Abstract
Soft tissue damage results in severe, extremely expensive therapeutic therapy. Microvascular consequences of diabetes mellitus resulting from neuropathy damage deformities include diabetic foot ulcers (DFU). peripheral artery disease and elevated plantar pressure that result in lower limb amputations Due to the aging of the population, extended hospitalization has increased patient morbidity from diabetes mellitus during the past few decades. Complications are not influenced by time, but rather by the level of chronic glycemia. Measurement of glycosylated hemoglobin (HbA/c level).
Keywords
Diabetes mellitus, Diabetic foot ulcers, deep learning, infections.
Introduction
Any foot infection in a diabetic patient that results from an acute or chronic damage to the foot's soft tissues and shows signs of neuropathy or ischemia Accurate diagnosis of 70% of lower limb amputations thorough examination that combines microbiological investigations, clinical evaluation, and imaging studies A diversified approach is required for management. Both antimicrobial treatment and surgery Motor impairment and sensory loss are hallmarks of peripheral neuropathy, which makes people more susceptible to altered foot abnormalities. Extremely high incidence of foot ulcers in diabetes. Myelopathy is a serious issue. If 71 out of 41 people have ulcers on the soles of their feet as a result of "unrecognized trauma," it is silent and doesn't pain, even in cases of gangrene. More over half of ulcers in diabetes individuals develop a clinical infection, and 15–25% of diabetic persons may develop DFU at some point in their lives. In order to decrease amputations and enhance quality of life, a multidisciplinary approach is crucial while treating DF ulcers. The use of antibiotics according to the severity of infections was also covered by antibiotic therapy recommendations.
Causes: Diabetic foot ulcers can be caused by a variety of factors, including poor blood flow, nerve damage, foot deformities, and repetitive trauma to the feet.
Consequences: If left untreated, diabetic foot ulcers can lead to serious complications, such as infection, gangrene, and even amputation, which can significantly impact a person's quality of life and overall health.
Prevalence and Incidence of Diabetic Foot Ulcers:
|
Global Prevalence
|
6-8% of people with diabetes
|
|
Annual Incidence
|
2-6% of people with diabetes
|
|
Recurrence Rate
|
40-70% within 1 year
|
|
Increased Risk with Age
|
Higher rates in older adults
|
Staging and classification:
1.Wagners
2.University of Texas
The most commonly used classification for diabetic ulcers is the Wagner classification
|
Grade
|
Clinical Finding
|
|
0
|
intact skin (impending ulcer)
|
|
1
|
superficial
|
|
2
|
Deep to tendon bone or ligaments
|
|
3
|
Osteomyelitis
|
|
4
|
Gangrene of toes or forefoot
|
|
5
|
Gangrene of entire foot
|
Stages of diabetic foot ulcers:
1 A superficial callus may grow as a result of aberrant pressure on the foot that is not felt when bearing weight because of a lack of sensation. The first indication of a diabetic foot ulcer is an initial skin break. For the wound to heal, it is essential to thoroughly evaluate and prepare it.
2 Inflammation and small impact trauma can cause bleeding beneath the callus. At this point, necrosis or tissue death develops in the wound, making it uncomfortable to touch and possibly smelling and discolored.
3. granulations start to show up, which makes the wound more uncomfortable and bigger.
4. This stage is the worst since there is more tissue damage and a higher.

Fig.1
A) Pathogenesis:
- Multi- factorial and complex:
- Neuropathy
- Vasculopathy
- Immune dysfunction
- Prolonged Hyperglycemia contributes to all the above factors through different mechanisms
Despite the long-established link between somatic and autonomic neuropathy and foot ulcers, the risk of developing the first foot ulcer is seven times higher in people with neuropathic diabetes in terms of sensory loss. Reduced sweating and dry skin that is more likely to crack and fissure due to increased blood flow arteriovenous shunting and the warm foot are symptoms of sympathetic autonomic neuropathy in the lower extremities. Good clinical observation and comprehensive foot examination, including taking off shoes and socks, are indicators of neuropathic
Risk Factors and Causes:
- Neuropathy
- Nerve damage that leads to loss of sensation and decreased ability to feel pain or discomfort in the feet.
- Peripheral Arterial Disease
- Reduced blood flow to the extremities, which can impair wound healing and increase the risk of infection.
