jack S, Thieu V et al (2018) Effect of onceweekly dulaglutide on glycated haemoglobin (HbA1c) and fasting blood glucose in patient subpopulations by gender, duration of diabetes and baseline HbA1c. Diabetes ObesMetab 20(2):409– 418. https://doi.org/10.1111/dom.13086
- Anichini R, Cosimi S, Di Carlo A et al (2013) Gender difference in response predictors after 1-year exenatide therapy twice daily in type 2 diabetic patients: a real world experience. Diabetes Metab Syndr Obes 6:123–129. https://doi.org/10.2147/dmso.S42729
- Onishi Y, Oura T, Matsui A, Matsuura J, Iwamoto N (2017) Analysis of efficacy and safety of dulaglutide 0.75 mg stratified by sex in patients with type 2 diabetes in 2 randomized, controlled phase 3 studies in Japan. Endocr J 64(5):553–560. https://doi.org/ 10.1507/endocrj.EJ16-0552
- Quan H, Zhang H, Wei W, Fang T (2016) Gender-related different effects of a combined therapy of Exenatide and Metformin on overweight or obesity patients with type 2 diabetes mellitus. J Diabetes Complications 30(4):686–692. https://doi.org/10.1016/ j.jdiacomp.2016.01.013
- Singh AK, Singh R (2020) Gender difference in cardiovascular outcomes with SGLT-2 inhibitors and GLP-1 receptor agonist in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials. Diabetes Metab Syndr 14(3):181–187. https://doi.org/10.1016/j.dsx.2020.02.012
- D'Andrea E, Kesselheim AS, Franklin JM, Jung EH, Hey SP, Patorno E (2020) Heterogeneity of antidiabetic treatment effect on the risk of major adverse cardiovascular events in type 2 diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 19(1):154. https://doi.org/10.1186/s12933-020-01133-1
- Esposito K, Chiodini P, Maiorino MI et al (2015) A nomogram to estimate the HbA1c response to different DPP-4 inhibitors in type 2 diabetes: a systematic review and meta-analysis of 98 trials with 24 163 patients. BMJ Open 5(2):e005892. https://doi.org/10.1136/ bmjopen-2014-005892
- Owens DR, Landgraf W, Frier BM et al (2019) Commencing insulin glargine 100 U/mL therapy in individuals with type 2 diabetes: determinants of achievement of HbA1c goal less than 7.0. Diabetes ObesMetab 21(2):321–329. https://doi.org/10. 1111/dom.13607
- Li FF, Zhang Y, Zhang WL et al (2018) Male patients with longstanding type 2 diabetes have a higher incidence of hypoglycemia compared with female patients. Diabetes Ther 9(5):1969– 1977. https://doi.org/10.1007/s13300-018-0492-3
- Leutner M, Matzhold C, Bellach L et al (2019) Diagnosis of osteoporosis in statin-treated patients is dose-dependent. Ann Rheum Dis 78(12):1706–1711. https://doi.org/10.1136/annrheumdis2019-215714
- Leutner M, Matzhold C, Kautzky A et al (2021) Major Depressive Disorder (MDD) and antidepressant medication are overrepresented in high-dose statin treatment. Front Med (Lausanne) 8:608083. https://doi.org/10.3389/fmed.2021.608083


 Bharathi DR*
Bharathi DR*
 Chandana G.
Chandana G.

 10.5281/zenodo.11382969
10.5281/zenodo.11382969