Abstract
The study mainly aims to assess the risk factors, clinical profile and prevalence in pancreatitis patients. The key objectives of the study include to assess the risk factors of pancreatitis patients, to identify the clinical profile and prevalence in pancreatic patients, the main objective of this present study is to assess the safety and give the information about the risk of various severity indices in predicting the outcome of the patients. It is a prospective observational study which was conducted in Government General Hospital Kurnool district in the department of general medicine. The present study was conducted to study the risk factors, clinical profile and prevalence of the pancreatitis patients In the current study, the sample size was 70 patients most of them were females constituting 76.3%. Majority of patients was suffering with pancreatitis from the age 21-40 years. Most common risk factors for were found to be Hypertension (30%), Diabetes (24%), HTN and T2DM (22%) followed by alcohol consumption (55.8%), gall stones (7.35%) .The clinical profile majorly observed in pancreatitis patients are abdominal pain , (98.5%), vomiting (67.6%), fever (17.6%), constipation (11.7%),jaundice(1.47%), bloating (23.5%).In this study minor complications like Headache was treated with paracetamol, followed by vomiting’s with ondansetron, infections with antibiotics like meropenem, ceftriaxone and amoxiclav and the least abdominal pain treated with tramadol. The present study concluded that the common risk factors are alcohol consumption and gall stones and mostly males are affected by the pancreatitis than the females and the most common symptoms are jaundice, vomiting, abdominal pain. Gender wise incidence of pancreatitis was more in males when compared to females due to the increased alcoholic consumption. Majority of patients were having mild disease and responding to conservative management. Complications are dealt with minimally invasive methods like image guided PCD and escalated to surgery when not relieved. There is no mortality in our study.
Keywords
Pancreatitis, clinical features, prevalence, risk factors, treatment.
Introduction
Pancreatitis is inflammation of the pancreas. The pancreas is a large gland behind the stomach, close to the first part of the small intestine, called the duodenum. The pancreas has two main functions—to make insulin and to make digestive juices, or enzymes, to help you digest food. These enzymes digest food in the intestine. Pancreatitis occurs when the enzymes damage the pancreas, which causes inflammation. Pancreatitis can be acute or chronic. Either form is serious and can lead to complications.
Acute pancreatitis
Acute pancreatitis occurs suddenly and is a short-term condition. Most people with acute pancreatitis get better, and it goes away in several days with treatment. Some people can have a more severe form of acute pancreatitis, which requires a lengthy hospital stay.
Chronic pancreatitis
Chronic pancreatitis is a long-lasting condition. The pancreas does not heal or improve. Instead, it gets worse over time, which can lead to lasting damage to your pancreas.
Etiology:
Alcohol use is one of the most frequent causes of acute pancreatitis, since it affects almost half of all cases. What's left are mostly cases of gallstones. Rarely, pancreatitis may result from injuries or surgeries to the pancreatic region hereditary abnormalities of the pancreas hereditary metabolic disorders.
- 80% of the cases are due to gall stones and alcohol
- The remaining 20% are due to:
- Congenital: pancreatic divisum
- Metabolic: Hyperlipidemia, hypercalcemia,
- Toxic: scorpion venom
- Infective: Mumps, coxsackie B, EBV, CMV
- Drugs: azathioprine, sulfonamide, steroids, thiazides, estrogens.1
Pathophysiology Of Acute Pancreatitis:
The pathophysiology of pancreatitis in the pancreas and systemic inflammatory response is characterized by the localized damage. Premature activation of trypsinogen to trypsin within the acinar cell rather than the duct lumen is the main initiating event. The main causes include issues with pH and calcium balance, as well as elevated ductal pressures (due to duct obstruction). Numerous toxins that induce pancreatitis deplete ATP, which raises intra-acinar calcium concentrations and may promote the early activation of trypsinogen to trypsin, activating enzymes such phospholipases and elastases. Damage Associated Molecular Patterns (DAMPs) are released and severe tissue damage is caused by this early activation of these zymogens. The inflammatory cascade and neutrophil recruitment are linked to this DAMP release. The systemic symptoms of acute pancreatitis are subsequently brought on by this inflammatory cascade. In the end, it results in microvascular thrombosis, capillary permeability, and endothelial destruction, which leads to multi-organ dysfunction syndrome (MODS), the primary cause of morbidity and mortality in the context of acute pancreatitis.A hereditary susceptibility to pancreatitis also affects some people, who experience repeated acute pancreatitis that eventually develops into chronic pancreatitis. It should come as no surprise that the linked genes are involved in the conversion of trypsinogen to trypsin. Recurrent pancreatitis is associated with mutations in several genes, including the CFTR gene, the gain of function mutations in the cationic trypsinogen gene (PRSS1), the trypsin degrading enzyme (CTCR), chymotrypsin C, and the pancreatic secretory trypsin inhibitor (SPINK1). Moreover, they are implicated in the growing range of illnesses, encompassing both acute and chronic pancreatitis.
