Abstract
Dysmenorrhea is a recurring ache in the lower abdomen or pelvis that can spread to the legs and back. It can occur before or during the menstrual cycle, or both. Parkinson's disease (PD) affects 45% to 95% of reproductive-aged women worldwide, with 2% to 29% experiencing severe discomfort. It is thought that prostaglandins (PGs) are the major cause of dysmenorrhea. Secondary dysmenorrhea refers to menstrual discomfort caused by an underlying sickness, ailment, or anatomical aberration inside or outside the uterus. Dysmenorrhea is caused by increased production of prostaglandin F2? (PGF2?) and prostaglandin E2 (PGE2) in the uterus during endometrial sloughing. The etiology of the disorder is not fully known. Both primary and secondary dysmenorrhea begin with similar therapies. The first suggested baseline therapies are medical management, supportive therapy, patient education, and reassurance.
Keywords
Primary Dysmenorrhea, Prostaglandins, Cyclooxygenase, Menstrual cycle, Nonsteroidal anti-inflammatory drugs
Introduction
Dysmenorrhea is a cyclical pain in the lower abdomen or pelvis that can also radiate to the thighs and back. It can happen either before or during the menstrual cycle, or both. Lower abdominal pain and cramps occur once regular ovulation is established. It starts shortly after the menarche. It is the most typical gynecologic problem that affects female adolescents and adults. A wide range of emotional and physical issues that arise around the time of menstruation are collectively referred to as menstruation-associated symptoms.[1] Menstrual symptoms include headache, nausea, fatigue, lightheadedness, and diarrhea, to name a few frequent ones. Usually lasting the first 24 to 48 hours, symptoms begin at the initiation of menstrual flow or appear a few hours before or following onset. Dysmenorrhea symptoms include emotional exhaustion, distension of the abdomen, nausea, vomiting, and disturbed sleep. Primary dysmenorrhea's causes have not been well investigated, but common risk factors include smoking, not using oral contraceptives, having a positive family history of the condition, experiencing more severe bleeding, having a shorter or longer monthly period interval, stress, and irregular menstrual cycles. [2]
Since different women experience primary dysmenorrhea in different ways and since there is variation in the diagnostic criteria that are frequently utilized, it is challenging to determine the epidemiology of this condition. Estimates of prevalence for women and adolescents range from 25% to 90%. Research from India revealed a 50–87.8% prevalence range. According to other research, up to 90% of women who are fertile experience dysmenorrhea, albeit to differing degrees. For 5-20% of women who report severe dysmenorrhea or discomfort that keeps them from engaging in their regular activities, pain is a serious concern. It is estimated that the yearly economic loss in the United States is 600 million work hours or two billion dollars. Dysmenorrhea has a wide range of effects and is significant for reasons beyond only its socioeconomic effects. [3]
Primary dysmenorrhea can have significant impacts on daily activities, academic performance, social withdrawal, absenteeism from work or school, and medical costs. Treatment methods to lessen dysmenorrheic pain include the use of oral contraceptives, non-steroidal anti-inflammatory drugs, herbal remedies, massage, and lifestyle changes. The prevalence, severity, impact, and contributing causes of primary dysmenorrhea in Ethiopian female preparatory school students are little documented. [1]While the exact origin of dysmenorrhea remains unknown, prostaglandin synthesis during an ovulatory cycle in the endometrium is thought to be the source of pain during or around menstruation. According to certain accounts, dysmenorrheic women had twice as much prostaglandin F2? in their menstrual fluid from tampons as non-dysmenorrheic women. Patients with dysmenorrhea have reported a considerable benefit with prostaglandin inhibitors as a corrective treatment. [4] Though there is evidence linking prostaglandin levels to dysmenorrhea, it is crucial to understand that menstrual pain cannot be explained by the cyclical generation of a single hormone. Hormonal patterns in women who experience dysmenorrhea may change in intricate ways throughout the menstrual cycle. Prostaglandin inhibitor analgesics are the most effective type of analgesics for treating dysmenorrhea, as their goal is to relieve symptoms. This research aimed to determine the frequency of dysmenorrhea and menstrual symptoms among Indian females, the effect it has on their academic performance, and the methods used for treatment. [5] There is currently a substantial body of research on dysmenorrhea; however, the conclusions drawn from these studies may differ due to the various definitions of