Abstract
Anthrax is a zoonotic disease that disturbs mainly farm animals (herbivores are the natural host). Accidental human-animal transmission of disease occurs when contaminated products come into contact with the skin, respiratory system, or gastrointestinal tract. Bacillus anthracis is also utilized in biological weapons programs in many nations. About 95% of human anthrax cases are cutaneous, 5% are respiratory, and intestinal anthrax cases are extremely rare. Blood tests, skin tests, stool samples, Gram stain, and cultures of bodily fluids or lesions can all be used to make a diagnosis. When treating anthrax infections, penicillin is the recommended medication. Ciprofloxacin, doxycycline, ampicillin, and ciprofloxacin are substitutes. Additionally, a mix of the drugs was administered. It has been suggested recently that certain medicinal plants, such as neem and Tulsi, are also used as ayurvedic remedies to treat anthrax diseases. As authors, we have included every piece of information that is currently accessible on the pathophysiology, structure, epidemiology, symptoms, diagnosis, and treatment options for anthrax (Bacillus anthracis), including allopathic and—most importantly—ayurvedic remedies for the treatment and prevention of this kind of illness.
Keywords
Anthrax, Bacillus anthracis, Zoonotic disease, Ayurvedic remedies
Introduction
Anthrax is a zoonotic disease that disturbs mainly farm animals Accidental contact with infected animals or consumption of animal products can expose humans to the disease; the respiratory and gastrointestinal routes are rarely used. The gram-positive, rod-shaped bacterium Bacillus anthracis produces a toxin that causes anthrax and is mainly found in herbivorous animals. It is encased in a capsule. An industrial or agricultural exposure to diseased animals or animal products can expose humans to anthrax. Nonetheless, the illness was recognized by the ancient Egyptians and is thought to have caused two of the plagues that struck Egypt approximately 3500 years ago. It was not known which organism was the cause until Robert Koch was able to grow it in vitro in 1877.[1]Ayurveda is an ancient Indian medical system. In many parts of Asia, ayurvedic medicine is a well-organized system of traditional medical care that is used for both curative and preventive purposes. Ayurveda has a rich history; it may have started as long as 3,000 years ago in India. In many Eastern countries, particularly India, where a sizable portion of the populace either exclusively or in conjunction with modern medicine uses this system, it is still favoured as a means of healthcare today. [2]
Exploring Ayurvedic remedies for anthrax:
The purpose of exploring Ayurvedic remedies for anthrax in a review is likely to assess the traditional medicinal practices within Ayurveda and their potential efficacy in managing or treating anthrax. Anthrax is a serious infectious disease caused by Bacillus anthracis, and its treatment typically involves antibiotics such as ciprofloxacin and doxycycline. In the context of Ayurveda, an ancient system of medicine that originated in India, the focus is often on holistic approaches that consider the balance of doshas (Vata, Pitta, Kapha), lifestyle, diet, and herbal remedies. The review might aim to
- Evaluate Traditional Ayurvedic Knowledge: Assess the historical use of Ayurvedic herbs, formulations, or practices in managing infectious diseases or conditions with symptoms similar to anthrax.
- Explore Ayurvedic Remedies: Identify specific Ayurvedic herbs or formulations believed to have antimicrobial or immune-boosting properties that could potentially be relevant to anthrax treatment.
- Assess Safety and Side Effects: Examine the safety profile of Ayurvedic remedies to ensure they do not pose additional risks or side effects, especially considering the seriousness of anthrax.
- Consider Holistic Approaches: Explore holistic approaches within Ayurveda, such as lifestyle modifications, dietary recommendations, and practices that aim to restore overall balance and strengthen the body's natural defences.
- Review Scientific Evidence: If available, analyse any scientific studies or clinical trials that investigate the effectiveness of Ayurvedic remedies in managing bacterial infections or conditions similar to anthrax.
- Identify Potential Synergies: Explore if Ayurvedic remedies could be used in conjunction with conventional antibiotic treatments for anthrax to enhance overall therapeutic outcomes.
It's important to note that while traditional medicine systems like Ayurveda have a rich history and cultural significance, any exploration of alternative remedies for serious infectious diseases should be approached with caution. Conventional medical treatments, especially antibiotics, are well-established and proven effective for anthrax. Any consideration of alternative treatments should involve consultation with qualified healthcare professionals to ensure safety and efficacy.
Overview of Bacillus anthracis:
Bacteria called Bacillus anthracis cause anthrax. The spores that the bacteria produce have a long shelf life in the ground. While grazing, livestock like cattle or sheep as well as wild animals like deer may inhale or consume the dormant (inactive) spores. The anthrax bacteria enter your body through bodily fluids, multiply, and spread throughout your body. The bacteria produce a poisonous, possibly fatal reaction. Those who swallow, inhale, or come into contact with the spores on their skin go through the same procedure. [3].Spores enter the body and cause anthrax infection in humans. The spores may become activated and develop into anthrax bacteria as a result. Subsequently, the bacteria can proliferate, disperse throughout the body, generate toxins, or poisons, and result in serious disease.