Clinical Manifestations :
Symptoms :
Symptoms of acute pancreatitis could include:
- Upper abdominal pain.
- radiating pain from high abdomen to back.
- tenderness in the abdomen when touched.
- High temperature.
- quick heartbeat. Upset stomach. throwing up.
- Severe abdominal pain and pain located in the upper quadrant and mid epigastric. Nausea, vomiting, hypotension, anorexia , fever , weakness2
Treatment:
Treatment for acute or chronic pancreatitis may include:
-a hospital stay to treat dehydration with intravenous (IV) fluids and, if you can swallow them, fluids by mouth
-pain medicine, and antibiotics by mouth or through an IV if you have an infection in your pancreas
-a low-fat diet, or nutrition by feeding tube or IV if you can’t eat
Acute Pancreatitis
Mild acute pancreatitis usually goes away in a few days with rest and treatment. If your pancreatitis is more severe, your treatment may also include: Surgery. Your doctor may recommend surgery to remove the gallbladder, called cholecystectomy, if gallstones cause your pancreatitis. Having surgery within a few days after you are admitted to the hospital lowers the chance of complications. If you have severe pancreatitis, your doctor may advise delaying surgery to first treat complications. Procedures. Your doctor or specialist will drain fluid in your abdomen if you have an abscess or infected pseudocyst, or a large pseudocyst causing pain or bleeding. Endoscopic Cholangiopancreatography (ERCP). Doctors use ERCP to treat both acute and chronic pancreatitis. ERCP combines upper gastrointestinal endoscopy and x-rays to treat narrowing or blockage of a bile or pancreatic duct.
Chronic pancreatitis
Treatment for chronic pancreatitis may help relieve pain, improve how well the pancreas works, and manage complications.
Your doctor may prescribe or provide the following: Medicines and vitamins. Your doctor may give you enzyme pills to help with digestion, or vitamins A, D, E, and K if you have malabsorption. He or she may also give you vitamin B-12 shots if you need them. Surgery. Your doctor may recommend surgery to relieve pressure or blockage in your pancreatic duct, or to remove a damaged or infected part of your pancreas. Surgery is done in a hospital, where you may have to stay a few days. In patients who do not get better with other treatments, surgeons may perform surgery to remove your whole pancreas, followed by islet auto-transplantation. Islets are groups of cells in your pancreas that make hormones, including insulin. After removing your pancreas, doctors will take islets from your pancreas and transplant them into your liver. The islets will begin to make hormones and release them into your bloodstream. 3
METHODOLOGY:
This study is a prospective observational study and the subject involved are the in patient general medicine department of government general hospital Kurnool.
-
- Study design: prospective observational study
- Study site: general medicine department, GGH ,Kurnool.
- Sample size:70 cases
- Study material: patient data collection proforma .
Inclusion criteria:
- Patients newly diagnosed with Pancreatitis.
- Patients of age >20 years are included in this study.
- Either gender is considered.
Exclusion criteria:
- Patients did not sign to consent form are excluded from the study
- Patients are excluded who age is below 20 years.