- Foot Deformities
- Structural changes in the feet, such as bunions, hammertoes, or Charcot foot, that can increase pressure and lead to ulcer formation.
- Poor Foot Care
- Neglecting basic foot hygiene, failing to properly trim nails, and not wearing appropriate footwear can contribute to ulcer development.
Principles of Wound Care:
Debridement: Removing dead or devitalized tissue to promote wound healing and prevent infection.
Moisture Balance: Maintaining an optimal moisture level in the wound to support the healing process.
Infection Control: Implementing appropriate antimicrobial measures to prevent and manage wound infections.
Infection Signs:
Redness: Inflammation and increased blood flow to the affected area.
Swelling: Accumulation of fluid due to the body's immune response.
Pus: Buildup of white blood cells, dead tissue, and bacteria, indicating a serious infection.
•For patients with diabetic foot ulcers, the following protocol was created:
- establishing effective communication between the patient, the wound healing team, and the primary care physician; (2) providing comprehensive, protocol-driven care for the entire patient, including hemoglobin A1c, microalbuminuria, and cholesterol as well as early treatment of retinopathy, nephropathy, and cardiac disease; (3) objectively measuring the wound every week using digital photography and planimetry, and the Wound Electronic Medical Record, if available, to document the wound-healing process; (4) noninvasive flow measurements or other objective assessment of blood flow in the lower extremities; (5) debridement of nonviable, infected, and hyperkeratotic tissue; (6) the use of systemic antibiotics for cellulitis, drainage, and deep infection; (7) offloading; (8) keeping the wound bed moist; (9) As part of the protocol, all patients should be checked for callus formation and have all calluses removed. Patients with diabetic foot ulcers must also be examined for thickened fungal toenails (onychomycosis), a fungal infection of the nails that affects one-third of patients with diabetes. Callus formation with hemorrhage is a sign of impending skin breakdown and ulceration, and removal of the callus lowers plantar pressure.
Fungal toenails: The quality of life of patients is impacted by morbidity. 78–80 It's crucial to note that untreated toenails have a reduced capacity to prevent infection. These toenails, which we frequently culture, frequently contain bacteria. For instance, the sharp and brittle nails that are a symptom of onychomycosis can cause bacterial infections following skin damage. Fungal toes can be treated with oral antifungal medications (such as griseofulvin, itraconazole, ketoconazole, and terbinafine) and topical fluconazole therapy (such as ciclopirox nail lacquer, 8%), which is preferable over systemic treatment. Procedures involving mechanical intervention range from routine nail care to complete surgical nail avulsion. As part of treatment, debridement of diseased nails is beneficial.Because it enables the elimination of refractory dystrophic columns and the decrease of thick, sharp nails.
Growth Factors: It is possible to create individual synthetic growth factors using recombinant DNA technology. Growth factors may act on adjacent cells in paracrine function or on cells that make growth factors in autocrine function. They may promote cellular proliferation, chemotaxis, angiogenesis, protein expression, and enzyme synthesis.Growth factors cause the wound's cells to become active, sending messages to the target cells that start the healing process.By promoting the production of granulation tissue and improving epithelization, growth factors applied topically to wounds might hasten healing.Recombinant human PDGF-BB, or becaplermin, is a homodimer made using recombinant DNA technology. The B chain of human PDGF, or PDGF-BB, is found in becaplermin. This naturally occurring PDGF promotes the chemotactic recruitment and proliferation of cells involved in the wound repair process.Becaplermin is a gel made of sodium carboxymethylcellulose that is used topically. Applying a tiny layer to the wound (with a tongue depressor) and then covering it with a gauze dressing soaked with saline is the strategy for administering becaplermin.Twelve hours later, the becaplermin is gently washed off and replaced with gauze saturated with saline (without reapplying the gel) or the gel is administered again.The cycle is repeated every 12 hours after the dressing is changed and the gel is reapplied.