Modes of transmission :
The bacterial infection of the human body occurs through the integumentary system, specifically through a cut. Commonest and least lethal form of anthrax is cutaneous anthrax. The most vulnerable people are veterinarians and those who work with animal hides, wool, or hair.
Gastrointestinal:
This kind impacts individuals who consume raw or undercooked meat from contaminated animals. The stomach, intestines, throat, and esophagus are all impacted by the bacteria. In the US, gastrointestinal anthrax is uncommon. Before killing them, American farmers vaccinate their cattle against anthrax and identify sick animals.
Inhalation:
This lethal form of anthrax can develop in people who inhale anthrax spores. It can be fatal or result in serious breathing difficulties. Wool sorter's disease is another name for inhalation anthrax, which is a condition where workers in tanneries, slaughterhouses, and wool mills may inhale spores from infected animals.
Injection:
Anthrax injection can occur in heroin users. There haven't been any reports of this type in the US; it's more prevalent in northern Europe. Anthrax injections can infect muscles or deep beneath the skin [4].
Conventional treatments and their limitations: Traditional management consists of penicillin and supportive care. However, the CDC advises broader coverage with ciprofloxacin or doxycycline due to growing concerns about the weaponization of anthrax and probable resistance to penicillin. Given that incomplete treatment can result in a mortality rate of over 50%, these recommendations cover all affected patients, regardless of age. For seven to ten days, ciprofloxacin or doxycycline can be administered as an outpatient treatment for visually normal individuals diagnosed with cutaneous anthrax. Intravenous (IV) ciprofloxacin 400 mg or doxycycline 100 mg every 12 hours, in addition to at least two additional antibiotics (such as imipenem, clindamycin, rifampin, or an aminoglycoside), should be administered to all other patients. Treatment must be administered for a minimum of sixty days, or until three doses of the anthrax vaccine are administered. It is advised to administer the vaccine on days 0 through 28. There is no evidence that any of the other interventions, such as the insertion of a chest tube or mechanical ventilation, increase survival. It is advised to take postexposure prophylaxis in situations where anthrax exposure is suspected.[6]
Ayurveda: A holistic approach:
According to Ayurveda, when any one of the three elements—air, water, or time—becomes impacted, it creates an epidemic, with animals being the first to suffer. Ayurveda holds that nonreligious actions like war are the root of the epidemic. Chemical and biological weapons are used in warfare, which contaminates the atmosphere and sparks epidemics, which in turn leads to disease. Lethal infections brought on by pathogenic microorganisms have become more commonplace worldwide and are now a major source of disease and mortality for individuals with weakened immune systems everywhere. A significant worldwide issue is the ongoing emergence of bacteria that are resistant to drugs and the infectious illnesses they can cause. One of the most vital tools in the fight against bacterial infections is the antibiotic, which also serves as the foundation for treating other microbiological infections. Antibiotics that are effective today might not be effective tomorrow due to bacterial resistance to them.[7]
Ayurvedic perspective on infectious diseases:
If we wish to use Ayurvedic medicine to treat infectious diseases, we must adhere to Acharya Charaka's Rajayaksma disease treatment protocol. It is possible to provide certain formulations, such as Sitopaladi Churna, Agastya Haritaki, Samshamani Vati, Mahasudarshana Ghanavati, etc.Preventive medicine is Ayurveda's primary treatment tenet. In order to prevent infectious diseases, there are a few major preventive measures that are outlined in Sadvritta (good regime) . Since COVID-19 is an airborne illness spread by droplet infection, the following precautions should be taken:
- It's recommended to cover your mouth when you sneeze, laugh, or yawn.
- Mucous nasal secretions should not be expelled at any other time than during a facial wash or bath
- In order to avoid breathing in stale air from other people, one should also stay far away from them.
- Every day, one should try to purify the air, apply oil to the head, ears, nose, and feet, and avoid scraping or brooming the roof.
- In order to reduce the spread of respiratory illnesses, it is recommended that people practice cough etiquette and respiratory hygiene.
