Abstract
Alzheimer's disease is a neuro-degenerative disorder & the most prevalent form of mental illness, resulting in the forward-looking impairment of memory & behavioral functions, including memory, language, attention, thinking, & the ability to multitask. It ranks as the sixth leading cause of mortality globally. Owing to its intricate etiopathology, existing pharmacological treatments have not succeeded in completely curing the disease. Consequently, natural compounds are being explored as alternative therapeutic options for Alzheimer’s disease. Traditional herbs & formulations from the Indian Ayurvedic system, which are abundant in antioxidants, and anti-amyloidogenic, neuroprotective, & anti-inflammatory properties, have demonstrated the potential to enhance the standard of living by improving cognitive memory & revitalizing brain function by means of neurogenesis. Multiple risk factors contribute to the development of the disease, including advancing age, infections, genetic predispositions, vascular conditions, & environmental influences. Contemporary research is focused on elucidating the pathology of Alzheimer's disease by targeting multiple mechanisms, such as aberrant tau-protein metabolism, Beta-amyloid accumulation, inflammatory reactions, cholinergic dysfunction, & oxidative stress, to grow efficacious treatments able to halt or make changes to the progression of the disease. This review elucidates the risk factors and novel pathophysiological pathways implicated in Alzheimer's disease & underscores the neuroprotective effects of medicinal plants in combating the disorder.
Keywords
Neuro-deterioration, Demise, Cognitive, Anti-amyloidogenic, Neuroprotective
Introduction
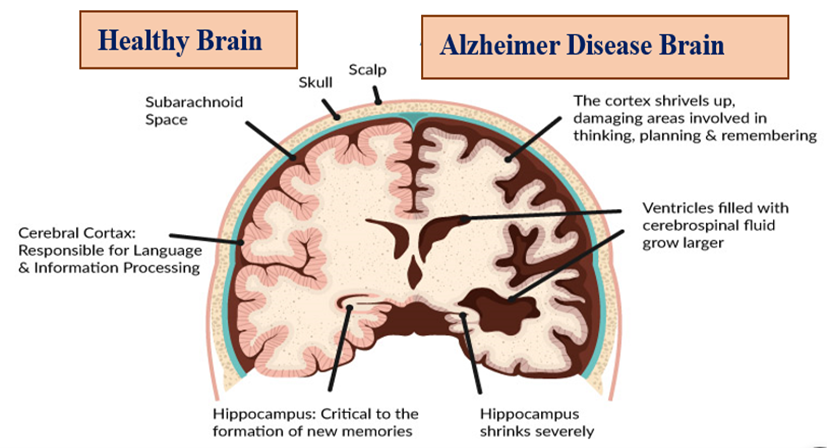
The word "dementia" describes a broad range of memory impairments that significantly impair daily functioning. With Alzheimer’s disease accounting for two-thirds of the instances or more among those 65 years of age & older, it is the most common type of dementia. While Alzheimer's disease itself is not directly fatal, it significantly increases susceptibility to other complications that can eventually lead to death. Alzheimer's disease, pronounced "alz-HAI-mirs," is a brain condition that progressively undermines one's ability to remember, think, learn, and organize, eventually impairing the capacity to perform essential daily tasks. It is responsible for 50% to 75% of instances of dementia, rendering it the most prevalent kind of dementia. The disease damages neurons and brain cells, disrupting the brain's neurotransmitters, particularly those responsible for memory storage. As the most prevalent neurodegenerative disease-causing dementia, Alzheimer's accounts for 60%-80% of cases. The hippocampus and temporal lobes, crucial for storing and retrieving new information, begin to atrophy as gaps appear in the brain. This leads to a decline in individuals' abilities to recall information, speak, think, and make decisions. Additionally, the disease affects the brain's capacity to produce specific neurotransmitters, such as acetylcholine.[1] As the most prevalent form of dementia, Alzheimer's disease is named after the German physician Alois Alzheimer. It's described as a neurological disease that advances gradually.[2] The first person to describe a debilitating ailment that would later be known as Alzheimer’s disease was first introduced by Alois Alzheimer, a psychiatrist of German and expert in neuropathology. Alzheimer's disease is described in the patient named Auguste D., a 51-year-old lady who experienced disorientation, behavioral symptoms (such as hallucinations, paranoia, and delusions), progressive memory & language impairment, and psychosocial impairment. Alzheimer’s as an “unusual disease of the cerebral cortex” referred to the illness. The greatest danger element for the onset of Alzheimer’s disease is getting older.[3] The most popular kind of dementia worldwide and the second most important reason for mortality is Alzheimer’s disease, a neurodeterioration condition. It is still unknown, nevertheless, exactly what causes Alzheimer’s disease. The hypothesis of cholinergic neurons, the amyloid-beta hypothesis, the tau protein hypothesis, & the neuroinflammation hypothesis are currently accepted theories. Finding new, promising treatments and effective medications for Alzheimer's disease is a popular topic globally because there are now relatively few effective medications and treatments available.[4] The onset & progression of Alzheimer’s disease pathology are also influenced by additional variables such as oxidative stress, inflammatory cascades, and anomalies in cholinergic neurons. A multitude of cellular dysfunctions are known to be caused by oxidative stress, which disrupts the biomolecules' cellular metabolic system, including proteins, lipids, and nucleic acids. Major brain damage or even death are the disease's eventual outcomes, which frequently start as mild symptoms. All cases of Alzheimer’s disease occur in the premature stage, which occurs between the ages of sixty and sixty-five and accounts for 1% to 6% of cases. Of these cases, 60% are familial, and 13% seem to be inherited in an autosomal dominant fashion. The variations in familial Alzheimer's disease with premature stages. An autosomal dominant disorder associated with mutations in three genes is another way that Alzheimer's disease might be inherited: genes for the amyloid precursor protein on chromosome 21, chromosomes 14 & 1 for presenilin1 & 2, respectively. Mutations in presenilin 1 & presenilin 2 prevent gamma-secretase from executing, This eventually results in the accumulation of beta-amyloid. Around 5% to 10% of all cases are because mutations mostly in these three genes account for the majority of cases of early-onset Alzheimer's disease.[5] Alzheimer’s disease symptoms are lessened by current pharmaceutical therapies, but the illness's primary pathological features remain unaltered. As a result, creating novel and effective treatments is crucial. Alzheimer's disease has several possible therapies. Research is being done on new therapy strategies, including ones that are more directly aimed at the disease's pathophysiology. Anti-inflammatory medications, cholesterol-lowering medications, secretase inhibitors, metal chelators, and the amyloid-beta-peptide vaccine are some of these possible disease-modifying therapies. Currently being researched are several prospective treatments, such as antioxidants and free radical scavengers, monoamine oxidase-B inhibitors, estrogen replacement, and anti-inflammatory drugs.[6]
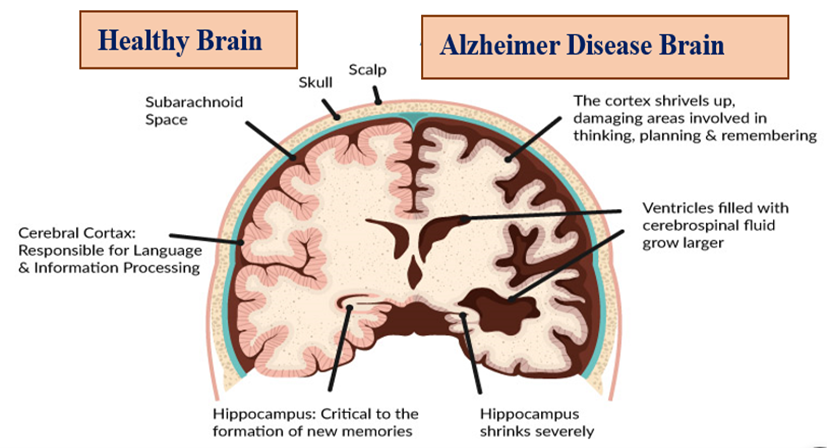
Figure 1: Showing a difference between a Healthy and Alzheimer’s disease brain
Over the past ten years, noteworthy advancement has been achieved in the development of indications of the early & specific identification of Alzheimer's illness. These biomarkers include phospho-tau, amyloid, & tau levels found in plasma, cerebrospinal fluid, and neuroimaging markers acquired from positron emission tomography scans. [7] The manner in which memory impairments & Alzheimer’s disease are greatly aided by medicinal plants. Through phytochemical research, several substances with pharmacological activity, such as anti-cholinesterase and anti-amyloidogenic properties, have been found. These chemicals include alkaloids, sterols, polyphenols, tannins, triterpenes, flavonoids, & lignins. The manner in which memory impairments & Alzheimer’s disease are greatly improved by medicinal plants. The oldest known cures are natural items and herbal medications. The demand for herbal goods is rising rapidly worldwide in the current environment. Memory deficit is a serious worldwide health issue. We have read the research on the usage of medicinal herbs to cure memory loss and Alzheimer's disease. [8] For many years, various civilizations have utilized medicinal plants like Punica granatum Linn, Salvia officinalis, Valeriana officinalis, Myristica fragrans, Bacopa monnieri Linn, Centella asiatica Linn, & Evolvulus alsinoides Linn to enhance memory. Herbal medicines are useful in treating Alzheimer's disease because of their general anti-inflammatory & antioxidant properties as well as their unique cholinesterase inhibitory impact. Due to claims about their efficacy, safety, and affordability, herbal drugs are also growing in popularity. [9]
Prevalence:[10, 11, 12, 13]
Behavioral problems, cognitive degeneration, and a progressive decline in daily functioning are its defining characteristics. Pre-senile and senile dementia are most commonly associated with this type. Per WHO estimates, the global prevalence of Alzheimer 's type dementia is 6% in women and 5% in men over 60. Vascular dementia makes up over 39% of dementia cases in India, where the general frequency is 33.6% per 1000 people. This represents nearly 54% of all dementia cases. The number of persons having dementia globally was projected to be 44 million in 2013, and a surge is anticipated dramatically to 136 million up till 2050. Alzheimer's disease incidence is somewhat greater in women, particularly after 85 years of age. Between 2000 and 2019, the quantity of reported Alzheimer's disease-related deaths increased by about 145%, whereas deaths from heart disease, stroke, and HIV/AIDS decreased. Alzheimer's disease death rates most likely worsened due to the coronavirus pandemic. In India, the occurrence of dementia in persons sixty years of age & older is estimated to be 7.4%. Approximately 8.8 million Indians who are older than sixty suffer from dementia. By 2022, Alzheimer’s disease is predicted to rank sixth as the most prevalent cause of death in the US. Every five years after 65 years of age, Alzheimer’s disease incidence rises. Following the age of 85, age-relevant incidence rates increase notably, going from less than one percent to six percent annually. Rates of prevalence increase from 10%-40% to 85 years of age after 65 years of age. The prevalence of Alzheimer’s disease is marginally more elevated in women, specifically those over the 85 years of age.