B) Neuropathy:

Fig. 2
•Sensory Neuropathy: The general word "neuropathy" refers to a lack of movement, sensorium, autonomic function, and feedback in a specific location. It might be either a peripheralized neuropathy or a centralized neuropathy caused by the dispersion of neurotomes paralyzing the extremities. In the extremities, peripheral neuropathy in various degrees is most frequently observed. The most common cause of peripheral neuropathy, which often primarily affects the limbs, is diabetic peripheral neuropathy. alcoholism, B12 deficiency, poisons (including chemotherapy), amyloid, hypothyroidism, autoimmune diseases, Lyme disease, syphilis, HIV, and genetic illnesses such demyelinating polyneuropathy and Charcot-Marie-Tooth.Significant pedal surfaces like the heel are affected by the majority of neuropathic ulcerations, which develop in the lower extremities.

•Motor Neuropathy: Diabetes can lead to motor neuropathy, affecting the nerves that control foot muscles. This can cause muscle weakness, foot deformities, and increased risk of foot ulcers, a serious complication requiring prompt treatment and interdisciplinary care. qPathology of Motor Neuropathy : Nerve damage Prolonged high blood sugar levels harm motor nerves, reducing their ability to signal foot muscles. Muscle Atrophy Without nerve signals, the foot muscles waste away, resulting in deformities and instability. Changed Foot BiomechanicsWeakened muscles and anatomical alterations affect how the foot operates resulting in increased the pressure.

•Autonomic Neuropathy: Damage to the nerves governing involuntary bodily activities is known as autonomic neuropathy. It has an impact on digestion, blood pressure, and heart rate.It affects 20–40% of people with diabetes and is common in diabetic patients. The longer the disease lasts, the higher the incidence. Effects has a major impact on life quality and raises the probability of death. Early symptoms are often modest, leading to underdiagnosis.

|
Symptoms
|
Diagnostic Tests
|
|
Dry, cracked skin
|
Quantitative sudomotor axon reflex test (QSART)
|
|
Decreased sweating
|
Heart rate variability testing
|
|
Slow-healing wounds
|
Thermoregulatory sweat test
|
|
Orthostatic hypotension
|
Skin biopsy for small fiber neuropathy
|
•Peripheral neuropathy: is the most common in the diabetic population. It is thought to be caused by cell death due to inflammation and oxidative stress on the tissues, which leads to nerve dysfunction.This is exacerbated by hyperglycemia and insulin resistance, which result in the inability to control various metabolic pathways inside the body and increase reactive oxygen species (ROS) within the tissues. ROS causes direct nerve damage and, ultimately, peripheral polyneuropathy.This neuropathy evolves from unmyelinated fibers to demyelination of myelinated nerve fibers, which accounts for sensory, autonomic, and motor neuropathies. There are several recognized causes of peripheral neuropathy, which can be divided into four groups: toxic, metabolic, systemic, and anatomical. Nerve dissection following surgery or unintentional injury, sciatic nerve compression, and fibular nerve compression or entrapment are the anatomic causes of neuropathy. Tick bites, amyloidosis, sarcoidosis.
•Multidisciplinary Approach and Case Studies
|
multidisciplinary team
|
Coordinated care involving various healthcare providers, such as podiatrists, wound care nurses, vascular surgeons, and primary care physicians, is essential for optimizing diabetic foot ulcer management.
|
|
Case Studies
|
Reviewing real-world examples of successful diabetic foot ulcer treatment strategies can provide valuable insights and guidance for healthcare professionals
|
*Nerve examination:
1.Monofilament test. You will close your eyes as your provider sweeps a soft strand of nylon (monofilament) across your foot and toes. You'll notice when the thread touches your foot.
2.Tuning fork and vibration perception threshold (VPT) testing : Your provider will place a tuning fork or other vibrating device on various sections of your foot and toes to determine whether or not you can feel the vibrations.
3.Pin-prick test : Your provider will gently press a small pin against your big toe to see whether you can feel anything. The pin will not penetrate your skin.
4.Ankle reflexes : Your provider will tap a unique, compact hammer on your Achilles tendon, the strong band of tissue connecting your calf muscle to to your heel bone. If your nerves are functioning normally, your foot will jerk slightly on its own.
•Skin examination: Examine the skin on your feet for dryness, cracking, calluses, blisters, ulcers, and any other damage or odd regions. Check your toenails for cracks and fungal infections.Check the temperature of your feet to determine if they are same.