- We can take a warm bath with Siddha Jala (herbal-purified water) or gargle with warm triphala or Yashtimadhu (herbs) Nasya (nasal insufflations), such as Pradhamana Nasya (nasal insufflations of powdered herbs).[8]
Concept of doshas and their role in maintaining health
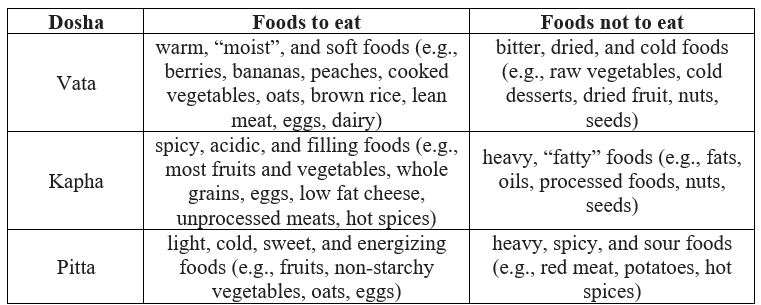
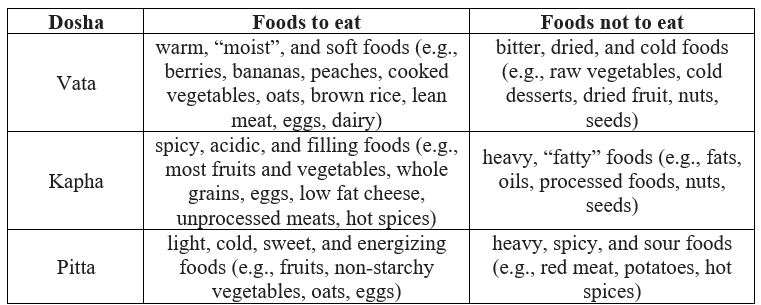
An Ayurvedic practitioner can ascertain a person's dosha based on physical, emotional, mental, and behavioral traits, drawing from centuries of Ayurvedic practice. An overview of each dosha is given here.Vata:-The elements of vata are primarily air and space, also referred to as ether. Vata is generally characterized as being dry, cold, light, rough, flowing, and spacious. Autumn's crisp, cool days are a representation of vata. Kapha:- The foundations of Kapha Kapha (pronounced "kuffa") are earth and water. It can be characterized as heavy, slow, cold, soft, steady, and stable. Since many regions of the world gradually emerge from hibernation, spring is referred to as the "kapha season. “Pitta:- Basing on fire and water, the pitta dosha is known to be linked to a tenacious personality. It is frequently characterized as hot, greasy, liquid, sharp, light, and mobile. Summertime, with its hot, sunny days, is called pitta season. [9] The above table gives brief information about foods to eat and foods to avoid when a person is suffering from Vata, Kapha, Pitta respectively. [10]
Traditional methods of diagnosing anthrax in Ayurveda :
Madhava lists the inspection of Purvarupa (prodromal symptoms), Rupa (manifested symptoms), and Samprapti (pathogenesis) as well as the performance of Upasaya (therapeutic tests) and Ashtavidha Pareeksha (physical examination) as the five primary forms of Ayurvedic diagnostic methods.The term "purvarupa" (prodromal symptoms) describes the initial warning indications of a disease that eventually precede patients' full-blown symptoms from manifesting.The difficulties and afflictions that the patient brings to the vaidyan's attention are known as rupa (manifested symptoms), and the vaidyan utilizes touch and percussion to assess the patient's condition.Samprapti, or pathogenesis, charts the patient's medical history, including personal and familial, from the moment the patient's symptoms first appear until the Nidana stage. In this case, the patient's age, general physical and mental health, and metabolism all play a significant part in the diagnosis.Herbal treatments and lifestyle advice known as upasaya (therapeutic testing) are effective in halting the disease's progression.The unique stage where a comprehensive examination is conducted is called Ashtavidha Pareeksha (physical examination). The patient's Nadi (pulse), Jihva (tongue), Sabda (voice), Sparsa (touch), Drik (eyes), Akruti (appearance), Mutra (urine), and Mala (feces) are all examined by the doctor.
Pulse diagnosis (Nadi Pariksha) and other diagnostic techniques:
Here are eight common ways of diagnosis in AyurvedaOne of the most significant diagnostic techniques in Ayurveda is pulse diagnosis, or nadi pariksha. When feeling the pulse at the wrist, Ayurvedic practitioners use three fingers to evaluate the pulse's strength, rhythm, and quality. Every pulse has a distinct dosha (Pitta, Kapha, and Vata) and might indicate bodily imbalances.
- Tongue Exam (Jihva Pariksha): The color, coating, shape, and texture of the tongue are examined to assess dosha imbalances and general health.
- Iris Diagnosis (Iridology): Ayurvedic practitioners use the patterns and colors of the iris to determine imbalances in the body's organs and systems, much like iridology is used in Western alternative medicine.
- Face Reading (Mukha Pariksha): To determine dosha imbalances and general health, the face's features—such as the eyes, nose, lips, and skin—are analyzed.
- Observation of Body Constitutions (Prakriti Analysis): In order to ascertain a person's primary dosha constitution (Vata, Pitta, or Kapha), practitioners evaluate a person's bodily composition, body shape, and traits.