CLASSIFICATIONS OF ALZHEIMER’S DISEASE [14]
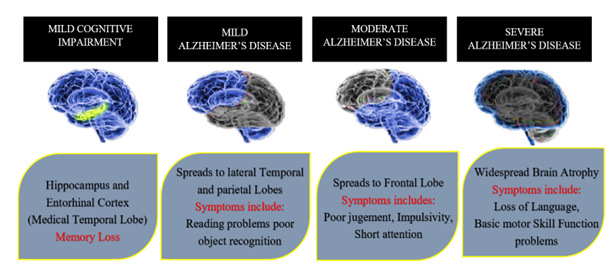
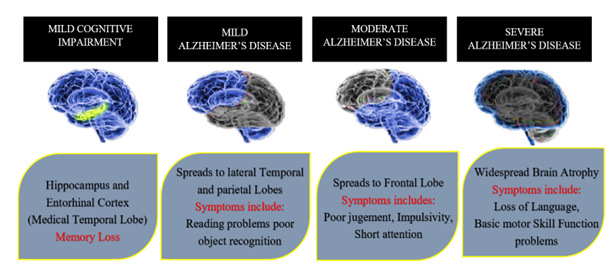
Figure 2: Alzheimer’s disease stages of spreading throughout the brain- mild cognitive impairment, mild, moderate & severe stages of Alzheimer’s disease.
- Mild cognitive impairment:
This stage is important in distinguishing b/w dementia & normal aging-related cognitive decline. It is separated into both non-amnestic and amnestic subtypes. Mild cognitive impairment is one of the most common conditions that affect the elderly and increases the risk of dementia. Because Alzheimer’s disease converts to a high rate from mild cognitive impairment, public health faces major financial issues. Therefore, it's critical to pay attention to the diagnosis & treatment of mild cognitive impairment.
- Mild Alzheimer’s disease:
This is the first phase of cognitive symptoms. This is the point at which the abnormal changes make it to the cerebral cortex. Memory loss is linked to deficits in executive functioning, judgment, and problem-solving skills, in addition to challenges remembering new knowledge and forgetting things and appointments. People also exhibit changes in their personalities, mood swings, & lack of spontaneity. Confusion & disorientation are also frequent occurrences.
- Moderate Alzheimer’s disease:
The symptoms are getting worse at this stage. The brain cortex, which controls language, thinking processes, and sensory perception, is similarly impacted by cognitive decline. Including the symptoms from the earlier phases getting worse, behavioural issues & a tendency toward social disengagement also start to show signs. The following include language challenges and deficits in visuospatial ability. It is noteworthy that people were having trouble identifying their loved ones at this point.
- Severe Alzheimer’s disease:
During this stage, patients become incapable of performing daily duties on their own. Degenerative degeneration is thought to impact all cortical areas at this time. When the diseased subject's cognitive capacities are at their lowest, other systemic symptoms manifest, such as dyspraxia (difficulty in performing or learning motor tasks), olfactory dysfunction, problems in sleeping, extrapyramidal motor indications (dystonia, akathisia), & Parkinsonian symptoms.
COMPLICATIONS ASSOCIATED WITH ALZHEIMER’S DISEASE [15]
According to the Disease Control's National Center for Health Statistics 2023, Alzheimer’s disease is the sixth most common reason for mortality, for approx. 120,000 deaths annually. People over 65 account for the bulk of cases of Alzheimer's disease, & they are also more likely to have comorbidities, which can seriously harm their health and general quality of life. As the disease worsens, Individuals suffering from Alzheimer's disease have increasing levels of loss of memory and other cognitive problems. A few instances of issues comprise wandering and becoming lost, having financial difficulties management & bill payment, posing the same queries repeatedly, taking longer than normal to complete daily duties, & also it was seen that there is changing in behavior and personality in Alzheimer’s patients. People begin to struggle to recognize friends and relatives as their disorientation and memory loss get worse. Hallucinations, an inability to pick up new skills, trouble with multistep chores like dressing, or trouble adjusting to unfamiliar situations are a few examples. Patients suffering from suffering from Alzheimer's disease are completely dependent on others for care and are unable to communicate for themselves. A wide classification of issues associated with Alzheimer's disease can be made using mental/behavioral and physical challenges.
They are stated in the following order:
Mental/Behavioural:
- Depression is one of the most prevalent comorbidities among Alzheimer's patients, which complicates the treatment of their condition. Depression-stricken individuals having Alzheimer's disease often have mood fluctuations, sleep problems, social disengagement, and difficulty focusing.
- Agitation, delirium, and sundowning are typically in the later stages of Alzheimer's disease & cause challenges for both patients & caregivers. Managing these symptoms is most important to ensuring the safety & well-being of those suffering from Alzheimer's illness. Still, there is evidence that using antipsychotic medications to improve these illnesses is associated with increased mortality rates & other adverse effects.
- Traveling This is yet another typical Alzheimer's disease effect. Because Alzheimer's disease disrupts their regular sleep patterns, people with the disease may have restlessness and insomnia. They might therefore mistakenly leave the house thinking they are going to work or on an errand. The issue is that someone you care about might leave the house and lose track of how to return. When everyone else is asleep at night, some individuals with Alzheimer's disease go wandering.
Physical: [16]
- Elderly Alzheimer's patients frequently experience fever & infections, especially urinary & respiratory infections. Aspiration pneumonia can arise from problems with swallowing, exacerbating their precarious health.
- Starvation and dehydration it's critical that the person you care about consumes adequate food and liquids. This can be challenging, though, since as the illness worsens, they might stop eating or drinking. Additionally, swallowing difficulties may prevent them from consuming food and liquids. Decreased periods of agitation & anxiety are prevalent among people with Alzheimer’s disease. A loved one's ability to reason and understand situations may also decline as the illness progresses.
- Other complications of Alzheimer’s disease disease include gastrointestinal & bladder issues. A family could become less aware of the illness as it worsens. the feeling that one must go to the restroom. They could also find it difficult to react rapidly to cravings. Limited movement or poor communication abilities may be the cause of this disease.
ALZHEIMER’S DISEASE-CAUSING RISK FACTORS
Recent years have seen a focus on the early identification & prevention of Alzheimer’s disease by experts. Obesity, diabetes, cardiovascular illness, low education, social isolation, and depression are among the major variables that increase the chance of Alzheimer's. Recent epidemiological research demonstrates that early indications of the disease are primarily displayed by other biomarkers, such as sleep, diet, and hearing loss, which are primarily responsible as risk factors for Alzheimer's disease.