Parkinson's disease (PD) used in the studies as well as variations in the study population's lifestyle, culture, genetics, and level of social and personal stress. Furthermore, some research on dysmenorrhea (both primary and secondary dysmenorrhea) was carried out, which could potentially lead to study heterogeneity. The majority of people at risk for Parkinson's disease (PD) are students, and PD is the main reason behind students' frequent, short-term absences from school. By teaching students how to handle PD, research on the subject could greatly lessen its effects. Thus, the sole focus of our current study is PD in students, and our objectives are to clarify the prevalence of PD today, as well as any associated risk factors, and investigate any dynamic shifts in the incidence of PD over time. [6]
EPIDEMIOLOGY
In females of reproductive age, the prevalence of Parkinson's disease (PD) varies globally between 45% and 95%, with 2% to 29% reporting severe pain. The observed variance in the rates could potentially be attributed to variations in the PD assessment methodology, the demographics that were chosen, age and ethnic groups, and variations in pain perception within the populations. Younger women (less than 24 years old) reported a higher prevalence (70% to 90%). The most often reported menstruation and gynecological condition is primary dysmenorrhea. [7] A significant number of women who are of reproductive age are affected. Millions of women are impacted by it while they are fertile. Previous epidemiological studies have indicated that the prevalence of dysmenorrhea varies around the globe, from 41.7% to 94%. The frequency of primary dysmenorrhea varies from 51.1% to 88.1% in sub-Saharan Africa.6,7 In Ethiopia, the frequency of primary dysmenorrhea varies from 62.3% to 85.4%. [8]
ETIOLOGY
Numerous theories have been put out to explain the genesis of dysmenorrhea since the 1960s. These hypotheses include etiologies that are psychological, biological, and anatomical. The anatomical theory highlights anomalies in the length or form of the cervix as well as improper uterine position. a favorable relationship between the volume and severity of dysmenorrhea and cervical length. Other investigations have found that the biochemical explanation provides the strongest supporting data. The age (usually) up to 30 years old, smoking, dieting attempts, higher or lower than normal BMI, anxiety and depression, longer menstrual cycles, younger menarche age, nulliparity, history of sexual assault, previous cesarean section with incomplete uterine scar healing (uterine niche), longer and heavier menstrual flow, family history of dysmenorrhea, and disruption of social networks are risk factors associated with dysmenorrhea. [7,9]
Primary Dysmenorrhea:
It is believed that prostaglandins (PGs) are the primary cause of dysmenorrhea. Women with dysmenorrhea have been found to have higher levels of PGs in their endometrial tissue and menstrual fluid. The menstrual cycle's declining hormone levels cause endometrial shedding to start. [6] The endometrial cells release progesterone throughout the period of endometrial shedding at the onset of menstruation. Uterine contractions are brought on by PGs, and the severity of the cramps is correlated with the amount of PGs released. Tissue hypoxia and ischemia brought on by uterine contractions result in pain, occasionally accompanied by nausea and diarrhea. [8]
Secondary Dysmenorrhea:
Menstrual pain brought on by an underlying illness, condition, or structural anomaly inside or outside the uterus is known as secondary dysmenorrhea. Women may experience it at any point following menarche. For women in their 30s or 40s, it may be their first symptom. Different pain levels and occasionally additional symptoms like dyspareunia, menorrhagia, intermenstrual bleeding, and postcoital hemorrhage might be linked to secondary dysmenorrhea. [9] Secondary dysmenorrhea can be caused by a variety of common conditions, such as endometriosis, adenomyosis, big cesarean scar niche, fibroids, endometrial polyps, pelvic inflammatory disease, and possibly the use of an intrauterine contraceptive method. The prevalence of endometriosis in women with dysmenorrhea may reach 29%. Up to 35% of patients with NSAID-resistant dysmenorrhea may also have endometriosis. Another prevalent underlying condition linked to secondary dysmenorrhea is adenomyosis. Reproductive tract anomalies affect up to 3.8% of young women, and subsequent dysmenorrhea may be linked to both obstructive and non-obstructive defects. [10]
PATHOPHYSIOLOGY