- Diet and Lifestyle Assessment (Ahar-Vihar Pariksha): To determine the causes of dosha imbalances, Ayurvedic practitioners assess a patient's food habits, daily schedule, and lifestyle decisions.
- Questioning (Prashna): Through questioning, a thorough medical history, including symptoms, past medical conditions, and family history, is gathered for the patient. This aids in comprehending the imbalances and particular constitution.
- Palpation and Physical Examination: A hands-on examination of the body can provide more diagnostic details. This includes feeling for tender spots, evaluating the texture and temperature of the skin, and looking for any physical anomalies.
Integrating modern diagnostic tools with Ayurvedic principles:
The diagnostic instruments for the ailments listed in the Ayurvedic classics aid in standardizing the clinical procedure to reach a particular diagnosis.It takes an hour to use the many contemporary instruments that aid in early diagnosis and illness state since changes in Dosha and Dushya are subtle and reaching a likely diagnosis is challenging. Acharya Susruta described the Naadi Yantra and Shalaka Yantra in Ayurveda in order to eliminate Shalya or any foreign particles from the body and to determine the direction, size, and shape of Shalya. Electroencephalography (EEG), one of several contemporary imaging techniques, is capable of identifying anomalies in your brain waves. magnetic resonance imaging (MRI), which generates intricate, three-dimensional pictures of the anatomy. Computed tomography (CT) scan: a collection of X-ray pictures of your body collected from various perspectives. Ultrasonography (USG), which scans the body's internal organs using high-frequency sound waves. The electrical voltage pattern produced by the heart is recorded via electrocardiography (ECG).It is noteworthy that the description of diagnostic tools and methods found in ancient Ayurvedic literature is relevant. More advanced diagnostic and imaging techniques are also required in an hour to improve understanding of diseases and diagnose them. [11]
Ayurvedic remedies for anthrax: Herbs with antimicrobial properties in Ayurveda
Neem (Azadirachta indica) :
Azadirachta indica A. Juss and Melia azadirachta are the two closely related species of neem; the former is commonly referred to as the Indian neem, or margosa tree, and the latter as the Persian lilac. Neem has drawn attention for its capacity to act as an inexpensive natural pesticide in addition to its insect-repelling, anti-feedant, and growth-disturbing properties. The most widely used neem product is neem oil, which is made from the fruit's seed kernels. In terms of pesticide production, it is widely considered to have the highest concentration of active ingredients. It is also used to treat a variety of skin conditions and to make soap.Recent research has also shown that the plant is active against illnesses caused by fungi, viruses, and bacteria. Neem originated in India and is now widely used in tropical, subtropical, and dry regions of the world. It grows predominantly in the southern Terai region of Nepal. [12]
Turmeric (Curcuma longa) :
A member of the Zingiberaceae (ginger) family, turmeric is a herbaceous evergreen plant. In India, China, and South East Asia, turmeric (Curcuma longa) is widely used as a spice, food preservative, and coloring agent. Primarily used as an ingredient in curry powder, turmeric powder also contributes to the vibrant yellow color of ballpark mustard. Turmeric has been utilized extensively in traditional medicine across the globe, in addition to its culinary use. It has been demonstrated that the primary yellow bioactive ingredient in turmeric, curcumin (diferuloylmethane), has a broad range of biological effects. The anti-inflammatory, antioxidant, anti-carcinogenic, anti-mutagenic, anticoagulant, antifertility, antidiabetic, antibacterial, antifungal, antiprotozoal, antiviral, antifibrotic, antivenom, antiulcer, hypotensive, and hypocholesteremic properties of this substance are examples of these.The turmeric plant was a great natural antibacterial, disinfectant, anti-inflammatory, and painkiller for old Ayurvedic medicine. It was also frequently used to heal skin irritations, promote gut flora, and help with digestion.[13]
Triphala formulation :
One well-known Ayurvedic polyherbal compound is called "Triphala." It is made up of equal amounts of dried fruits from Terminalia belerica, Terminalia chebula, and Emblica officinalis (1:1:1). This combination has been used traditionally to treat a variety of illnesses, including laxative, colon cleansing, digestive, and rejuvenator [14].