•musculoskeletal (muscle and bone) examination : Your provider will check for concerns like bent or overlapped toesBunions Charcot Foot is characterized by a rocker shape on the bottom of the foot.
•vascular (blood vessel) examination: To assess blood flow to your feet, a doctor may Feel the pulses in your ankle and foot.Compare the blood pressures in your ankles and arms. If your ankle's blood pressure is lower than your arm's, your foot may have less blood flow. This is referred to as an ankle-brachial index test.If you exhibit signs and symptoms of a blood flow problem, your doctor may advice this test.
C) Vasculopathy:
Diabetic Vasculopathy is an encompassing term used to describe vascular complications associated with systemic hyperglycemia and hypertension seen in diabetes. The hallmarks of diabetic vasculopathy include injury to large vessels such as the aorta and coronary vessels as well as more peripheral injuries such as retinopathy and nephropathy
In diabetes there is macro and microangiopathy
1. Macroangiopathy: Atherosclerosis of large arteries
2. Microangiopathy: Increased thickness of basement membrane and endothelial proliferation capillary damaged.

Fig no.6
• Immune dysfunction : Impaired defense against infection
1. Polymorphonuclear leukocytes migration
2. ?phagocytosis
3. ?intracellular killing
4. ?chemotaxis

Fig no.7
Depending on the type of wound and if it is infected, the appropriate medication for diabetic foot wounds will vary:-
1.Antibiotics: Use oral antibiotics for milder infections and broad spectrum antibiotics such as ampicillin, levofloxacin, ciprofloxacin, cefuroxime, or cilastatin for more serious infections.
2.Agents that promote wound healing: Among the wound-healing substances that could be useful for diabetic foot ulcers are
3.Regranex becaplermin gel: An FDA-approved gel that encourages healthy granulating wounds to heal
4.Metronidazole : marketed under the brands Metrogel and Metrocream Notate, reduces edema and redness.
5.Hyperbaric oxygen therapy: is a treatment that accelerates healing by allowing patients to breathe pure oxygen in a contained space.
6.Topical Treatments: Promote wound healing through the use of growth factors, antimicrobials, and advanced dressings.
7. A novel treatment that could aid in wound healing is neuropeptide.
Antibiotic treatment : typically lasts 1-2 weeks for mild to moderate illnesses and more than 2 weeks for severe infections. • If contaminated bone is not removed, antibiotics are prescribed for 6-8 weeks based on culture findings. • If all diseased bone is removed, a shorter course of antibiotics (1-2 weeks) may suffice, similar to soft tissue infection.
The type of antibiotics used to treat depends upon the type of infections and the type of bacteria causing it :
- Mild infections : treated with oral antibiotics like cephalexin, dicloxacillin, amoxicillin-clavulanate or clindamycin.
- Moderate infections: Treated with parenteral antibiotics like amoxicillin-clavulanate or piperacillin- tazobactam Plus amikacin or gentamycin.
- Severe infections: treated with parenteral antibiotics like vancomycin, teicoplanin, imipenem/meropenem plus amikacin or gentamycin
Evaluating Peripheral Neuropathy:
Monofilament Testing : Assess light touch sensation by applying a standardized nylon filament to various areas of the foot.
Vibration Perception: Use a tuning fork to evaluate the patient's ability to detect vibrations, which can indicate nerve damage.
Reflex Assessment: Check deep tendon reflexes, such as the ankle jerk, to identify potential nerve impairment.
Foot Deformities
Bunions: Bony growths at the base of the big toe, often caused by pressure and poor foot mechanics.
Hammertoes: Toes that bend at the middle joint, leading to increased pressure and friction.
Charcot Foot: A severe deformity caused by weakening of the bones and joints, leading to collapse of the foot's structure.
The neuropathic joint (charcot’s joint):
•Charcoat’s foot have loss of pain sensation and rarefaction of the bones and Abnormal mechanical stresses damages the susceptible bones by relatively minor trauma
An inflammatory disorder called Charcot neuroarthropathy causes bone fractures, joint dislocations, and osseous subluxation, which results in structural remodeling of the foot. Because Charcot neuroarthropathy includes several stages, a changeable timetable, and conflicting views regarding causality, it can be difficult to manage. It frequently results in bone infections and neuropathic ulcers.