Current data indicates that the pathogenesis of dysmenorrhea is caused by increased secretion of prostaglandin F2? (PGF2?) and prostaglandin E2 (PGE2) in the uterus during endometrial sloughing, even if the pathophysiology of the condition is not entirely understood. These prostaglandins contribute to uterine ischemia and anaerobic metabolite synthesis by tightening vasoconstriction and myometrial contractions. Pelvic discomfort eventually comes from the hypersensitization of pain fibers caused by this. [11] Prostaglandin synthesis occurs via the cyclooxygenase (COX) route, which mediates the arachidonic acid cascade. Progesterone levels control the formation of arachidonic acid via activating the lysosomal enzyme phospholipase A2. The middle of the luteal phase, which is the latter part of the menstrual cycle that follows ovulation, is when the progesterone level peaks. The corpus luteum degenerates and the level of progesterone in the blood drops if conception is unsuccessful. Progesterone levels are rapidly declining, linked to endometrial sloughing, menstrual bleeding, and the release of lysosomal enzymes, which produce arachidonic acid and prostaglandins. [12] In the late luteal phase, endometrial prostaglandin levels are higher in women who have regular menstrual cycles. Nonetheless, several investigations that employed endometrial biopsies and menstrual fluids to evaluate prostaglandin concentrations during the luteal phase found that dysmenorrheic females had higher prostaglandin levels than eumenorrheic females. Consequently, a direct correlation exists between increased endometrial concentrations of PGF2? and PGE2 and monthly cramps, pain intensity, and related symptoms. [13] The cyclooxygenase COX-2 is highly expressed during menstruation, and this has led to the usage of NSAIDs as a form of treatment, as will be discussed below. Primary dysmenorrhea has also been connected to vasopressin. Vasopressin's vasoconstrictive effects might result in ischemia discomfort and enhance uterine contractility. [14] Patients with dysmenorrhea have greater levels of leukotrienes C4 and D4, which also seem to be linked to an increase in uterine contractions. Additionally, during the first two days of menstruation, when dysmenorrhea is most common and severe, uterine contractility is more noticeable. The most frequent causes of secondary dysmenorrhea in premenopausal women are adenomyosis and endometriosis. [15]
CLINICAL PRESENTATION
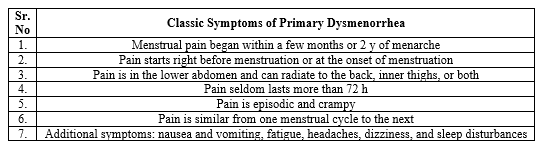
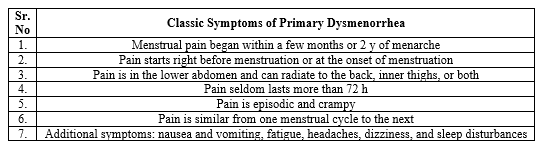
Table No 1: Classic Symptoms Of Primary Dysmenorrhea
DIAGNOSIS
The commencement of ovulatory cycles, which typically occurs 6–12 months following menarche but in certain teens can occur up to 2 years later, is when primary dysmenorrhea first appears. In a significant proportion of cases, its frequency declines with age. Patients report cramping, and erratic pain that starts either before or right after bleeding starts and lasts for up to 72 hours. The upper thigh, back, or both may experience radiating pain from the suprapubic area. Intense pain typically peaks 24–36 hours after the menstrual cycle begins, and it seldom lasts more than a few days. Nausea, vomiting, bloating, and diarrhea are other symptoms. Risk factors for dysmenorrhea include age under 30, body mass index (BMI, defined as weight in kilograms divided by height in meters squared) less than 20, smoking, menarche before the age of 12, longer menstrual cycles or duration of bleeding, irregular or heavy menstrual flow, a history of sexual assault, and a family history of dysmenorrhea. [16] Dysmenorrhea is typically identified as primary rather than secondary in adult study participants based on history, normal examination findings, and the absence of other known causes of menstrual pain. As women age, there is a general decline in the prevalence and severity of moderate to severe primary dysmenorrhea, and childbearing is linked to this decline. Women who had miscarriages or abortions during their pregnancies do not show any improvement. Primary dysmenorrhea is consistent with a physical examination that finds a normal-sized, mobile, non-tender uterus and does not show signs of mucopurulent discharge, uterosacral nodularity, or an adnexal mass. [17] There is currently no test to confirm the diagnosis, but patients with the classic presentation are candidates for empirical therapy. In adolescents with a classic history of primary dysmenorrhea, a pelvic examination is not required to begin treatment. As a result, telehealth platforms can be used for initial treatment, and it is not necessary to postpone it if a face-to-face visit is not convenient for the patient or cannot be arranged in any other way (e.g., during periods of reduced office hours related to contagion-containment strategies). Evaluation for secondary amenorrhea reasons should be prompted by an unusual presentation, aberrant physical examination findings, or lack of response to medicinal therapy. If the patient's symptoms are not improving with empirical treatment, a pelvic examination and radiologic tests, such as an abdominal or transvaginal ultrasound scan, should be carried out. Surgical assessment could be necessary in light of the results or a clinical suspicion. [18]