- Patients who does not have the Pancreatic risk factors can be excluded. Patients are excluded who having pancreatitis but it's idiopathic
RESULTS:
Distribution of patient based on acute pancreatitis in the total study population
Table. 5.1 Types of Pancreatitis:
|
S. N0
|
Types
|
Total
|
Percentage
|
|
1
|
Acute pancreatitis
|
45
|
64.20%
|
|
2
|
Chronic pancreatitis
|
25
|
35.71%
|
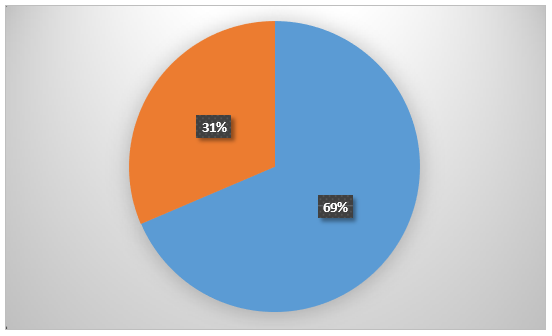
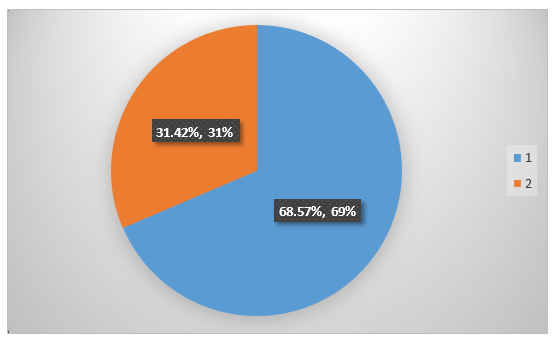
Figure :5.1 Types of pancreatitis
A total 70 patients out of them 45 males(12%) and 12 females(17%) are suffering with Acute Pancreatitis .
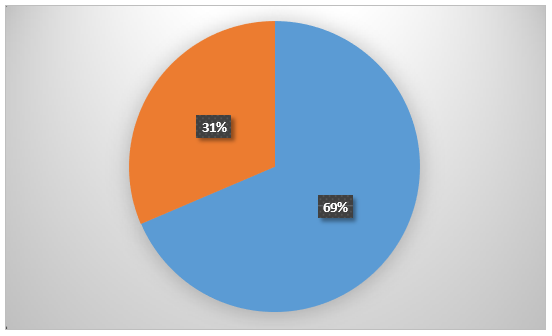
Gender Wise Distribution Of Total Study Population: The Study involved total 70 Patients out of them 48(68.57%) are Males and 22(31.42%) are Females
Table.5.2 Gender wise distribution of total study population
|
S. No
|
Gender
|
Numbers
|
Percentage
|
|
1
|
Males
|
48
|
68.57%
|
|
2
|
Females
|
22
|
31.42%
|
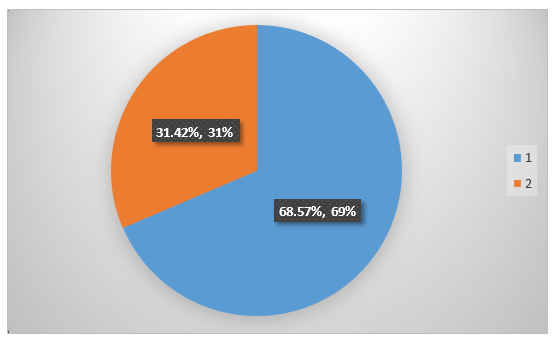
FIG:5.2 Distribution of males and females on total study population
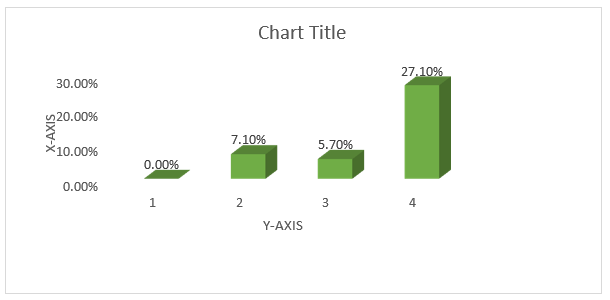
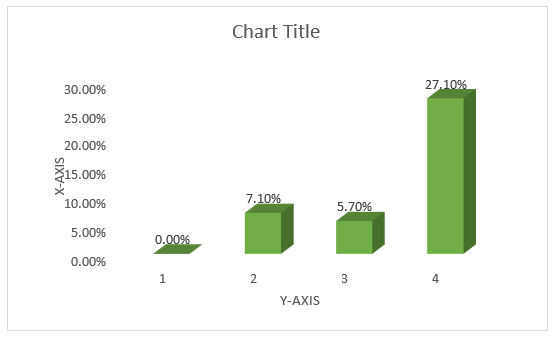
Age Distribution of Total Study:
A total of 70 patients were enrolled in general medicine department at which the age the age group of >20(11.4%), followed by 21-40 years (42.8%), followed by 41-60 years (34.2%) followed by >60 years (11.4%).