Detoxification therapies in Ayurveda:
Panchakarma therapies:
The term panchakarma refers to the five primary Ayurvedic detoxification methods, which are: raktamokshana (bloodletting), vamana (emesis), virechana (purgation), nasya (nasal instillation of herbal oils/powders), and basti or vasti (herbal enema). These operations are frequently combined with complementary therapies to clear the channels, get rid of toxins from the body, and bring the body back into equilibrium. One of the most significant Ayurvedic therapy techniques is panchakarma. When carried out properly, it improves the efficacy and responsiveness of later therapy.Every procedure is carried out in three stages: the primary procedure, the cleaning phase, and the post-cleansing phase, which includes changing one's diet and lifestyle. Adjuvant allied therapies include, but are not limited to, ayurvedic oil dripping treatment (shirodhara), warm herbal oil retention on the scalp (shirobasti), warm herbal oil retention on the back (katibasti), and warm herbal oil retention on the knee (janubasti). Each patient's unique needs are taken into account when designing treatment programs. Panchakarma can also be employed as a rejuvenating and preventative measure. This means that everyone—even those in good health—can use it.[15]
Herbal detoxification methods :
Drugs derived from plants, animals, and minerals are used in Ayurveda. Each of the three drug sources falls into one of two categories: poisonous or nonpoisonous. Numerous crude drugs exist, most of which contain hazardous ingredients and undesired impurities that can cause serious health issues. Numerous writers have noted that because many medicinal plants contain toxic and dangerous phytoconstituents, not all of them are safe to use. The process of ?odhana, which means detoxification or purification, entails turning any toxic substance into a useful, nontoxic one. Among the intriguing instances of poisonous plants still utilized in Indian medicine are Vatsan?bha (Aconitum species), Semecarpus anacardium, Strychnos nux-vomica, Acorus calamus, Abrus precatorius, etc. Some of the relatively toxic components found in these plants include abrin, strychnine, ?-asarone, bhilawanols, and aconite. The ?odhana process purifies while lowering the concentrations of harmful elements, which can occasionally lead to increased therapeutic efficacy. [16]Chemical chelators are the most widely used technique for eliminating heavy metals from the body. Because they have fewer negative effects, medicinal plants have recently caught the interest of researchers as possible remedies for heavy metal intoxication. In the current study, we examine the potential of herbal remedies for treating heavy metal poisoning, including triphala, phytochelatins, Chlorophyta (green algae), Ginkgo biloba (gingko), Silybum marianum (milk thistle), Coriandrum sativum (cilantro), and Allium sativum (garlic).
Strengthening the immune system through Ayurveda :
- Rasayana therapies:
Ayurvedic medicine has been practiced for ages through its eight specialized branches:
- Internal Medicine (Kayakitsa)
- Surgery (Salya)
- Ophthalmology and ENT (Salakya)
- Paediatrics (Kummarbhritya)
- Toxicology (Aagada tantra)
- Psychiatry (Bhuta Vidya)
- Rejuvenation (Rashayana)
- Sexology (Bajikarana)
Rasayana Tantra is one of these disciplines that addresses immuno-enhancement, therapeutic diet, and longevity. The three main mechanisms by which the Ayurvedic Rasayana remedies work are:
- A Direct Nutrient Effect Or Rasa Enhancing Agent
- Agni Enhanc- Ers Or Promoters Of Digestion And Metabolism
- Srotas Purifying Agents Or Promoters Of Microcirculation And Tissue Perfusion.
When these three things happen separately or in combination, the body's nutritional state is enhanced, which promotes the development of the best types of cells and tissues that support aging and stress—‘Labhopayo hi shastanam rasadinam Rasayanam’ (Charaka Chikitsa—1). In general, all rasayanas promote nourishment; however, some are unique to particular organs or tissues, such as the brain-specific Medhya rasayana, the heart-specific Hridya rasayana, the skin-specific Twacha rasayana, the eye-specific Caksusya rasayana, and so forth. Likewise, Rasayanas may also be age-specific because, as Table 1 illustrates, they support nutrition in line with the normal bio-losses that happen at various stages of life. The following list of Rasayana therapies can be utilized to offset bio-losses associated with aging.In general, all rasayanas promote nourishment; however, some are unique to particular organs or tissues, such as the brain-specific Medhya rasayana, the heart-specific Hridya rasayana, the skin-specific Twacha rasayana, the eye-specific Caksusya rasayana, and so forth. Likewise, Rasayanas may also be age-specific because, as Table 1 illustrates, they support nutrition in line with the normal bio-losses that happen at various stages of life. The following list of Rasayana therapies can be utilized to offset bio-losses associated with aging.[17]
- Dietary recommendations:
Ayurveda defines svasthya as "to be established in one's self or own natural state," or optimal health. This requires achieving a level of self awareness and contentment, as well as balancing structural and physiological elements, metabolic and excretory processes, body tissues, senses, and the mind [18]. Ayurvedic medicine uses ten factors (dasa vidha pariksa) to assess an individual's health: body tissues (dusya), place of residence (desa), physical strength (bala), seasons and time (kala), digestive and metabolic processes (agni or anala), genetic and phenetic constitution (prakriti), age (vaya), mental strength or temperament (sattva), habituation (satmya), and food (ahara) [19]. It's noteworthy to note that sattva is thought to have an impact on wellbeing. Although their primary application is in diagnosis, these can also be used to gauge an individual's level of wellbeing.The distinctive Ayurvedic ideas in nutrition, such as pathya, viruddha ahara, kala and desa vicara, agni, ama, etc., still require a great deal of study [18, 10].