TREATMENT
The goal of dysmenorrhea treatment is to give patients enough pain relief to enable them to carry out the majority of their everyday tasks. Both primary and secondary dysmenorrhea start with comparable treatments. The first recommended baseline interventions are medical management, supportive therapy, patient education, and reassurance. A possible secondary dysmenorrhea cause examination may be necessary if symptoms do not improve with first-line therapy. The two categories of therapy techniques are pharmacologic and nonpharmacologic, as shown below. Tramadol and opioids shouldn't be used to treat dysmenorrhea regularly. [19]
Nonpharmacological Treatment
Heat application, exercise, and diet:
The first three components of a baseline intervention are heat application and exercise. With no negative side effects, heat applied to the lower abdomen may be more beneficial than acetaminophen and as effective as NSAIDs. For many patients, this is the first therapy option of choice. With no negative side effects, heat applied to the lower abdomen may be more beneficial than acetaminophen and as effective as NSAIDs. For many patients, this is the first therapy option of choice. [20] There is evidence to suggest that regular exercise can help treat dysmenorrhea, although it is unclear what kind, how long, and how often to exercise. For all patients, a moderate exercise regimen is advised. A balanced diet high in vitamins and minerals and an active lifestyle are generally advised for improved health results. Such dietary and lifestyle adjustments may be very helpful in lessening the severity of dysmenorrhea. Chinese medicine, plant-based therapy, and dietary supplements are among complementary and alternative medicine modalities used to treat dysmenorrhea. [21] However, the FDA does not regulate them. All things considered, there is not enough data to support the use of any additional dietary or herbal therapy. PG levels and discomfort related to primary dysmenorrhea have not been improved by spinal manipulation, according to at least one excellent randomized controlled experiment. [22]
Acupuncture, transcutaneous electrical nerve stimulation, and behavioral counseling:
A few studies that lack rigorous methodological standards and active comparisons lend credence to the efficacy of acupuncture. As a second-line nonpharmacological treatment, behavioral counseling and transcutaneous electrical nerve stimulation may be utilized. [23]
Pharmacological Treatment
Nonsteroidal anti-inflammatory drugs (NSAIDs) for the pharmacologic treatment of dysmenorrhea, and nonsteroidal anti-inflammatory medications (NSAIDs) are regarded as the first line of treatment. NSAIDs are more successful than placebos in treating dysmenorrhea. NSAIDs work by preventing the synthesis of PG by inhibiting cyclooxygenase enzymes. It has been demonstrated that taking an NSAID regularly, beginning one to two days before pain starts, is more effective than taking it on an as-needed basis. Marjoribanks et al. concluded that, in general, no NSAID is safer or more effective than another in a comprehensive study that compared various NSAIDs to a placebo in the treatment of dysmenorrhea. [24] Flurbiprofen and tiaprofenic acid were found to be more effective in treating dysmenorrhea in a meta-analysis of 70 studies. Nevertheless, tiaprofenic acid is not readily available in the United States. Regretfully, data suggests that 20% of those suffering from dysmenorrhea may not benefit from NSAID therapy. We refer to this as dysmenorrhea resistant to NSAIDs. Similar to mefenamic acid, fenamates may be somewhat more effective than the derivatives of phenyl propionic acid (ibuprofen, naproxen) due to their ability to both inhibit and prevent the synthesis of PGs. Mefenamic acid 500 mg at the onset of the menstrual cycle or pain, then 250 mg every 6 hours for a maximum of three days, may be beneficial. [22] According to a study, ibuprofen and fenamates are the safer and more effective options. It has been suggested to take ibuprofen 800 mg every 8 hours or naproxen 440 mg to 550 mg as an initial dose and thereafter 220 mg to 550 mg every 12 hours on a scheduled basis. When it comes to effectiveness, NSAIDs outperform paracetamol (acetaminophen). When NSAIDs are not advised, paracetamol is still a suitable substitute. Previously used to treat dysmenorrhea, celecoxib is a COX-2 selective NSAID; however, because of its cardiovascular side effects, it is no longer advised. You should pay attention to black box warnings about the possibility of severe bad consequences. Since PGs are required for ovulation, COX-2 selective NSAIDs have also been connected to delayed ovulation. [21,23] Patients who cannot take NSAIDs may be able to get pain relief with Acetaminophen. Acetaminophen combined with caffeine or pamabrom, two diuretics, has been demonstrated to lessen dysmenorrhea pain. [25]