Table :5.3 Distribution of age on total study population
|
S. No
|
Age Group (Years)
|
No Of Patients
Male Female
|
Total (%)
|
|
1
|
>20
|
5
|
3
|
8(11.4%)
|
|
2
|
21-40
|
24
|
6
|
30(42.8%)
|
|
3
|
41-60
|
19
|
5
|
24(34.2%)
|
|
4
|
>60
|
4
|
4
|
8(11.4%)
|
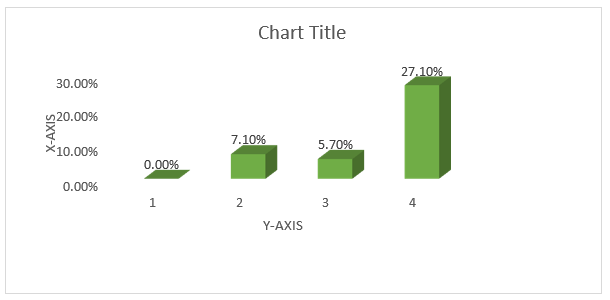
Fig :5.3 Distribtion of Age on Total Study Population
Occupation distribution of the total study population A total of 70 Patients were enrolled in general medicine department in which out of them 25 males and 10 females are farmers, followed by 20 males and 3 females are cooly, followed by 5 males and 2 females are skilled workers, followed by 2 males and 4 females are un employed.
Table:5.4 Distribution of occupation on total study population
|
Occupation
|
Males
|
Females
|
Percentage
|
|
Farmer
|
25
|
10
|
50%
|
|
Cooly
|
20
|
3
|
32.8%
|
|
Skilled Work
|
5
|
2
|
10%
|
|
Un Employed
|
2
|
4
|
8.5%
|
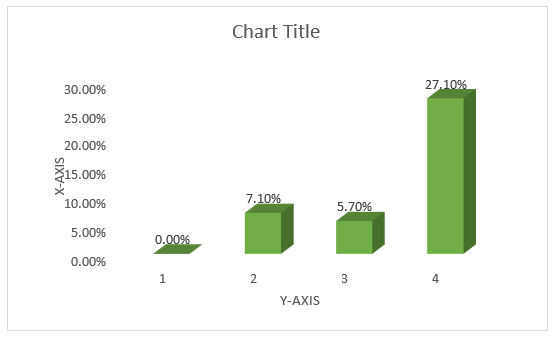
FIG:5.4 Distribution of occupation on total study population
Social Habits distribution of total study population
A total of 70 patients out of 28 males and 6 females are alcohol consumption (48.5%), followed by 10 males and 0 females are smokers (14.28%) followed by 7 are male and 16 are females were eating the junk food (32.85%).