Ayurvedic case studies
Modern science discovers, creates, describes, explains, and introduces a great deal of new diseases. Researchers may now investigate the genesis and development of illnesses right down to the DNA level. However, when it comes to Ayurveda, we must take into account the basic ideas in order to create the Samprapti (pathophysiology) and subsequently create the treatment plan, which may include Shamana (medical management) or Shodhana (purification techniques). In that scenario, administering a herbal medication alone—which is justified by current research—would not be adequate. First, it is necessary to formulate the etiology from an Ayurvedic perspective by amplifying the core concepts of Ayurveda through the integration of contemporary investigative instruments. For instance, nerve conduction tests and electromyelography can be helpful in diagnosing of a disease that is related to Mamsa Dhatu (muscular tissue), which may be Mamsagata Vata, Mamsavritta Vata, etc., in Ayurveda and muscular dystrophy in modern medicine. Analogously, these examinations can also be helpful in determining the effectiveness of Ayurvedic practices like Pinda Sweda and Shashtika Shali Sweda, which include fermenting red rice cooked in milk. This will supply the factual information. However, it would only be somewhat beneficial to provide certain medications based on contemporary research without also identifying the Awastha (state) of Dosha, level of Dhatu, and Aama status according to Ayurveda. As a result, standardizing the basic diagnostic concepts is crucial, as is incorporating them with contemporary research instruments and applying them to the acquisition of a diagnostic and therapeutic viewpoint. This could aid the younger, more intelligent and quick-witted generation in overcoming the difficulties in applying Ayurveda to comprehend more recent problems.[21]
Integrative approaches
Combining Ayurvedic and modern medicine for anthrax treatment In contemporary medicine, antibiotics such as ciprofloxacin, tetracycline, and penicillin are used to treat anthrax patients. Sanjeevani Vati, Mahamrutyunjaya Rasa, Arogyawardhini, and Amritarishta, according to Ayurveda, can be administered as natural antibacterial medications to complement contemporary medication therapy. These Ayurvedic medications strengthen the immune system, help it function better, and can be used as preventative medicine. Collaborative research and clinical trials :PA is the main immunogen of the two currently approved vaccines, AVA and AVP. AVA also has traces of LF but almost no EF, whilst AVP has some LF and EF traces. Non-clinical results from the experimental use of both vaccines would imply that AVA and AVP, when administered prior to and within a specified period of time after exposure, are both effective in protecting animals. Serological correlates of protection that predict vaccine efficacy in humans have been found in recent findings from extensive and comprehensive research in non-human primates [23; 31; 24, 28].While increasing immunogenicity by adding CpG, for example to the AVA formulation as NuThrax [30; 29,25], the AVA and AVP formulations in clinical use can be reactogenic. As a result, current efforts are focused on rationalizing the clinical dosing regimen to reduce dosing frequency [26,27]
CONCLUSION
Key findings on Ayurvedic treatment for anthrax highlight the potential benefits of herbal formulations, immune system support, and holistic approaches. Further research is essential to validate these findings and establish evidence-based guidelines for integrating Ayurveda into anthrax management.Ayurveda's holistic approach and natural remedies may offer complementary support in managing anthrax, focusing on immune system enhancement and overall well-being. However, it's crucial to consult with modern medical professionals for evidence-based treatments.It is appropriate that the extensive pharmacopeia and fundamentals of this antiquated field can now be investigated using systems biology's cutting-edge technology to identify novel immunological, molecular, and cellular components of health and illness. This method may uncover emergent mechanisms that were previously unrecognized and provide insight into the workings of Ayurvedic beliefs and treatments. Additionally, it can reveal common physiological mechanisms that underpin the onset of several illnesses, including cancer, diabetes, musculoskeletal disorders, mental health issues, and cardiovascular disease.This work can help create new biomarkers for health and disease as well as paradigm-shifting whole person health research methodologies. [32,33]
REFERENCE
- Friedlander AM. 2000. Anthrax: clinical features, pathogenesis, and potential biological warfare threat. Curr Clin Topics Infect Dis, 20: 335-349
- Britannica, The Editors of Encyclopaedia. "Ayurveda". Encyclopedia Britannica, 27 Feb. 2024, https://www.britannica.com/science/Ayurveda. Accessed 30 March 2024.
- National Organization for Rare Disorders. Anthrax (https://rarediseases.org/rare-diseases/anthrax/). Last updated: 7/22/2015. Accessed 6/17/2023.