In comparison to a placebo, Hormonal contraception including progesterone and estrogen in the form of pills, patches, or vaginal rings is said to be more effective at lowering dysmenorrheic pain. All combination pills that were available offered comparable pain relief without any variations in effectiveness. Due to small sample numbers and sparse comparison data, some studies have contested the efficacy of combination hormonal contraceptives as a treatment for dysmenorrhea. [20,24] Combining progesterone and estrogen contraceptives will prevent ovulation and restrict endometrial development. Menses become lighter and less accompanied by uterine contractions as the endometrium thins over time. Menstrual pain is thereby lessened as a result. Combination birth control pills (COCs) function by reducing leukotriene and prostaglandin synthesis. Women on COCs had low amounts of PGs in their menstrual fluid. Users of the contraceptive pill seem to experience dysmenorrhea at much lower rates and require fewer extra analgesics for treatment. Even more effective than cyclic therapy in treating dysmenorrhea are continuous hormonal contraceptive regimens that exclude placebo pills. [26] Whether used as pills, implants, IUDs, or intramuscular injections, Progestin-only contraception is most suited for individuals who have endometriosis-related secondary dysmenorrhea. It's unclear if they work well as a primary dysmenorrhea treatment. Progesterone inhibits ovulation and causes atrophy of the uterine lining. Oral progesterone formulations like dienogest and norethindrone acetate are explicitly advised as the first line of treatment for secondary dysmenorrhea brought on by endometriosis. [19,25] As a second-line pharmaceutical intervention, Gonadotropin-releasing hormone agonists and antagonists may be prescribed. Goserelin, leuprolide acetate, and nafarelin are examples of GnRH agonists. Elagolix is the antagonist of GnRH. These are useful remedies for endometriosis-related dysmenorrhea, but their cost and side effects may prevent them from being used widely, particularly when add-back progesterone and estrogen therapy are not used. Following a surgical diagnosis of endometriosis, the American Society of Reproductive Medicine advises treating dysmenorrhea with gonadotropin-releasing hormone agonists. These drugs aren't regarded as long-term treatments, though. [27] Since they cause amenorrhea, Aromatase inhibitors can be used to treat secondary dysmenorrhea. However, side effects, including decreased bone mineral density, can make use unfeasible, particularly in the absence of concurrent add-back medication for progesterone and estrogen. A vasodilator lessens the pain associated with primary dysmenorrhea. It encourages the uterus' smooth muscle to relax. Smooth muscle is similarly relaxed by nitric oxide donor medications such as transdermal nitroglycerin or 0.1 mg glyceryl trinitrate patches. Vasodilators have serious adverse effects, including headaches and dizziness, which is why they are usually not used as a first line of treatment for dysmenorrhea. The effectiveness of using vasodilators as a treatment for dysmenorrhea requires more research. Calcium channel blockers, reduce dysmenorrhea discomfort and stop uterine contractions. Examples of these blockers include nifedipine (20–40 mg). However, use may be restricted due to side effects such as flushing, tachycardia, and headache. [24,26,27]
Vasopressin/oxytocin receptor agonists are known to induce myometrial contractions, they have been investigated as a potential treatment for dysmenorrhea. For NSAID-resistant dysmenorrhea, atosiban and SR49059 have both been examined; however, no decisions have been made regarding when, how, or how well to administer them. Since dysmenorrhea has been linked to muscle spasms, Antispasmodics have been researched as a possible treatment. Because hyoscine butyl bromide has anticholinergic actions on muscarinic receptors, which cause smooth muscle relaxation, it has been used worldwide to treat dysmenorrhea. Hyoscyamine sulfate is a comparable drug that is available in the US but has not received FDA approval for the treatment of dysmenorrhea. An antispasmodic drug taken in addition to an NSAID produced better outcomes in a randomized controlled trial than an NSAID taken alone. [11,28] Due to its vasodilator and muscle-relaxing qualities, Magnesium has been demonstrated to lessen dysmenorrhea pain. It has been determined that magnesium should be used in conjunction with other therapies rather than as a stand-alone treatment for dysmenorrhea due to a lack of formulation and dosage guidelines. [26]
Surgical Options
Surgical options should only be used if there is not a satisfactory response to trials of medical management.