Table:5.5 Distribution of social habits on total study population
|
Social Habits
|
Males
|
Females
|
Percentage
|
|
Alcohol Consumption
|
28
|
6
|
48.5%
|
|
Smoking
|
10
|
0
|
14.28%
|
|
Junk food
|
7
|
16
|
32.85%
|
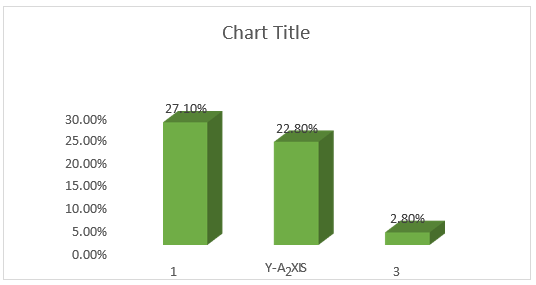
Figure :5.5 Distribution of social habits on total study population
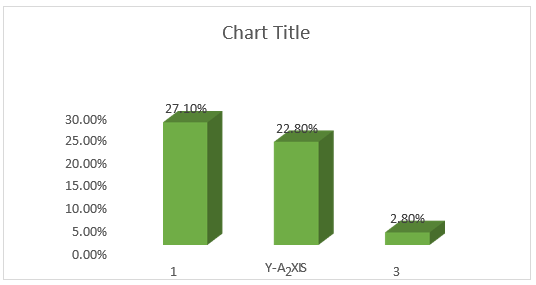
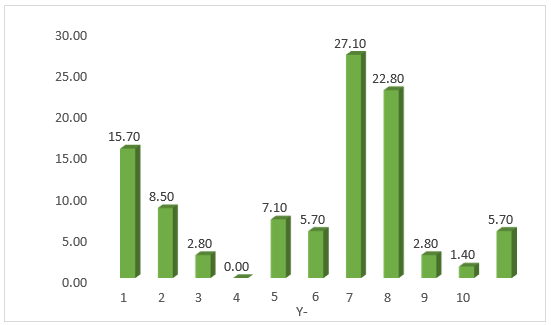
Risk Factors analysis of the total study population
A total 120 patient out of them 8 males and 6 females are diabetic (20%) ,2 males and 4 females has abdominal injuries (8%) , 1 male and 1 female has hypertriglyceridemia (2%) , 15 males and 1 female are alcoholic (22%) , 1 men
and 1 female are traumatic (10%) , 5 males and 1 female has obesity (8%).
Table.5.6 Distribution of risk factors on total study population:
|
Risk Factors
|
Males
|
Females
|
Total
|
Percentage
|
|
Diabetes
|
5
|
6
|
11
|
15.7%
|
|
Abdominal Injuries
|
2
|
3
|
6
|
8.5%
|
|
Hypertriglyceridemia
|
1
|
1
|
2
|
2.8%
|
|
Cystic Fibrosis
|
0
|
0
|
0
|
0%
|
|
Infections
|
2
|
3
|
5
|
7.1%
|
|
Hypercalcemia
|
3
|
1
|
4
|
5.7%
|
|
Gall Stones
|
9
|
10
|
19
|
27.1%
|
|
Alcohol Consumption
|
13
|
3
|
16
|
22.8%
|
|
Traumatic
|
1
|
1
|
2
|
2.8%
|
|
Choledocholithiasis
|
1
|
0
|
1
|
1.4%
|
|
Obesity
|
3
|
1
|
4
|
5.7%
|
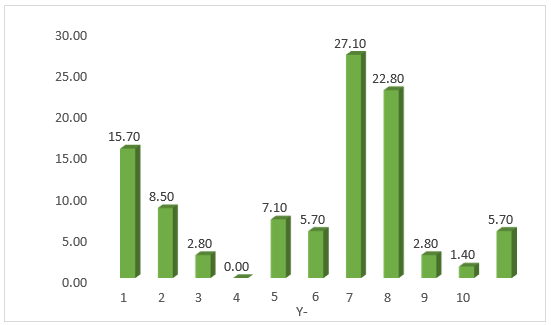
Figure :5.6 Distribution of risk factors on total study population
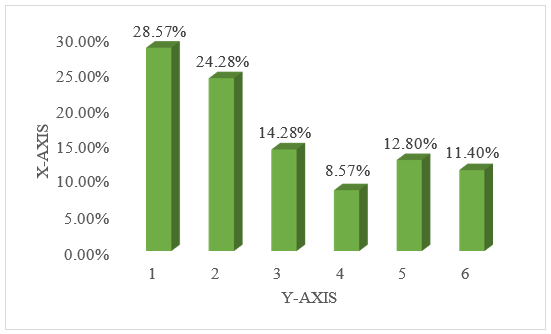
Clinical manifestation of the total study population
A total of 70 patients out of 20(28.57%) are abdominal pain, followed by vomiting17(24.28%), fever (14.28%), and followed by constipation (8.57%), jaundice (12.8%), bloating (11.4%).