- Brachman P., and Friedlander AM. 1999. Anthrax. In: Plotkin SA., Orenstein WA. (eds) Vaccines (3rd ed.). WB Saunders Co., Philadelphia. pp. 629- 637
- Brachman P., and Friedlander AM. 1999. Anthrax. In: Plotkin SA., Orenstein WA. (eds) Vaccines (3rd ed.). WB Saunders Co., Philadelphia. pp. 629- 637
- McComb RC, Martchenko M. Neutralizing antibody and functional mapping of Bacillus anthracis protective antigen-The first step toward a rationally designed anthrax vaccine. Vaccine. 2016 Jan 2;34(1):13-9. doi: 10.1016/j.vaccine.2015.11.025. Epub 2015 Nov 21. PMID: 26611201.
- Rakholiya K, Kaneria M, Chanda S. Inhibition of microbial pathogens using fruit and vegetable peel extracts. International journal of food sciences and nutrition. 2014 Sep 1;65(6):733-9.
- Priyanka Shelotkar, & Swapnil Borage. (2020). Concept of infectious diseases in Ayurveda. International Journal of Research in Pharmaceutical Sciences, 11(3), 4756–4759.
- Shepard CW, Soriano-Gabarro M, Zell ER, Hayslett J, Lukacs S, Goldstein S, Factor S, Jones J, Ridzon R, Williams I, Rosenstein N; CDC Adverse Events Working Group. Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence. Emerg Infect Dis. 2002 Oct;8(10):1124-32. doi: 10.3201/eid0810.020349. PMID: 12396927; PMCID: PMC2730317.
- Jeitler M, Wottke T, Schumann D, Puerto Valencia LM, Michalsen A, Steckhan N, Mittwede M, Stapelfeldt E, Koppold-Liebscher D, Cramer H, Wischnewsky M, Murthy V and Kessler CS (2021) Ayurvedic vs. Conventional Nutritional Therapy Including Low-FODMAP Diet for Patients With Irritable Bowel Syndrome—A Randomized Controlled Trial. Front. Med. 8:622029. doi: 10.3389/fmed.2021.622029
- Banso, A., & Adeymo, S. (2003). Phytochemical screening and antimicrobial assessment of Abutilon mauritianum, Bacopa monnifera and Datura stramonium. Biokemistri, 18, 39e44.
- Mandal S, Mandal MD. Antibacterial Potential of Neem Tree (Azadirachta indica A. Juss) Seeds. InNuts and seeds in health and disease prevention 2011 Jan 1 (pp. 803-811). Academic Press.
- ????. Kapoor LD: Handbook of Ayurvedic Medicinal Plants. ??????. 2002 Feb 20;77(1):60-.
- Patel H, Patel F, Jani V, Jha N, Ansari A, Paliwal B, Rathod B, Patel D, Patel P, Kothari V. Anti-pathogenic potential of a classical ayurvedic Triphala formulation. F1000Res. 2019 Jul 18;8:1126. doi: 10.12688/f1000research.19787.2. PMID: 33093941; PMCID: PMC7549186.
- Sharma H, Chandola HM, Singh G, Basisht G. Utilization of Ayurveda in health care: an approach for prevention, health promotion, and treatment of disease. Part 1--Ayurveda, the science of life. J Altern Complement Med. 2007 Nov;13(9):1011-9. doi: 10.1089/acm.2007.7017-A. PMID: 18047449.
- Maurya SK, Seth A, Laloo D, Singh NK, Gautam DN, Singh AK. ?odhana: An Ayurvedic process for detoxification and modification of therapeutic activities of poisonous medicinal plants. Anc Sci Life. 2015 Apr-Jun;34(4):188-97. doi: 10.4103/0257-7941.160862. PMID: 26283803; PMCID: PMC4535066.
- Singh RH, Narsimhamurthy K, Singh G. Neuronutrient impact of Ayurvedic Rasayana therapy in brain aging. Biogerontology. 2008 Dec;9:369-74.
- Verotta L, Macchi MP, Venkatasubramanian P, editors. Connecting Indian wisdom and western science: Plant usage for nutrition and health. CRC Press; 2015 Apr 24.
- Raj GA, Ikbal NM, Kumar DS. A????gah?daya: A Scientific Synopsis of the Classic Ayurveda Text. CRC Press; 2023 May 5.
- Payyappallimana U. Health and well-being in Indian local health traditions. InAn integrated view of health and well-being: Bridging Indian and western knowledge 2013 May 19 (pp. 99-112). Dordrecht: Springer Netherlands.
- Chandola HM. New challenges for Ayurveda: How it will stand? Ayu. 2012 Apr;33(2):165-6. doi: 10.4103/0974-8520.105231. PMID: 23559783; PMCID: PMC3611633.
- NIMISHA K, Dr.K AMBIKA, Dr. SUNIL JOHN THYKATTIL, & Dr. PRAVITH N K. (2023). Multiple myeloma - Modern and Ayurvedic perspective- a critical review. Kerala Journal of Ayurveda, 2(2). https://doi.org/10.55718/kja.155
- Fay MP, Follmann DA, Lynn F, Schiffer JM, Stark GV, Kohberger R, Quinn CP, Nuzum EO. Anthrax vaccine-induced antibodies provide cross-species prediction of survival to aerosol challenge. Sci Transl Med. 2012 Sep 12;4(151):151ra126. doi: 10.1126/scitranslmed.3004073. PMID: 22972844; PMCID: PMC3668972.