Figure 3: Above image showing Alzheimer’s disease-causing risk factors
Sleep problems, such as insomnia, aberrant sleep length, poor quality sleep at night, excessive daytime sleepiness, & altered circadian patterns, are linked to a 50% to 80% a higher chance of dementia developing. A higher incidence of cognitive impairment in elderly males has also been linked to excessive daytime napping; studies have also suggested that sleep deprivation is a trigger for the amyloid-beta pathogenic characteristic of Alzheimer’s. [1]
Diet is also a risk factor for Alzheimer’s disease is eating a bad diet. Diabetes, hypertension, and obesity Reduced risk of cognitive impairment have been demonstrated by a high intake of vegetables, fruits, whole grains, nuts, & legumes; a moderate diet of fish, & alcohol; & a lower intake of red meat. Research, both preclinical and experimental, has demonstrated that dietary flavonoids and antioxidants directly impact the brain through their suppression of neuroinflammatory processes linked to Alzheimer's disease & their inhibition of pro-inflammatory cell-signaling pathways, cytokine generation, and oxidative stress. [17]
Deficits in auditory processing or modifications to the inner ear may result in hearing problems. A significant percentage of older persons (up to 40%) have hearing difficulties. Due to their detrimental effects on cognitive processing, hearing impairments may directly increase the risk of dementia by causing brain atrophy. [18]
Smoking may affect a person's susceptibility to Alzheimer’s through several different mechanisms. It is well recognized that it can enhance oxidative stress, boost pro-inflammatory activity in the immune system, and increase the production of free radicals, which will activate phagocytes and cause more oxidative damage. [19]
Some have proposed that being a widow is a significant risk of developing memory-related problems like Alzheimer's. Widowed people were more likely than married people to get Alzheimer’s disease, according to cohort research. [20]
Dementia development is in danger due to depression. Depression in early adulthood increases the probability of dementia, including Alzheimer's disease, developing afterward in life. [21]
Some have proposed that having high cholesterol increases the likelihood of getting Alzheimer's. Research has previously indicated that persons with Alzheimer's disease have cholesterol levels that are 10% greater than those of healthy individuals. Hypercholesterolemia has a connection to an elevated likelihood of causing atherosclerosis, Alzheimer’s disease, & other neurological illnesses. [22]
In common with most forms of dementia, age is the primary increased chance of Alzheimer's. Accordingly, an individual's The age-related rise in risk of Alzheimer's disease. Alzheimer’s disease doubles in risk approximately every five years in people over 65. Though those over 65 make up the majority of those affected, younger people might still have Alzheimer's. When a person has young-onset dementia, about one in three of them have Alzheimer's. [23]
Amyloid-beta plaques & neurofibrillary tangles can accumulate resulting in the occurrence of chronic infections of the central nervous system because of this, they are regarded as risk factors for Alzheimer's disease. Dr. Itzhaki's research revealed that patients with apolipoprotein E epsilon 4 allele carriers have herpes simplex virus DNA, which explains their increased risk of Alzheimer's disease. Herpes simplex virus1 can proliferate inside the brain, which can cause inflammation and an increase in amyloid-beta deposition, which can harm neurons & cause Alzheimer's disease to proceed progressively. [24]
The most reliable indicators of Alzheimer's disease risk are apolipoprotein E epsilon 4 allele, rare dominantly-inherited mutations in genes controlling amyloid in the brain, and a family history of dementia; nevertheless, these variables remain inadequately comprehended. The primary cause of Alzheimer's disease risk is getting older. An individual's danger of developing Alzheimer's disease rises by 10%-30% if they possess a first-class relative with dementia. In comparison to the general population, the risk of Alzheimer’s disease increases threefold when two or more siblings have the condition at a later stage. Apolipoprotein E is the main hereditary susceptibility factor to Alzheimer's disease with a late onset. [25]
Air pollution increases the risk of dementia, according to an increasing body of studies. The result of contaminants entering the atmosphere and altering its makeup is air pollution, which can be chemical, physical, or biological. Alzheimer's disease, cardiovascular disorders, and respiratory conditions have all been linked to it lately. [26]
-
- Cerebrovascular diseases:
Cerebral vascular abnormalities increase the chances of developing dementia, comprising hemorrhagic infarcts, minor & large ischemic cortical infarcts, vasculopathy, & alterations in cerebral white matter. Parenchymal vascular disease is found in Alzheimer's disease patients' brains according to postmortem examinations. [27]
According to research, type 2 diabetes can raise one's risk of Alzheimer's disease & dementia by 1.3 to 5.5 times. A study conducted in the 1990s in Rotterdam found that diabetes of type 2 doubled the chances of dementia & Alzheimer’s disease. Individuals suffering from type 2 diabetes have a ~60% higher risk of dementia development than people without the disease. [28]
An increasing body of research suggests that Alzheimer's disease & cardiovascular risk factors might be related to one another. The brain is especially susceptible to cerebral hypoperfusion, a condition that happens when there is inappropriate blood supply to the brain because it is highly vascularized and consumes a fifth of the oxygen supply in the body. The oxidative stress resulting from cerebral hypoperfusion is thought to be a part of the formation of tau and amyloid plaques. [24]
[29, 30] The connection between fat and Alzheimer's disease development is more in middle-aged obese people which may also increase the likelihood of developing dementia. Obesity raises the risk of vascular dementia, Alzheimer's disease, moderate cognitive impairment, & age-related cognitive decline. Obesity causes a low-grade chronic inflammation that is indicative of many other chronic disorders, including fatty liver disease, metabolic syndrome, and neuroinflammation, which is an attribute of neurodegenerative diseases like Alzheimer’s disease.
ALZHEIMER’S DISEASE-RELATED HYPOTHESIS [31]