Table.5.7 Clinical manifestation of the total study population
|
Characteristics
|
No of cases
|
Percentage (%)
|
|
Abdominal pain
|
20
|
28.57%
|
|
Vomiting
|
17
|
24.28%
|
|
Fever
|
10
|
14.28%
|
|
Constipation
|
6
|
8.57%
|
|
Jaundice
|
9
|
12.8%
|
|
Bloating
|
8
|
11.4%
|
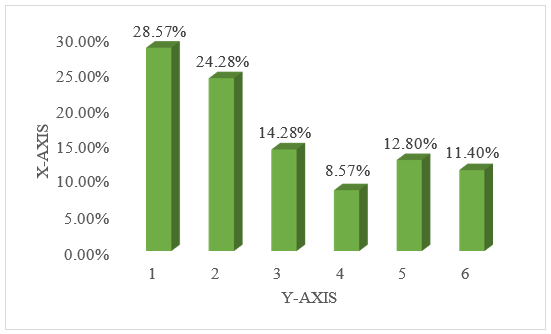
Figure: 5.7 Clinical manifestation of the total study population
DISCUSSION:
In our Study, the preponderance of male patients over the female patients was the comparable study done by devi MB and Swaroopa et al,4 at which male preponderance is greater. various epidemiological Studies in pancreatitis are able to explain the differences in gender distribution in their respective Studies. In our present study the gender distribution shows the both males and females are affected with pancreatitis with variable frequency. In our study 68.57% patients affected by pancreatitis were found to be male and 31.42% were female. Similar to the study of Manohar Lal prasad et al.5, found that pancreatitis affecting 73.9% patients was male and 26.1?male is seen. Distribution of age among the total study population shows the majority of patients were in the age group of 21 -40 years with 30(42.8%) followed by 34.2% patients in the age group of 41-60 years. this may be higher alcohol consumption among older and middle-aged males and compared with the age of female patients. This is comparable to the studies by M. Bhargavi devi et al.,4 of the patients were aged 31 -40 years 46 (32.8%) were aged 21-30 years (17.1%) were aged between 41- 50 years 2.14 %in years. In our study the occupation was distributed of farmers 50%, cooly 23% and skilled workers 7% and in this the farmers shows the majorly affected with the pancreatitis . similar study like Manjunatha Goud and Bhavan Nayal7 can show the 53% of farmers were affected with pancreatitis due to farmers were exposed to at least one or other type of toxicity every day. It causes the respiratory distress like bronchospasm and bronchial secretions and causes the sub clinical symptoms of pancreatitis In present study the identify the most common affected factor is alcohol consumption 48.5% and followed by junk food 32.85%. most of the alcohol consumption patients were affected with the pancreatitis. In this study the most commonly studied risk factors are alcohol consumption 22.8 % and gall stones 29.7%, followed by diabetes 20 % and here the majorly alcohol consumption patients and gall stones patients affected by the pancreatitis. In a similar study by Dibyendu Mukherjee et. al., risk factors was alcohol consumption 69% and gall stones in 29.4 % of patients followed by hypertriglyceridemia 8.9%. In our study we found the abdominal pain was the most common presenting symptom in most of the patients, i.e. 28.57%. a poorly functioning pancreas causes digestive problems, which eventually leads to increased vomiting, which is a common clinical symptom in 24.28%, fever in 14.28%, constipation in 8.57% and jaundice in 12.8%. this comparable study done by Surajit Kumar Das et al.9 where abdominal pain was seen in 100 patients followed by vomiting in 85?ver in 14%. In our study the distribution between the both tables of acute pancreatitis and chronic pancreatitis, the majorly affected by acute pancreatitis i.e. 68.20% and chronic pancreatitis is 35.71%.in acute pancreatitis gall stones are formed and may causes inflammation in the pancreatic duct. And the chronic pancreatitis can mostly in severe condition like heavy alcoholic consumption. In similar studies like Hamza Ashraf11 and John Paul Colombo10 with the acute pancreatitis 25% and chronic pancreatitis 14%.