If the patient has a high probability of pathology being the underlying cause of the dysmenorrhea and if relief has not been achieved after 3 to 6 months of the first pharmacologic treatment, Laparoscopy is the next step in the examination and treatment of dysmenorrhea. The resection of endometriotic implants is the aim of surgery. It is advised to use progesterone alone, combined birth control, or GnRH agonist medication postoperatively to suppress any residual or microscopic endometriosis. In women who are finished having children and have heavy monthly bleeding, Endometrial ablation is a possibility to think about if medication therapy has not produced satisfying outcomes. [29]Women who have exhausted all other options for treatment may be offered a Hysterectomy as a last resort. Depending on the cause of the dysmenorrhea, the patient's age, and the likelihood that more ovaries would need to be removed in the future, ovarian excision may be a possibility. Nerve transection procedures, such as presacral neurectomy and laparoscopic uterine nerve ablation, are not advised, with the possible exception of a small number of patients who have intractable midline pelvic pain. These processes need to be studied further. It has been observed that pain returns after surgery when nerve regeneration takes place. Significant side effects include constipation, urinary dysfunction, and pelvic organ prolapse. [30]
CONCLUSION
In conclusion, dysmenorrhea is a common gynecologic problem that affects female adolescents and adults, with a wide range of symptoms and impacts on daily life. Primary dysmenorrhea is believed to be caused by prostaglandins, while secondary dysmenorrhea can be caused by underlying conditions. The prevalence and severity of dysmenorrhea vary globally, and treatment options include oral contraceptives, non-steroidal anti-inflammatory drugs, and lifestyle changes. Further research is needed to understand the epidemiology and treatment of dysmenorrhea in different populations.
REFERENCES
- Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H. M. J. (2022). Primary dysmenorrhea: Pathophysiology, diagnosis, and treatment updates. Korean Journal of Family Medicine, 43(2), 101–108.
- Chen, C. X., Shieh, C., Draucker, C. B., & Carpenter, J. S. (2018). Reasons women do not seek health care for dysmenorrhea. Journal of Clinical Nursing, 27(1–2), e301–e308.
- Sharghi, M., Mansurkhani, S. M., Ashtary-Larky, D., Kooti, W., Niksefat, M., Firoozbakht, M., Behzadifar, M., Azami, M., Servatyari, K., & Jouybari, L. (2019). An update and systematic review on the treatment of primary dysmenorrhea. JBRA Assisted Reproduction.
- Arra-Fernandez, M. L., Onieva-Zafra, M. D., Abreu-Sanchez, A., Ramos-Pichardo, J. D., Iglesias-Lopez, M. T., & Fernandez-Martinez, E. (2020). Management of primary dysmenorrhea among university students in the south of Spain and family influence. Int J Environ Res Public Health, 17.
- Latthe, P., Mignini, L., Gray, R., Hills, R., & Khan, K. (2006). Factors predisposing women to chronic pelvic pain: systematic review. BMJ (Clinical Research Ed.), 332(7544), 749–755.
- Wong, C. L. (2018). Health-related quality of life among Chinese adolescent girls with Dysmenorrhoea. Reproductive Health, 15(1).
- Agarwal, A. K., & Agarwal, A. (2010). A study of dysmenorrhea during menstruation in adolescent girls. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine, 35(1), 159–164.
- Proctor, M. L., Latthe, P. M., Farquhar, C. M., Khan, K. S., & Johnson, N. P. (2005). Surgical interruption of pelvic nerve pathways for primary and secondary dysmenorrhoea. Cochrane Database of Systematic Reviews, 2010(4), CD001896.
- Proctor, M., Latthe, P., Farquhar, C., Khan, K., & Johnson, N. (2005). Surgical interruption of pelvic nerve pathways for primary and secondary dysmenorrhoea. The Cochrane Library, 2010(11).