• bony changes are most often seen at all:
-Ankle joint
-Tarsal-metatarsal region of the foot
-Metatarso- phalanges region
•When diagnosis is difficult : used gallium white cell scan and magnetic resonance imaging scan
charcot's joint

fig no.8
•Computer tomography (CT) and magnetic resonance imaging (MRI) can be used to efficiently inform treatment choices. Surgical debridement is essential for controlling the cause and removing necrotic tissue, especially when infections are deep or severe. •Unusual swelling, exudate, maceration, redness, itching, irritation, and odor are early signs of DFU.
•The most obvious indication of severe DFU is the black tissue, or escha, that surrounds the ulcer region. In western nations, the most frequent reason diabetics are admitted to hospitals is foot ulcers. In those with diabetes, foot ulcers occur about 22% of the time each year.
•The benefits of vitamin D include better glycemic management. Therefore, it is advised to routinely check vitamin D levels in diabetics who have foot ulcers. Even the tenuous connection between vitamin D levels and DFU is yet unknown, but this vitamin may be a useful treatment for elderly diabetics who have low levels of this nutrient and poor glycemic control. A factor in diabetic peripheral neuropathy is vitamin D. Healing of wounds Disease of the peripheral arteries Among other things, pro-inflammatory cytokine production (IL-6) and TNF alpha can enhance angiogenesis
Objective wound measurement: Every patient's wound's length and width must be measured at least once every seven days. If planimetry is not accessible, a more basic ruler must be used. All results must be recorded in medical records. The vague but widely used adage "a wound looks good" is not a suitable objective wound assessment and is not to be applied. When assessing the healing of diabetic foot wounds and the efficacy of therapeutic therapy, sequential measures of wound area are useful.
Physiological History:
Because they don't undergo regular pedal exams, patients often arrive with the initial complaint of finding blood on their floors or in their socks. A comprehensive history of the ulceration itself should cover its nature, location, duration, and onset, as well as its course, things that aggravate it and relieve its accompanying symptoms, and any therapies or dressings.the patient's occupation and the frequency of positions that put additional strain on the area can be inferred from their social history. Because alcohol can cause neuropathy and nicotine can reduce blood flow to a region, past substance usage should be taken into account. •Surgical procedures including skin flaps, grafts, and debridement are examples of traditional wound care. Skin replacements, topical formulations, scaffold-based skin grafts, and hydrogel-based skin dressings are examples of non-surgical procedures. Utilizing growth factors, nanoparticles, and bioactive materials in wound dressings are examples of more recent methods. Biomaterials, cells, and growth factors are also being used to create bioengineered skin substitutes. Additional methods include vacuum-assisted wound closure, growth factor/cytokine therapy, stem cell therapy, and bio- or 3D-printed wound dressings.
Non limb threatening:
Initially treated as outpatients, these patients are admitted to the hospital only if or when their condition worsens or no improvement is observed within 48 to 72 hours. • If an ulcer is present, antibiotic treatment is started. They clean and debride the ulcer. • After that, ulcer management is carried out as described earlier. • Other co-morbidities are stabilized and hyperglycemia is corrected at the same time. • After 48 to 72 hours, the response to treatment is reassessed, and possibly further action is required. • Preventive measures, patient education, podiatric care, and orthotic treatment are also implemented.
Severe limb and life threatening infections:
Gram-positive and gram-negative bacteria, anaerobic organisms, and enterococci are all part of the polymicrobial character of severe limb and life-threatening infections.• Wounds that have been soaked or treated with wet dressings are frequently the source of Pseudomonas species. • Patients who have previously undergone cephalosporin therapy are frequently used to cultivate enterococci. • Wounds with necrosis, deep tissue involvement, or a foul odor are home to anaerobes. • MRSA is frequently contracted during an earlier hospital stay. • Common isolates of the aforementioned pathogens should be covered by empirical intravenous broad-spectrum antibiotic therapy in these individuals, which should then be modified based on culture and sensitivity findings. To rule out super infection, periodic deep tissue cultures should be performed for recurrent infections even when antibiotic medication is still being administered. In the event that MRSA is isolated, prompt and adequate treatment is necessary.