CONCLUSION:
- The present study concluded that the common risk factors are alcohol consumption and gall stones and mostly males are affected by the pancreatitis than the females and the most common symptoms are jaundice, vomiting, abdominal pain.
- Abdominal pain is the most common clinical characteristics of pancreatitis. The most common risk factor seems to be alcohol consumption.
- Gender wise incidence of pancreatitis was more in males when compared to females due to the increased alcoholic consumption.
- Majority of patients were having mild disease and responding to conservative management. Complications are dealt with minimally invasive methods like image guided PCD and escalated to surgery when not relieved. There is no mortality in our study.
REFERENCES
- National Institute of Diabetes and Digestive and Kidney Diseases. Definition & Facts for Pancreatitis | NIDDK [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. 2019. Available from: https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/definition-facts
- RSNA A. Pancreatitis [Internet]. Radiologyinfo.org. 2024 [cited 2025 Feb 4].Available from: https://www.radiologyinfo.org/en/info/pancreatitis#904384c39fd44388a0c5e1b61f2db803
- National Institute of Diabetes and Digestive and Kidney Diseases. Treatment for Pancreatitis | NIDDK [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. 2019. Available from: https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/treatment
- Dr . M . Bhargavi Devi , Dr .G . Sampoorna , Dr . P . Padmalatha (2016) to study the clinical presentation , etiological factors ,outcome of patients in a acute pancreatitis in a tertiary care hospital at Guntur #http//www.myoclinic.com
- Manohar Lal prasad, Prajit Mazumdar, (2015) is a cross sectional descriptive study of prevalence, clinical profile and etiological profile of pancreatitis in single center study #http//www.myoclinic.com.
- Abhishek Mathew S, Ashwini Reddy ,Dinesh Naik (2014) conducted a prospective observational study
- Manjunath Goud, Bhavan Nayal ,K Deepa (2013) conducted a study on acute pancreatitis with occupational exposure to organophosphorusc compounds//www.organophosparous compound.com.
- Singh VK, Bollen TL, Wu BU, et al (2012) Conducted a study on Factors Associated with severe disease among patients in acute Pancreatitis.feb25;29(1)26
- Peery AF, Crockett SD, Barritt AS, Dellon ES, Eluri S, Gangarosa LM, et al (2011) conducted a study on Gastrointestinal, Liver, and Pancreatic Diseases in the United States.//www.ncbi.nlm.nih.gov/pmc/articles
- Banks PA, Bollen TL, Dervenis C, et al. (2005) Conducted a study on Atlanta classification of acute Pancreatitis enabled standardising reporting of research aided communication between clinicians. Deficiencies identified and improved understanding of the disease make a revision necessary//www.ncbi.com
- Johnson CD, Abu-Hilal M. (2004) conducted a study on persistent organ failure during the first week as a marker of fatal outcome in acute Pancreatitis
- Howard TJ, Patel JB, Zyromski N, et al. (2002) conducted a study on declining morbidity and mortality rates in surgical management of pancreatitis necrosis//www.ncbi.com
- Lankisch PG, Weber-Dany B, Maisonneuve P, Lowenfels AB (2001) Conducted a study on High serum creatinine in acute Pancreatitis http//www.pulus.com/scholarly-articles/pancreatiticdisease.


 M. Spurthy Mitra*
M. Spurthy Mitra*
 C. Mahaboob Desai
C. Mahaboob Desai
 K. Meghana Rani
K. Meghana Rani
 10.5281/zenodo.14868821
10.5281/zenodo.14868821