- Chauhan, M., & Kala, J. (2012). Relation between dysmenorrhea and body mass index in adolescents with rural versus urban variation. Journal of Obstetrics and Gynaecology of India, 62(4), 442–445.
- Ferries-Rowe, E., Corey, E., & Archer, J. S. (2020). Primary dysmenorrhea: Diagnosis and therapy: Diagnosis and therapy. Obstetrics and Gynecology, 136(5), 1047–1058.
- Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiologic Reviews, 36(1), 104–113.
- Ylikorkala, O., & Dawood, M. Y. (1978). New concepts in dysmenorrhea. American Journal of Obstetrics and Gynecology, 130(7), 833–847.
- Oladosu, F. A., Tu, F. F., & Hellman, K. M. (2018). Nonsteroidal antiinflammatory drug resistance in dysmenorrhea: epidemiology, causes, and treatment. American Journal of Obstetrics and Gynecology, 218(4), 390–400.
- Falcone, T., & Flyckt, R. (2018). Clinical management of endometriosis. Obstetrics and Gynecology, 131(3), 557–571.
- Wilson, M. L., & Murphy, P. A. (2001). Herbal and dietary therapies for primary and secondary dysmenorrhoea. Nursing Times, 97(36), 44.
- Shetty, G. B., Shetty, B., & Mooventhan, A. (2018). Efficacy of acupuncture in the management of primary dysmenorrhea: A randomized controlled trial. Journal of Acupuncture and Meridian Studies, 11(4), 153–158.
- Ziaei, S., Zakeri, M., & Kazemnejad, A. (2005). A randomised controlled trial of vitamin E in the treatment of primary dysmenorrhoea. BJOG: An International Journal of Obstetrics and Gynaecology, 112(4), 466–469.
- Wong, C. L., Farquhar, C., Roberts, H., & Proctor, M. (2009). Oral contraceptive pill as treatment for primary dysmenorrhoea. Cochrane Database Syst Rev.
- Kannan, P., & Claydon, L. S. (2014). Some physiotherapy treatments may relieve menstrual pain in women with primary dysmenorrhea: a systematic review. Journal of Physiotherapy, 60(1), 13–21.
- Grandi, G., Ferrari, S., Xholli, A., Cannoletta, M., Palma, F., Romani, C., Volpe, A., & Cagnacci, A. (2012). Prevalence of menstrual pain in young women: what is dysmenorrhea? Journal of Pain Research, 5, 169–174.
- Elboim-Gabyzon, M., & Kalichman, L. (2020). Transcutaneous electrical nerve stimulation (TENS) for primary dysmenorrhea: An overview. International Journal of Women’s Health, 12, 1–10.
- Azagew, A. W., Kassie, D. G., & Walle, T. A. (2020). Prevalence of primary dysmenorrhea, its intensity, impact and associated factors among female students’ at Gondar town preparatory school, Northwest Ethiopia. BMC Women’s Health, 20(1).
- Kho, K. A., & Shields, J. K. (2020). Diagnosis and management of primary dysmenorrhea. JAMA: The Journal of the American Medical Association, 323(3), 268.
- Proctor, M. L., & Murphy, P. A. (2001). Herbal and dietary therapies for primary and secondary dysmenorrhoea. Cochrane Database of Systematic Reviews, 3, CD002124.
- Brown, J., & Brown, S. (2017). WITHDRAWN: Exercise for dysmenorrhoea. Cochrane Database of Systematic Reviews, 2, CD004142.
- Potur, D. C., Bilgin, N. C., & Komurcu, N. (2014). Prevalence of dysmenorrhea in university students in Turkey: effect on daily activities and evaluation of different pain management methods. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses, 15(4), 768–777.
- Arakawa, I., Momoeda, M., Osuga, Y., Ota, I., & Koga, K. (2018). Cost-effectiveness of the recommended medical intervention for the treatment of dysmenorrhea and endometriosis in Japan. Cost Effectiveness and Resource Allocation, 16(1).
- Organization, W. H. (2000). The Asia-Pacific perspective: Redefining obesity and its treatment.
- Ortiz, M. I. (2010). Primary dysmenorrhea among Mexican university students: prevalence, impact and treatment. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 152(1), 73–77.


 Neha Rani* 1
Neha Rani* 1
 Madhvi Ghadge 2
Madhvi Ghadge 2
 10.5281/zenodo.11263852
10.5281/zenodo.11263852