Despite extensive research in this field, the pathophysiology of Alzheimer's illness remains unclear, and as of right now, there isn't any natural medication for the illness that can cure overall the disease state. The hippocampus and cerebral cortex are atrophying on a macroscopic level. Under a microscope, amyloid plaques, sometimes referred to as senile plaques are amorphous structures made of A-beta. The build-up of hyper-phosphorylated Tau-protein implies the formation of fibrillary tangles in the brain & significant neuronal degeneration. Recent studies have revealed that additional mechanisms are involved in the progression of these Alzheimer’s disease-related plaques.
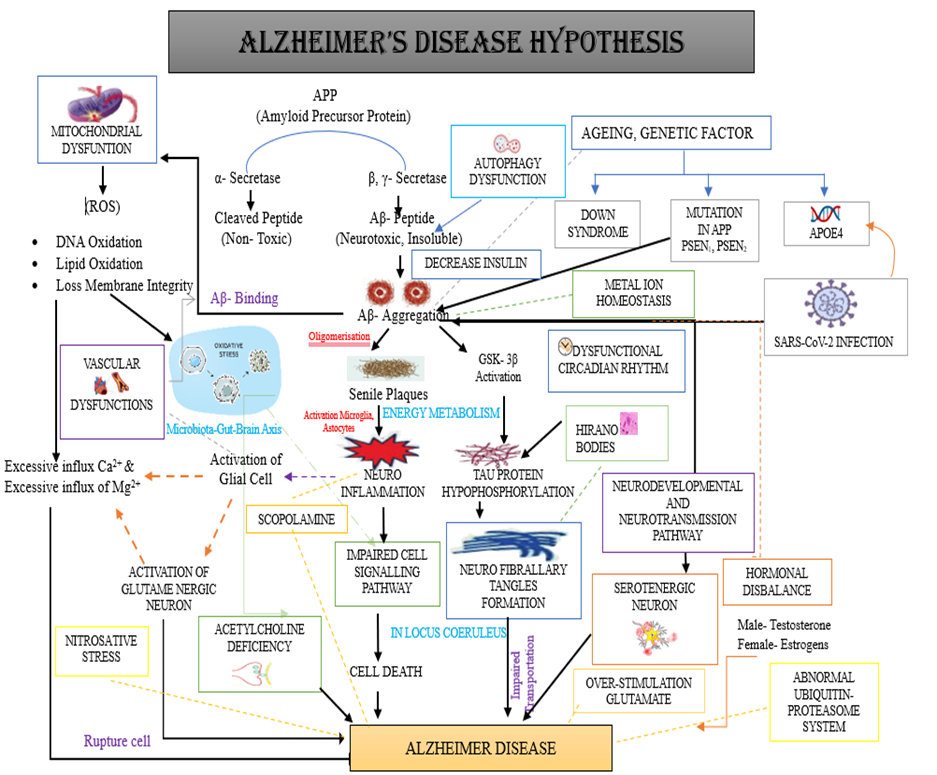
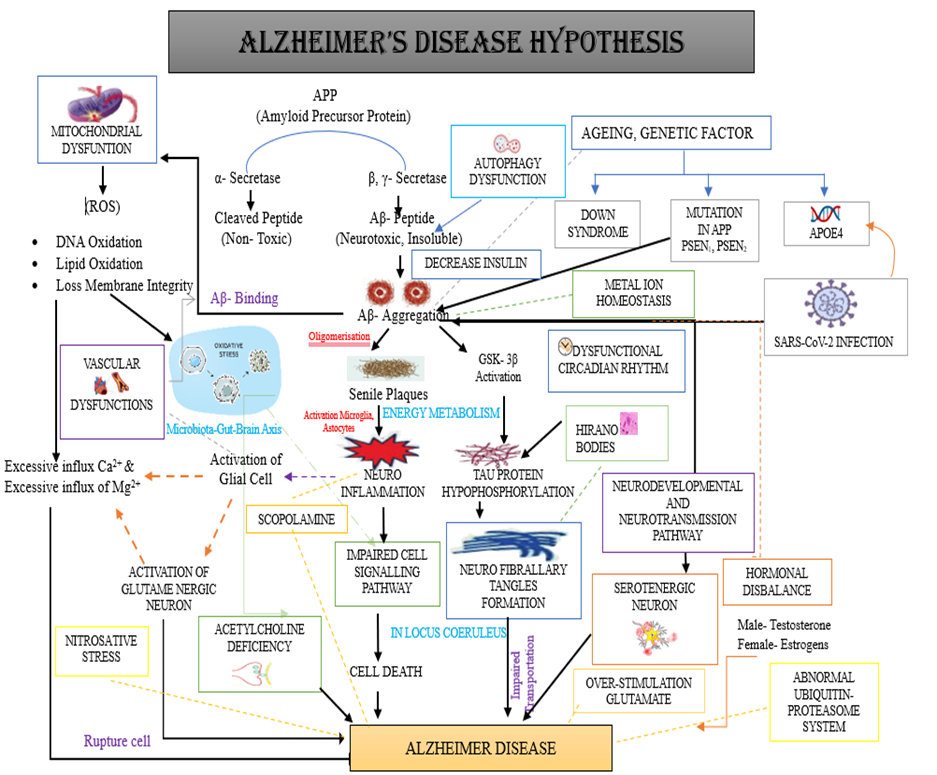
Figure 4: The figure above provides an overview of the theories related to Alzheimer's disease. It illustrates how age, genetic variables (such as Down syndrome, mutations in APP, PSEN1 & PSEN2, APOE4), mitochondrial malfunction, acetylcholine shortage, mitochondrial dysfunction in mice, oxidative stress, scopolamine, glutaminergic neuron activation, Neuro-inflammation, deficit of serotonergic neurons Circadian rhythm, nitrosative stress, locus coeruleus, and Hirano bodies neurodevelopmental and neurotransmission pathways, energy metabolism, equilibrium of metal ions, Gut-brain-microbiota axis, vascular dysfunction imbalance of hormones, anomalous proteasome-ubiquitin system, Reduce Insulin, SARS-CoV-2 outbreak, The senile plaques, also known as Amyloid Plaques, are eventually generated by autophagy dysfunction as well as the ?- & ?-secretase-mediated cleavage of APP in the normal state and alternative cleavage by ?- and ?-secretase in the diseased state. Tau protein hyperphosphorylation causes neurofibrillary tangles to develop. Each of these theories is connected to one of the other in triggering Alzheimer’s disease.
Cholinergic system Hypothesis:
The first theory relates to the etiology of Alzheimer’s illness. The basal forebrain's neurons are degenerating generally. Alzheimer’s disease causes cholinergic neurons in the entorhinal cortex and basal nucleus to disappear during the start of the disease, but by the time the illness progresses, almost 90% of the basal nucleus's cholinergic neurons have disappeared. In animal models, aberrant or compromised cholinergic system function can induce a memory deficit akin to Alzheimer's disease. This theory states that Alzheimer's patients experience both cognitive & non-cognitive symptoms as results in the death of the neurons of cholinergic in the basal forebrain & the decrease of central cholinergic transmission. [32]
Amyloid Plaque hypothesis:
The enzymes ?, ?, & ? secretase are responsible for the cleavage of amyloid precursor protein. On the other hand, the amyloid pathway's cascade is released when the amyloid precursor protein is broken down by beta-secretase, resulting in insoluble peptides with 39-43 Abeta-42 isoform fragments. These peptides have strong cytotoxic characteristics that are connected to the process of neurodegeneration, as they aid in the production of free radicals and disrupt calcium homeostasis by lipidic dysregulation of the cell membrane. Ultimately, these fragments form insoluble structures, which cause neuronal death. The normal degradation of amyloid precursor protein is not preferred by beta-amyloid 42 over the synthesis of aggregated fibrillary amyloid protein. Chromosome 21 which contains the gene encoding the amyloid precursor protein is one of the chromosomes linked to Alzheimer's disease in families. An accumulation of amyloid is observed around the meningeal, cerebral, and gray matter arteries in Alzheimer's patients. [33]
Neurofibrillary Tangles Hypothesis: [34, 35, 36]
According to this theory, the ? protein develops as a result of a secondary pathogenic event that leads to neurodegeneration. Alzheimer’s disease causes malfunctions in the ? protein's phosphorylation mechanisms, which lead to the molecule becoming hyperphosphorylated. The hyperphosphorylated protein ? exhibits abnormal cytoskeletal protein aggregation; it also interacts with microtubules at a lower grade, which promotes an increase in free tau protein. This increases tau protein's aggregation and fibrillization, which in turn causes axonal transport to malfunction. Tau protein stimulates a certain type of tubulin assembly, which results in microtubule stability. Tau protein hyperphosphorylation is the cause of neurofibrillary tangles. Research has also shown substantial evidence of the dependency between amyloid? buildup & tau-protein aggregation, which shows the last phase of the pathogenesis of the disease. High quantities of amyloid beta were found to produce Tau, which led to the process of hyperphosphorylation of Tau.
Inflammatory Hypothesis: [37, 38]
The brain's natural defense mechanism against injury, poisons, and infection is inflammation. Chronic Neuro-inflammation arises when the delicate balance b/w pro- and anti-inflammatory signals is upset. Additionally, it raises blood-brain barrier permeability and oxidative stress, which probably affects how Alzheimer's disease progresses. Inflammation and microglia activation may have a neuroprotective effect during acute events, they can also cause neurotoxicity and raise the amyloid-beta load over time. Microglia may have a protective function in response to amyloid beta, but persistent activation causes the microglia to start acting negatively, which starts a destructive cycle of degradation. Lastly, research indicates that modifying the triggering receptor expressed on myeloid cells2 (TREM2) expression, which contributes to inflammation, may affect amyloid-beta levels and plaque-associated macrophages.
Mitochondrial Dysfunction Hypothesis: [32, 39, 40]
One theory that was proposed to explain the causes and mechanisms of Alzheimer's illness was the mitochondrial cascade hypothesis. An essential source of energy for the nervous system is the mitochondria. In addition to supplying energy, mitochondria govern intracellular calcium, cellular redox, and programmed cell death/apoptosis. Numerous research studies have documented the apparent deficiency of mitochondria in Alzheimer's disease. Mitochondrial dysfunction is thought to be caused by the accumulation of pathogenic Tau protein and Abeta fragments in brain cells, which impairs mitochondrial oxidative metabolism. Numerous studies have shown that age-related decreases in mitochondrial integrity impact a variety of brain functions, including memory, learning, and sensory processing—all of which are frequently compromised in Alzheimer's disease.