*You can help to maintain your feet healthy by following ways :
1.Check your feet every day. Look for wounds, redness, and other changes in the skin and toenails, such as warts or other areas where your shoes may rub. Also, make sure to inspect the bottoms of your feet.
2. Wash your feet every day. Use warm water and soap. Don't wet your feet because it can cause your skin to dry out.After you've dried your feet, apply talcum powder or cornstarch between your toes.They absorb moisture, which can cause infection. If you use lotion, avoid applying it between your toes.
3.Ask your doctor how to safely remove corns and calluses.Thick skin on your foot can rub and cause ulcers. However, removing it incorrectly can cause damage to your skin. So, avoid cutting the skin and using medicated pads or liquid removers.
4. Trim your toenails straight across with a clipper. If you find it difficult to trim your own toenails, or if they are thick or curl into the skin, hire a podiatrist (foot doctor).
5. Always wear well-fitting shoes, socks, or slippers to protect your feet while walking. You do not want to walk barefoot, even indoors. Make sure your shoes are smooth inside. A seam or stone in your shoe may rub your skin raw.
6.Protecting your feet from the heat and cold. Use sunscreen on exposed areas.Don't stroll barefoot on the beach. In cold weather, wear warm socks instead of putting your feet near a heater or fireplace.
7.Keeping blood circulating via your feet. Sit with your feet up. Wiggle your toes and circle your feet all day. Do not wear tight socks. Get lots of activities that isn't too strenuous on your feet, like walking.
8. Having your feet checked at your health-care appointments. Even if you haven't experienced any symptoms, it's a good idea to have your provider examine your feet.
•Modern methods to prevent :
include vacuum-assisted wound closure, growth factor/cytokine therapy, stem cell therapy, and bioengineered skin substitutes have supplanted traditional wound therapies.But the majority of these tactics are ineffective and not well-tested. Therefore, additional study is needed to create novel, patient-friendly, and economical methods for cutaneous wound healing.

fig 9
1.Techniques of scaffold construction for DFU Traditional therapeutic approaches, such wound dressings, are known to have undesirable mechanical qualities despite being biocompatible. Thus, an attempt has been made to create 3D scaffolds, which can be manufactured using a variety of techniques, such as electrospinning and 3D printing technologies. In order to facilitate the adhesion and proliferation of cells necessary for effective wound healing, extremely porous scaffolds that closely resemble the extracellular matrix are needed.
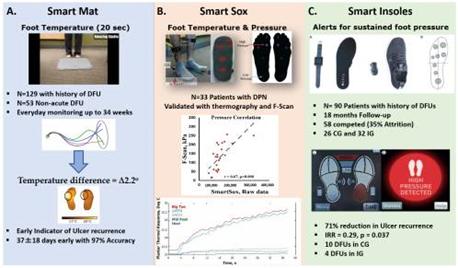
fig 10
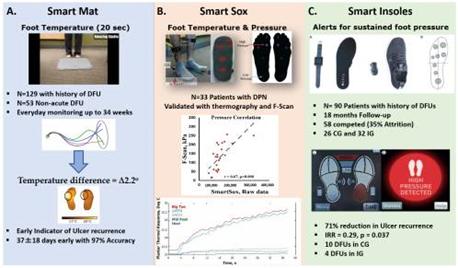
Recent advancements in technology have made it possible to remotely monitor early digital biomarkers of DFU, which can help triage patients at high risk of DFU and give high-sensitivity screening tools. These technologies consider the fact that the majority of foot ulcers are caused by repeated trauma at the sole's pressure points over a period of days [10]. Plantar tissue stress (PTS) increases in the foot region subjected to high pressure as a result of untreated repeated trauma [13]. Plantar pressure, shear stress, and the amount of time spent without protective footwear (adherence) are only a few of the mechanical elements that PTS represents.
*A pressure sensor-embedded insole that transforms plantar pressure into an electrical signal and a transmitter that sends out an alarm in the form of tactile, visual, or aural feedback are the two main parts of a typical smart insole system [37]. Three sites beneath the metatarsal heads, two beneath the lateral plantar surface, one beneath the heel, one beneath the hallux, and one beneath the lesser toes are often where pressure sensors are positioned.