- [Schiffer JM, Chen L, Dalton S, Niemuth NA, Sabourin CL, Quinn CP. Bridging non-human primate correlates of protection to reassess the Anthrax Vaccine Adsorbed booster schedule in humans. Vaccine. 2015 Jul 17;33(31):3709-16. doi: 10.1016/j.vaccine.2015.05.091. Epub 2015 Jun 10. PMID: 26072016; PMCID: PMC6360524.
- Shepard CW, Soriano-Gabarro M, Zell ER, Hayslett J, Lukacs S, Goldstein S, Factor S, Jones J, Ridzon R, Williams I, Rosenstein N; CDC Adverse Events Working Group. Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence. Emerg Infect Dis. 2002 Oct;8(10):1124-32. doi: 10.3201/eid0810.020349. PMID: 12396927; PMCID: PMC2730317.
- Wright JG, Plikaytis BD, Rose CE, Parker SD, Babcock J, Keitel W, El Sahly H, Poland GA, Jacobson RM, Keyserling HL, Semenova VA, Li H, Schiffer J, Dababneh H, Martin SK, Martin SW, Marano N, Messonnier NE, Quinn CP. Effect of reduced dose schedules and intramuscular injection of anthrax vaccine adsorbed on immunological response and safety profile: a randomized trial. Vaccine. 2014 Feb 12;32(8):1019-28. doi: 10.1016/j.vaccine.2013.10.039. Epub 2013 Dec 25. PMID: 24373307; PMCID: PMC9067390.
- Anthrax Vaccine Adsorbed. (1965). United States Patent US 3208909. Washington, DC: US Patent and Trademark Office Anthrax ACIP Vaccine Recommendations. (2001). Available online at: http://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/anthrax.html
- Georgopoulos AP, James LM. Anthrax Vaccines in the 21st Century. Vaccines (Basel). 2024 Feb 3;12(2):159. doi: 10.3390/vaccines12020159. PMID: 38400142; PMCID: PMC10892718.
- Minang JT, Inglefield JR, Harris AM, Lathey JL, Alleva DG, Sweeney DL, Hopkins RJ, Lacy MJ, Bernton EW. Enhanced early innate and T cell-mediated responses in subjects immunized with Anthrax Vaccine Adsorbed Plus CPG 7909 (AV7909). Vaccine. 2014 Nov 28;32(50):6847-54. doi: 10.1016/j.vaccine.2014.01.096. Epub 2014 Feb 13. PMID: 24530403; PMCID: PMC4133324.
- Ionin B, Hopkins RJ, Pleune B, Sivko GS, Reid FM, Clement KH, Rudge TL Jr, Stark GV, Innes A, Sari S, Guina T, Howard C, Smith J, Swoboda ML, Vert-Wong E, Johnson V, Nabors GS, Skiadopoulos MH. Evaluation of immunogenicity and efficacy of anthrax vaccine adsorbed for postexposure prophylaxis. Clin Vaccine Immunol. 2013 Jul;20(7):1016-26. doi: 10.1128/CVI.00099-13. Epub 2013 May 8. PMID: 23658392; PMCID: PMC3697458.
- Ding G, Chen X, Zhu J, Duesbery NS, Cheng X, Cao B. A human/murine chimeric fab antibody neutralizes anthrax lethal toxin in vitro. Clin Dev Immunol. 2013;2013:475809. doi: 10.1155/2013/475809. Epub 2013 Jun 5. PMID: 23861692; PMCID: PMC3687597.
- White JD, O'Keefe BR, Sharma J, Javed G, Nukala V, Ganguly A, Khan IA, Kumar NB, Mukhtar H, Pauli GF, Walker L, Sivaram S, Rajaraman P, Trimble EL. India-United States Dialogue on Traditional Medicine: Toward Collaborative Research and Generation of an Evidence Base. J Glob Oncol. 2018 Sep;4:1-10. doi: 10.1200/JGO.17.00099. Epub 2017 Nov 16. PMID: 30241135; PMCID: PMC6180779.
- Acharya R. Annexe of Ayurveda in G-20 countries: A brief insight. Journal of Drug Research in Ayurvedic Sciences. 2023 Oct 1;8(4):309-13.


 Tisha Thakkar* 1
Tisha Thakkar* 1
 Dhruvi Patel 1
Dhruvi Patel 1
 Taufik Mulla 2
Taufik Mulla 2
 10.5281/zenodo.10974728
10.5281/zenodo.10974728