Oxidative Stress Hypothesis:
A key contributing element to the etiology and development of Alzheimer’s disease is oxidative stress brought on by beta-amyloid. Oxygenative phosphorylation in the mitochondria supplies the energy required for the brain, an organ known for its high levels of energy activity. However, this process can produce excessive amounts of extremely reactive oxygen species, which can contribute to oxidative stress. When A-beta fragments build up, they encourage the reduction of brain copper and iron, two crucial components that set off oxidative stress, which in turn encourages DNA damage. This process is responsible for the accumulation of reactive oxygen species, which leaves the neurons open to an excitotoxic injury. [33]
Severe-Acute Respiratory Syndrome Coronavirus (SARS-Covid) Hypothesis:
Healthcare organizations have struggled with the COVID-19 epidemic, particularly when it comes to treating Alzheimer's patients. Due to concurrent and inflammatory disorders, age is a significant risk factor for severe strains of the coronavirus epidemic-19. Acute Respiratory Severe Syndrome Through the interaction of the spike protein with the receptor for angiotensin-converting enzyme 2, coronavirus 2 is known to infiltrate olfactory neurons and nerve terminals. The brain tissue is harmed by this contact because it sets off an inflammatory chain reaction. On the other hand, increased neuroinflammation caused by increased oxidative stress, neurodegeneration, and the isoform of apolipoprotein-E4 (APOE-4?) in Alzheimer's disease are connected. [41]
Circadian Rhythm Dysfunction Hypothesis:
Research suggests that the sleep-wake cycle and circadian rhythm may influence amyloid-beta levels. Intracerebroventricular orexin infusion raises interstitial fluid amyloid-beta levels, while dual orexin receptor antagonist almorexant reduces levels. Neuronal activity is unclear, but hippocampus orexin signaling may affect clock-controlled genes, such as beta-site amyloid precursor protein cleaving enzyme1 (Bace1) & beta-site amyloid precursor protein cleaving enzyme2 (Bace2). Dysfunctional circadian rhythm and sleep deprivation may cause abnormal tau metabolism. Numerous regions implicated in the regulation of sleep, including the locus coeruleus, dorsal raphe nucleus, periaqueductal gray matter, hypothalamic tuberomammillary nucleus, lateral hypothalamus, & basal forebrain, demonstrate a pathological trait associated with the tau. Transgenic animal research indicates that tau pathology alone may cause sleep disturbance linked to neurodegeneration. [42]
Serotonin Hypothesis: [43, 44]
Serotonin is crucial for learning and memory preservation during aging, and imbalances in serotonergic signaling and metabolism have been linked to various central nervous system disorders like anxiety, depression, schizophrenia, and Alzheimer's disease. Research shows a correlation b/w Alzheimer's disease & a reduction in serotonergic neurons in the raphe nuclei. Post-mortem brains show lower levels of serotonin and its metabolites, indicating a decrease in serotonergic neurons. The shrinkage of serotonergic neurons in Alzheimer's patients is unclear, but studies focus on potential interactions between the amyloid-mediated portion of pathology & the serotonergic system. Experimental evidence shows that selective serotonin reuptake inhibitors decrease the development of harmful amyloid-proteins & plaques in mice models of Alzheimer’s disease. Throughout the cortex and hippocampus, many Patients with Alzheimer's disease exhibit severe absence of 5-HTRs, mainly 5-HT1A and 5-HT2AR. Among the 5-HT receptors, 5-HT4Rs are distinct in that they seem to defend against amyloid beta burden and maintain cognitive function in the Alzheimer's disease early stage.
Hormonal Disbalance Hypothesis:
The most prevalent type of dementia, Alzheimer's disease, may be more likely to develop in older people due to changes in estrogen levels. Cognitive decline and neurodegenerative illnesses such as Alzheimer's are associated with hormonal changes that occur with aging. Alzheimer 's-related memory and learning problems may be more common in postmenopausal women. Gonadotropin elevations and serum sex steroid decreases are risk factors for Alzheimer's disease, indicating that estrogen can also impact the brain's utilization of chemical messengers. Through oxidative stress, inflammation, and amyloid-beta buildup, these hormones contribute to neurodegeneration. [45]
Scopolamine Hypothesis:
Scopolamine is a muscarinic cholinergic antagonist that has been utilized in many research to comprehend, discover, & describe therapeutic targets for Alzheimer's disease. It does this by changing the cholinergic system & inducing Alzheimer's disease-like pathology both in vivo and in vitro. Scopolamine damages synaptic integrity & causes synaptic dysfunction, neuroinflammation, & neurodegeneration. It may also increase the generation of lipid peroxidation & reactive oxygen species. Finally, scopolamine suppresses the secretion of neurotrophic nerve growth factor & the growth of neuroblastoma cells. Furthermore, as an inhibitor of protein kinase, the scopolamine analog H-89 can dramatically impair the capacity for spatial learning. One example of this is the H-89-induced spatial learning problem in male rats. [46]
Glutamate Hypothesis:
As an essential component of brain plasticity processes, it is the primary neurotransmitter that excites within the mammalian Central nervous system. However, an abundance of acute and chronic brain pathologies, such as brain trauma, seizures, neurodegenerative illnesses, and cerebral ischemia injury, are linked to glutamate excess. Life requires the regulation of glutamate since excessive glutamate production causes excitotoxicity & low glutamate levels impair the survival of neuronal cells. Increased N-methyl-D-aspartate activity, which at a pathological level result in impairment of synaptic function & neuronal cell death, is primarily responsible for the increase in intracellular calcium that causes excitotoxicity. Reactive oxygen species and calcium interact significantly, & this pathogenic increase in calcium causes an increase in reactive oxygen species. [47]
Genetic Hypothesis:
Gene changes affecting the presenilin1, presenilin2, and amyloid precursor proteins are typically the cause of early Alzheimer’s disease. On the other hand, the ?-4 allele in the gene for apolipoprotein E is mostly linked to a polymorphism in late-form Alzheimer’s disease. A key player within the ?-secretase complex's activation and crucial to the synthesis of amyloid-beta from amyloid precursor protein is presenilin1. Alzheimer’s disease which develops late and is inherited as well as sporadic has been linked to the Apolipoprotein E gene. Apolipoprotein E e4 allele status is a significant Alzheimer's disease risk factor. The gene's exon 4 contains the Apolipoprotein E ?4 locus. ApoE3 is the most prevalent type of Apolipoprotein E. Amyloid aggregation is mediated by Apolipoprotein E?4 and tau is mediated by Apolipoprotein E ?4 Both tau hyperphosphorylation and amyloid aggregation are mediated by Apolipoprotein E?4 (Bekris LM; et al.,2010). ApoE?4 was also shown to be associated with vascular damage in the brain, which leads to Alzheimer’s disease pathogenesis. [48]
Hirano Bodies Hypothesis:
They were initially identified in Parkinson's disease patients. Hematoxylin and eosin staining revealed the presence of these rod-like inclusions, which are rich in Filamentous-actin & actin-binding proteins, within dendrites of neurons. Additionally, they have been seen in middle-aged & older healthy individuals, as well as in a range of ailments outside Alzheimer's disease. It is in the hippocampus cornu ammonis1 (CA1) region where they are most commonly observed. They are more prevalent and abundant in individuals with Alzheimer's disease in contrast to healthy controls, although it is unclear how they contribute to the pathogenesis of the illness. More recently, it’s been proposed that Hirano bodies are linked with worse synaptic responses & decreased spatial working memory through the use of animal models that produce mutant actin-binding proteins. Further research is needed for a better understanding of their biological role in Alzheimer’s disease. [49]
Energy Metabolism Hypothesis:
Empirical studies have demonstrated the function of abnormal brain energy metabolism in the development of central nervous system-related disorders, compromising Parkinson's, Alzheimer’s, & Huntington's diseases. Under physiological settings, the main energy source that the brain needs is glucose, one of the body's most energy-dependent organs. Disorders of the central nervous system, such as Alzheimer’s patients have been shown to exhibit dysfunction in the energy supply. Compared to controls, Alzheimer's disease patients have considerably less cerebral glucose metabolism. On the other hand, decreased glucose metabolism in areas that depend on glucose metabolism—like the parietal, temporal, and prefrontal cortices—is linked to cognitive impairment. [50]
Insulin Hypothesis:
Insulin resistance and a decrease in insulin receptors have been demonstrated in the minds of those suffering from Alzheimer's. In addition, late-stage diabetes causes the brain to become resistant to insulin. This could lead to energy deficiencies, which could subsequently cause oxidative stress because cells largely rely on the metabolism of glucose to produce energy. Furthermore, insulin's role in neurotransmission and ability to be neuroprotective in the face of insults like ischemia have been established. Moreover, evidence has shown that in response to insulin and metabolic inhibitors, both wild-type & transgenic mice (a transgenic model that is derived from the amyloid precursor protein) showed increased levels of beta-secretase. In transgenic mice 2576, this also resulted in elevated levels of amyloid-beta. Nonetheless, given that some individuals observe a protective effect of insulin, there probably exists a threshold for this hormone that permits the brain to operate at its best. [51]
Metal ion Hypothesis:
Due to their necessity for controlling numerous other biological processes as well as synaptic neuronal activity, metal ions are crucial for brain function. The core & rims of senile plaques in Alzheimer's patients have been demonstrated to contain Cu2+, Zn2+, and Fe2+. This finding raises the possibility that metal ion sequestration into plaques may be the cause of the inadequate distribution of these metals in the surrounding areas. As the primary intracellular iron storage protein in the body, ferritin is highly correlated with levels of apolipoprotein E in the cerebrospinal fluid. This is because the Alzheimer's risk allele, Apolipoprotein E -?4, raises ferritin levels. Alzheimer's disease brain tissue contains higher concentrations of it, and metal ion homeostasis is a defining characteristic in Neurological illnesses caused by amyloid formation. [52]
Locus Coeruleus Hypothesis:
The locus coeruleus is the major source of noradrenaline, a neuromodulator that has a key role in cognition, mood, and behavior. This data suggests that Alzheimer’s disease is connected to widespread locus coeruleus deterioration. According to post-mortem evidence, the first pathology of Alzheimer’s disease that may be identified is tau deposition in the locus coeruleus. Compared to normal aging, Alzheimer's disease causes a larger loss of locus coeruleus neurons. According to reports, the early cognitive abnormalities in Alzheimer's disease may be connected to pathological alterations in the locus coeruleus. [46]
Neurodevelopmental And Neurotransmission Process Hypothesis:
Alzheimer's disease development, and specifically its cognitive symptoms, is probably linked to neurodevelopmental and neurotransmission pathways. Numerous studies have shown that Alzheimer's disease brains contain much lower levels of serotonin, dopamine, and norepinephrine as well as the receptors for these chemicals. Depression, anxiety, and agitation are caused by serotonin loss; defects in reward-mediated memory formation are caused by dysregulated dopamine release; and impaired spatial memory function is caused by low norepinephrine levels. There is a corresponding decrease in dopamine outflow in the hippocampus along with the loss of dopaminergic neurons. Deficits in impairment in reward processing, as well as memory and synaptic plasticity dependent on the hippocampal region, may be substantially attributed to the lower Dopamine outflow in the hippocampus, brain regions that are principally implicated in memory & reward, respectively. [53]
Vascular Dysfunctions Hypothesis:
Early in an illness's etiology, vascular dysfunction can lead to cognitive impairment and the advancement of the illness. Loss of tight connections damages the blood-brain barrier in Alzheimer’s disease patients. Fibrinogen and other blood proteins can permeate the brain parenchyma due to this vascular injury. De la Torre and Mussivand published the first formal proposal in 1993, linking poor neurovascular coupling to the etiology of Alzheimer’s disease. A reduction in the early disease etiology & damage to the vasculature are among these alterations, which may hasten the course of the illness and impair cognition. [54]
Microbiota-Gut-Brain Axis Hypothesis:
Hippocrates, the Greek physician regarded as the founder of modern medicine, is credited with saving more than 2,000 years ago that "all disease begins in the gut." About 1014 bacteria comprise the human gut microbiota, which controls several functions such as central and peripheral neurotransmission, immunological and inflammatory responses, and the metabolism of vitamins and glucose. Obesity, addiction, type 2 diabetes, cancer, aging, pain, stroke, and neurodegenerative illnesses are among the conditions it actively influences. Research has indicated that memory maintenance is significantly influenced by the gut flora, and probiotic supplements such as Lactobacillus and Bifidobacterium have been demonstrated to improve memory in mice. Methane, hydrogen sulfide, ammonia, & nitric oxide with microbial origins are important for neurophysiology & could contribute to Alzheimer's disease pathogenesis illness. [55]
Nitrosative Stress Hypothesis:
Nitrosative stress is the result of several defense mechanisms not being able to control the production of reactive nitrogen species, which damages components found inside cells. Nitric oxide, a signaling molecule that regulates neurotransmission, synaptic plasticity, and brain growth, is the primary constituent of reactive nitrogen species. Synapse disruption and glial activation have been linked to notable cognitive impairment in response to nitrosative stress. It has been found that the nitric oxide produced via amyloid-beta in Alzheimer’s disease leads to mitochondrial fission because of S-nitrosylation, which results in synaptic dysfunction and neuronal death. [56]
Ubiquitin-Proteasome System Hypothesis:
The ubiquitin-proteasome pathway assists in preserving cellular integrity by removing proteins that are misfolded or aggregated. The buildup of toxic and improperly folded proteins in brain cells, which happens when this mechanism for getting rid of undesirable protein complexes is interfered with, is thought to be one pathogenic aspect of Alzheimer’s disease. The survival & stability of neurons depends on the effective removal of aberrant protein waste, which can only be achieved via this pathway. [57]
Autophagy Lysosome Pathway Hypothesis:
The pathophysiology has also been linked to autophagy and lysosomal dysfunction. Tau clearance and amyloid-beta production and clearance are both influenced by autophagy. Through the endo-lysosomal route, amyloid precursor protein amyloidogenic processing is trafficked. Many genes linked to Alzheimer’s disease, such as Bridging-Integrator 1, Sortilin-related receptor1 (SORL1), & phosphatidyl-inositol-binding clathrin assembly protein (Picalm), are involved in endosomal recycling, & research suggests that some of these genes may be directly engaged in the amyloid precursor protein's processing endosomes. [58]
MEDICINAL PLANTS AGAINST ALZHEIMER’S DISEASE [59, 60, 61, 62]
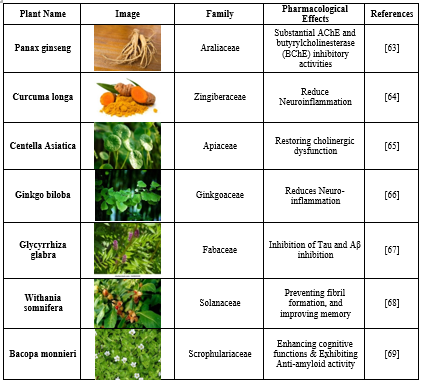
Medicinal plants have been used for medical purposes worldwide since the beginning. Natural products have attracted a lot of attention and helped in the creation of novel medications. The neurotransmitter systems in the brain that are made up of neurons can be supported by medicinal herbs. An imbalance in neurotransmitters can lead to a variety of neurological and mental health conditions. Neurotransmitters are chemical messengers that carry signals between nerve cells. The possibility that certain medicinal plants may affect the amounts and functions of neurotransmitters has been investigated. Because plant extracts can affect numerous targets at once, they may be a more effective and innovative therapeutic option for Alzheimer's disease than single medications. Plants include crucial secondary metabolites, such as alkaloids, flavonoids, and phenolic acids, which are important in avoiding neurodegenerative diseases. The ability of medicinal herbs to treat Alzheimer's disease has been proven. People who take anti-dementia medications may also develop other health issues; the effects of these conditions may differ based on the patient's reaction and the specific drug. Individuals who are on anti-dementia drugs, like N-methyl-D-aspartate receptor antagonists & acetyl-cholinesterase inhibitors, have had withdrawal symptoms. Several adverse effects have been recorded, including excitement, insomnia, nausea, vomiting, diarrhea, delusions, visual hallucinations, pornomania, hallucinations, & aggressive behavior. Consequently, developing Alzheimer's disease natural treatments is currently the main focus. Herbal therapy has proven to be a useful tool for managing symptoms and delaying the advancement of Alzheimer's disease. Pharmaceuticals made from medicinal plants are increasingly being produced and marketed, and their importance to healthcare is growing from a commercial and scientific standpoint. Alzheimer's disease can be managed with medicine even if there isn't a recognized cure for it. Providing information about plants that are used to enhance cognition in Alzheimer's patients was our main objective when putting together this review. Patients share knowledge about plants that help Alzheimer's patients think more clearly.
Table 1: Herbs that are neuroprotective in Ayurveda. Herbs are used extensively in Ayurvedic medicine to treat various ailments. Ayurveda intensively investigates the unique therapeutic properties of every section of the plant. The Ayurvedic treatment of neurological illnesses with nootropic herbs is highlighted in the table.
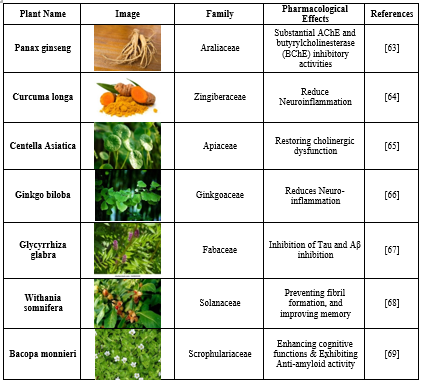
Neurodegenerative diseases are nervous system disorders that are often characterized by a selective loss of neurons. Research has shown that changes in the physicochemical characteristics of proteins result in their accumulation in the human brain, which ultimately causes neuronal degeneration. The death and morbidity rates in affluent nations are sharply rising due to neurodegenerative disorders, for which there is now no known therapy. Developing nations should expect the same outcome as the body of information grows. Along with other systemic disorders like cardiovascular, respiratory, renal, gastrointestinal, and many others, neuropsychiatric & neurological disorders like depression, anxiety, and schizophrenia, the most common illnesses are head traumas, cerebrovascular impairment, amyotrophic lateral sclerosis, Parkinson's disease, Alzheimer's disease, and Huntington's disease in the twenty-first century. The management of neurodegenerative disorders is the only basis for the current remedies; actual treatment for these diseases has not yet been investigated. Neurodegenerative illnesses have long been treated with plant-derived substances, or phytomedicines, such as flavonoids and alkaloids. They may be the most efficient therapeutic and management tools for reducing the critical symptoms of neurodegenerative illnesses like Alzheimer's. [98]
CONCLUSION:
The increasing number of cases of Alzheimer's disease has made it a global health concern. Both neurodegeneration and cognitive impairment are caused by it. While treatment for hypertension, depression, and neurodegenerative disorders is frequently costly, has side effects, and is generally ineffective, these conditions are developing at a phenomenal and frightening rate. To conclude, the effectiveness of treating Alzheimer's disease is contingent upon understanding the pathophysiology underlying the condition, given the multitude of pathogenic pathways involved. Thus, this review's primary goal is to give an overview of the accepted theories now in use about the etiology of Alzheimer’s disease. Additionally, we emphasize the risk components connected to the disease that exacerbate the disease's symptoms. Thus, preventing these risk factors could slow down the neurodegenerative disease's course. It was also mentioned that herbal remedies are a readily available and efficient way to cure Alzheimer's disease. An immediate need is the development of a potent, targeted, and effective drug to handle those with Alzheimer's disease & those who are in danger of developing the disease. Research on our indigenous herbs is necessary to produce effective antidisease medications. Given that Alzheimer's disease is influenced by multiple factors at both the onset & progression of the disease, a major change in the strategy for medication development from a single target to multiple targets might yield a more successful approach to medication development. In such situations, Herbal ingredients work best. Moreover, herbal remedies will surely yield encouraging outcomes because they have been used for ages, are unlikely to cause any negative side effects, and are reasonably priced. In the future, the novel functional identification for Alzheimer's disease may prove useful.