Reconstructive treatments : When the diabetic foot ulcer's area hasn't shrunk by more than 10%, these treatments might be helpful.Reconstructive treatments (such as meshed and split-thickness skin grafts and local and free muscle flaps) may be effective in preventing amputations, despite the high rate of complications associated with plastic surgery. 52 percent of patients with diabetic foot ulcers who had soft tissue reconstructive surgery had osteomyelitis, and 42 percent of the afflicted limbs needed revascularization prior to reconstruction.
Plantar pressure reduction (offloading) :
causes trauma to heal and ant lowing to heal. •Completely weightless. • Gold standard total contact cast Boots or a foot castWalking braces that are removable and have rocker bottom soles; total contact orthoses, which are customized walking braces; braces that support the patellar tendon; wedge or half shoes; and healing sandals, which are surgical shoes with molded plastizote insoles • Comfort dressings such as felt, foam, and felted-foam Shoe cuts (medial, lateral, dorsal, or toe box pressure points). • Assistance aids, such as canes, walkers, and crutches.
Importance of Early Detection:
Prevent Complications: Early detection and proper management of diabetic foot ulcers can help prevent serious complications, such as amputation.
Promote Healing: Timely treatment can improve the chances of the ulcer healing, reducing the risk of infection and further tissue damage.
Improve Quality of Life: Effective management of diabetic foot ulcers can help maintain mobility and independence, leading to a better quality of life.
CONCLUSION
To maintain optimal foot health, especially for individuals with diabetes, it's essential to adopt a proactive approach. Start by wearing well-fitting, supportive shoes to protect your feet from injuries. Keeping your feet clean and moisturized can prevent common skin issues, while maintaining proper blood glucose levels will help minimize risks associated with diabetes. Regular physical activity not only improves strength and overall health but also aids in circulation, which is crucial for foot health. Simple exercises like wiggling your toes and moving your ankles for a few minutes multiple times daily can further support blood flow to the feet. Additionally, diabetic patients should have access to a skilled podiatrist and benefit from coordinated care among healthcare professionals, including podiatrists, orthotists, nurses, physicians, and surgeons, for comprehensive foot care. Employing advanced wound care techniques is also critical for promoting healing and preventing infections, ensuring a more effective management of diabetic foot complications.
REFERENCES
- World J Clin Cases. (2023). *World Journal of Clinical Cases*, 11(8), 1684–1693. https://doi.org/10.12998/wjcc.v11.i8.1684
- Harold Brem, M.D. Peter Sheehan, M.D. Harvey J.Rosenberg, B.A. Jillian S. Schneider, M.S. Andrew J. M. Boulton, M.D. New York, N.Y.; Miami, Fla.; and Manchester, United Kingdom
- Baker N. Prevention, screening and referral of the diabetic foot in primary care. Diabetes & Primary Care 2011; 13 (4):225-34.
- Priyadarshini Shanmugam, JeyaJournal of clinical and diagnostic research: JCDR 7 (3), 441, 2013
- Jeffcoate, W.J., & Harding, K.G. (2003). *The Lancet*. Retrieved from thelancet.com
- Boyko, E.J., Ahroni, J.H., Stensel, V., Forsberg, R.C., et al. (1999). *Diabetes*, American Diabetes Association.
- Cavanagh, P.R., Lipsky, B.A., Bradbury, A.W., & Botek, G. (2005). *The Lancet*. Retrieved from thelancet.com
- Armstrong, D.G., Tan, T.W., Boulton, A.J.M., & Bus, S.A. (2023). *JAMA*. Retrieved from jamanetwork.com
- Frykberg, R.G. (2002). *American Family Physician*. Retrieved from aafp.org
- Fard, A.S., Esmaelzadeh, M., et al. (2007). *International Journal of ...*, Wiley Online Library.
- Reardon, R., Simring, D., Kim, B., et al. (2020). *Australian Journal of ...*, Retrieved from search.informit.org
- Armstrong, D.G., & Lavery, L.A. (1998). *American Family Physician*. Retrieved from aafp.org


 Pradnya More*
Pradnya More*
 Pooja Surve
Pooja Surve
 Suvidha Kabadi
Suvidha Kabadi
 Shravani mhatre
Shravani mhatre
 Kashish punamiya
Kashish punamiya









 10.5281/zenodo.14547577
10.5281/zenodo.14547577