REFERENCES
- Braun B, Demling J, Loew. Alzheimer’s disease: history, ethics, and medical humanities in the context of assisted suicide. Philos Ethics Humanit Med. 2022;1:667-678.
- Breijyeh Z, Karaman R. Comprehensive Review on Alzheimer's Disease, Causes and Treatment. Molecules 2020;6:25(24).
- Pramod S, Shyamlila B. (Alzheimer Disease: A Review International Journal of Research Publication and Reviews. 2021;2:240-241.
- Sobue A, Komine O, Yamanaka K. Neuroinflammation in Alzheimer’s disease: microglial signature and their relevance to disease. Inflamm Regener. 2023;4:56-67.
- Schweighauser M, Arseni D, Bacioglu M. Age-dependent formation of TMEM106B amyloid filaments in human brains. Nature. 2022;6:310–314.
- Thakur A. Kamboj P. Goswami K. Pathophysiology and management of Alzheimer’s disease: an overview. J Anal Pharm Res. 2018;9(2): 67-89.
- Zetterberg, H., Bendlin, B. Biomarkers for Alzheimer's disease- preparing for a new era of disease-modifying therapies. Mol Psychiatry. 2021;26(1):296-308.
- Xu, H., Liu, Z., and Liu, Y. Administration of midazolam in infancy does not affect the learning and memory of adult mice. Clin Exp Pharmacol Physio. 2009; 36:1144–1148.
- Akram M, Nawaz A. Effects of medicinal plants on Alzheimer's disease and memory deficits. Neural Regen Res. 2017;2(4):660-670.
- Mishra S, Palanivelu K. The effect of curcumin (turmeric) on Alzheimer's disease: An overview. Ann Indian Acad Neurol. 2008;1:13-9.
- Anil K, Jaskirat S, Amandeep G. Alzheimer disease review Treasure Island. 2022;29(6):67-89.
- Ahmad F, Cisewski J, Xu J, Anderson R. Provisional Mortality Data - United States, 2022. MMWR Morb Mortal Wkly Rep. 2023;72(18):488-492.
- Qiu, C, Kivipelt M, Strauss E. Epidemiology of Alzheimer's disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009;11(2):111-128.
- Braak H, Thal R, Ghebremedhin E, Tredici K. Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J Neuropathol Neurol. 2011;70(11):960-969.
- Silva M, Loures C, Alves V. Alzheimer’s disease: risk factors and potentially protective measures. J Biomed Sci. 2019;2:33-45.
- Burgio L. Interventions for the behavioral complications of Alzheimer's disease: behavioral approaches. Int Psychogeriatr 1996;1:45-52.
- Koyama A, Hashimoto M, Todani S. Malnutrition in Alzheimer’s disease, dementia with Lewy bodies, and frontotemporal lobar degeneration: Comparison using serum albumin, total protein, and hemoglobin level. PLoS ONE. 2016;11:455-456.
- Brenowitz W, Yaffe K. Depressive Symptoms Imputed Across the Life Course Are Associated with Cognitive Impairment and Cognitive Decline. J Alzheimers. 2021;83(3):1379-1389.
- Traber M, Reznick A. Cross E. Tobacco-related diseases. Is there a role for antioxidant micronutrient supplementation? Clin Chest Med. 2000;21(1):173–187.
- Sommerlad A, Ruegger J, Singh A, Lewis G. Livingston G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Psychiatry. 2018;89(3):231–238.
- Vilalta J, Lopez S, Merino J, Garre J. Depression subtypes and 5-year risk of dementia and Alzheimer disease in patients aged 70 years. Int J Geriatr Psychiatry. 2013;28(4):341–350.
- Popp J, Meichsner S, Kolsch H, Lewczuk P. Cerebral and extracerebral cholesterol metabolism and CSF markers of Alzheimer's disease. Biochem Pharma. 2013;86(1):37–42.
- Bekris LM, Tsuang D, Yu CE, Bird TD. Genetics of Alzheimer's disease. J Geriatr Psychiatry Neurol. 2010;23(4):213-227.
- Sochocka M, Zwoli?ska K, Leszek J. The Infectious Etiology of Alzheimer's Disease. Curr Neuropharmacol. 2017;15(7):996-1009.
- Kim J, Castellano J, Jiang H, Basak M. Overexpression of low-density lipoprotein receptors in the brain markedly inhibits amyloid deposition and increases extracellular A? clearance. Neuron. 2009;64:632-644.
- Croze M, Zimmer L. Ozone atmospheric pollution and Alzheimer’s disease: From epidemiological facts to molecular mechanisms. J. Alzheimer’s Dis. Jad. 2018;62:503-522.
- Love S, Miners J. Cerebrovascular disease in aging and Alzheimer's disease. Acta Neuropathol. 2016;1(5):645-58.
- Edwards G, Gamez N, Escobedo G, Calderon O, Moreno-Gonzalez, I. Modifiable Risk Factors for Alzheimer’s Disease. Frontiers in Aging Neuroscience. 2019;1:97-112.
- Profenno L, Porsteinsson P, Faraone S. Meta-analysis of Alzheimer's disease risk with obesity, diabetes, and related disorders. Biol Psychiatry. 2010;67(6):505–512.
- Flores J, Pérez A, Alba G, Flores-Cordero A. Obesity as a Risk Factor for Dementia and Alzheimer's Disease: The Role of Leptin. Int J Mol Sci. 2022;23(9):5202-5206.
- Forestier A, Douki T, Rachidi W, Bael D, Rosa VD. Combination of A? Secretion and Oxidative Stress in an Alzheimer-Like Cell Line Leads to the Over-Expression of the Nucleotide Excision Repair Proteins DDB2 and XPC. Int. J. Mol. Sci. 2015;16:224-226.
- Bartus R, Dean R, Beer B, Lippa A. The cholinergic hypothesis of geriatric memory dysfunction. Science. 1982;2(7):408-414.
- Lobo A, Launer L, Fratiglioni L, Andersen K, Hofman A. Prevalence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology. 2000;11(5):9-15.
- Funderburk F, Marcellino B, Yue Z. Cell “self-eating” (autophagy) mechanism in Alzheimer's disease. Mt Sinai J Med. 2010;7:59-68.
- Michel H, Kumar S, Pinotsi D, Tunnacliffe A, George P, Mandelkow E. Extracellular monomeric tau protein is sufficient to initiate the spread of tau protein pathology. J. Biol. Che. 2014;289:956-967.
- Stancu C, Vasconcelos B, Terwel D, Dewachter I. Models of beta-amyloid induced Tau-pathology: the long and “folded” road to understand the mechanism. Mol Neurodegener. 2014;9:51-57.
- Rubio M, Morillas M. A review: inflammatory process in Alzheimer's disease, the role of cytokines. Scientific World Journal. 2012;3:75-86.
- Sheppard O, Coleman M, Durrant S. Lipopolysaccharide-induced neuroinflammation induces presynaptic disruption through a direct action on brain tissue involving microglia-derived interleukin 1 beta. J Neuroinflammation. 2019;16(1):106-112.
- Wong K, Roy J, Fung L, Heng C, Zhang C, Lim W. Relationships between Mitochondrial Dysfunction and Neurotransmission Failure in Alzheimer's Disease. Aging Dis. 2020;11(5): 1291-1316.
- Rhein V, Song X, Wiesner A, Ittner M, Baysang G, Meier F, Ozmen L, Bluethmann H, Drose S, Brandt U, Savaskan E, Czech C, Gotz J, Eckert A. Amyloid-beta and tau synergistically impair the oxidative phosphorylation system in triple transgenic Alzheimer's disease mice. Proc Acad Sci. 2009;10:20057–20062.
- Ortiz G, Velazquez I, Torres E. Alzheimer's Disease and SARS-CoV-2: Pathophysiological Analysis and Social Context. Brain Sci. 2022;12(10):1405-1409.
- Homolak J, Mudrovcic M, Vuki? B, Toljan K. Circadian Rhythm and Alzheimer's Disease. Med Sci (Basel). 2018;6(3):52-67.
- Evgeni P. The role of Serotonin Receptors in Alzheimer’s disease. Opera medica ET physicology. 2016;2(1):244-254.
- Pierson R, Kolling J, James D, Pushpavathi G, Marcinkiewcz A. Serotonergic dysfunction may mediate the relationship between alcohol consumption and Alzheimer’s disease. Pharmacological Research. 2024;1:202-223.
- Janicki S, Schupf N. Hormonal influences on cognition and risk for Alzheimer's disease. Curr Neurol Neurosci Rep. 2010;10(5):359-366.
- Chen Y, Chen T, Hou R. Locus coeruleus in the pathogenesis of Alzheimer's disease: A systematic review. Alzheimers Dement (N Y). 2022;8(1):122-134.
- Huang T, Shu Y, Cai D. Genetic differences among ethnic groups. BMC. 2009;16:1093- 1097.
- Kim J, Castellano J, Jiang H, Basak M. Overexpression of low-density lipoprotein receptors in the brain markedly inhibits amyloid deposition and increases extracellular A? clearance. Neuron. 2009;64:632-644.
- Hirano A. Hirano bodies and related neuronal inclusions. Neuropath Neurobiol. 1994;20:3– 11.
- Van V, Teav T, Gallart H, Mehl F, Konz I, Clark C, Oikonomidi A, Peyratout G, Henry H, Delorenzi M, Ivanisevic J, Popp J. Systemic and central nervous system metabolic alterations in Alzheimer's disease. Alzheimers Res Ther. 2019;11(1):93-109.
- Ferreira L, Fernandes S, Vieira M, Felice F. Insulin resistance in Alzheimer’s disease. Front Neurosci. 2018;2:1-11.
- Cristovao S, Santos R, Gomes M. Metals and Neuronal Metal Binding Proteins Implicated in Alzheimer's Disease. Oxid Med Cell Longev. 2016;2:98-112.
- Nobili A, Latagliata E, Viscomi M. Dopamine neuronal loss contributes to memory and reward dysfunction in a model of Alzheimer’s disease. Nat Commun. 2017;8:147-154.
- Badimon A, Torrente D, Norris E. Vascular Dysfunction in Alzheimer's Disease: Alterations in the Plasma Contact and Fibrinolytic Systems. Int J Mol Sci. 2023;24(8):7046-7057.
- Cryan J, Riordan J, Sandhu K, Clarke G. The Microbiota-Gut-Brain Axis. Physiol Rev. 2013;99(4):1877-2013.
- Zahid, S., Khan, R., Oellerich, M., Ahmed, N., and Asif, A. Differential S-Nitrosylation of Proteins in Alzheimer’s Disease. Neuroscience. 2014;2:126–136.
- Gadhave K, Ahmed S, Lahkar M. The Ubiquitin Proteasomal System: A Potential Target for the Management of Alzheimer’s Disease. J. Cell. Mol. Med. 2016;20:1392-1407.
- Selkoe D, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608.
- Sharma P, Srivastava P, Seth A. A comprehensive review of mechanisms of pathogenesis involved in Alzheimer's disease and potential therapeutic strategies. Prog Neurobiol 2019;174:53–89.
- Winslow B, Onysko M Stob M, Hazlewood K. Treatment of Alzheimer's disease. Am Fam Physician. 2019;83(12):1403–1412.
- Rao V, Descamps O, John V, Bredesen D. Ayurvedic medicinal plants for Alzheimer disease: a review. Alzheimers Res Ther. 2012;4(3):1–9.
- Grodzicki W, Dziendzikowska K. The role of selected bioactive compounds in the prevention of Alzheimer's disease. Antioxidant. 2020;9(3):229-234.
- Liu H, Lu X, Hu Y, Fan X. The chemical constituents of Panax ginseng and Panax notoginseng explain why they differ in therapeutic efficacy. Pharmacol. Res. 2020;6:161- 171.
- Karri S, Sharma S, Hatware K, Patil K. Natural anti-obesity agents and their therapeutic role in the management of obesity: A future trend perspective. Biomed. Pharmaco. 2019;110:224-238.
- Gray N, Zweig A, Caruso M, Zhu YJ, Wright MK. Centella Asiatica attenuates hippocampal mitochondrial dysfunction and improves memory and executive function in ?-amyloid overexpressing mice. Mol. Cell. Neurosci. 2018;93:1-9.
- Zhang Y, Zhao Y, Zhang J, Gao Y, Li S, Chang C, Yu D, Yang G. (2021). Ginkgolide B inhibits NLRP3 inflammasome activation and promotes microglial M2 polarization in A?1-42-induced microglia cells. Neurosci Lett. 2021;764-771.
- Simayi Z, Rozi P, Yang X, Ababaikeri G. Isolation, structural characterization, biological activity, and application of Glycyrrhiza polysaccharides: Systematic review. Int. J. Biol. Macromol. 2021;183:387–398.
- Choudhary D, Bhattacharyya S, Bose S. Efficacy and Safety of Ashwagandha Withania somnifera Root Extract in Improving Memory and Cognitive Functions. J. Diet. Sup. 2017;14:599-612.
- Dubey T, Chinnathambi S. Brahmi Bacopa monnieri: An ayurvedic herb against Alzheimer’s disease. Arch. Biochem. Biophys. 2019;676:108-112.
- Sharma A, Bajaj P, Bhandari A, Kaur G. From ayurvedic folk medicine to the preclinical neurotherapeutic role of a miraculous herb, Tinospora cordifolia. Neuro Int. 2019;1:141-146.
- Bihaqi S, Singh A, Tiwari M. In vivo investigation of the neuroprotective property of Convolvulus pluricaulis in scopolamine-induced cognitive impairments in Wistar rats. Indian J Pharmacol. 2011;43:520–525.
- Kumar H, Gupta K. The antioxidant property of Celastrus paniculatus wild: a possible mechanism in enhancing cognition. Phytomedicine. 2002;9:02-211.
- Pakade V, Cukrowska E, Chimuka L. Comparison of antioxidant activity of Moringa oleifera and selected vegetables in South Africa. S Afr J Sc. 2013;109: 1–5.
- Akram M, Nawaz A. Effects of medicinal plants on Alzheimer's disease and memory deficits. Neural Regen Res. 2017;2(4):660-670.
- Pramodinee D, Mahesh M, Niranjan D, Sankpala S. Memory enhancing activity of Cissampelos papiera in mice. Int J Pharm Sci. 2011;3:206–211.
- Hamidpour R. Rosmarinus officinalis (Rosemary): a novel therapeutic agent for antioxidant, antimicrobial, anticancer, antidiabetic, antidepressant, neuroprotective, anti-inflammatory, and anti-obesity treatment. Biomed J Sci Tech Res. 2017;1(4):1098-10113.
- Hussain G, Rasul A, Anwar H, Aziz N. Role of Plant-Derived Alkaloids and Their Mechanism in Neurodegenerative Disorders. Int J Biol Sci. 2018;14(3):341-357.
- Bordoloi S, Pathak K, Devi M, Saikia R, Das J. Some promising medicinal plants used in Alzheimer’s disease: an ethnopharmacological perspective. Discov Appl Sci. 2024;6:215- 218.
- Heinrich M, Teoh L. Galanthamine from Snowdrop—the development of a modern drug against Alzheimer’s disease from local Caucasian knowledge. Ethnopharmacol. 2004;92(2– 3):147–62.
- Lyle N, Bhattacharyya D. Stress modulating antioxidant effect of Nardostachys jatamansi. Indian J Biochem Biophys. 2009;46:93-98.
- Vasudevan M, Milind P. Memory enhancing activity of Coriandrum sativum in rats. J Pharmacol. 2009;2:827–839.
- Saxena V, Ahmad H, Gupta R. Memory enhancing effects of Ficus carica leaves in hexane extract on interoceptive behavioral models. Asian J Pharm Clin Res. 2013;6:109–113.
- Colpo G, Trevisol F, Teixeira A, Rocha B. Ilex paraguariensis has antioxidant potential and attenuates haloperidol-induced orofacial dyskinesia and memory dysfunction in rats. Neurotox Res. 2007;12:171-180.
- Gujra S, Singh S, Pal R, Singh S, Nath C. Gugu lipid, an extract of Commiphora whighitti with lipid-lowering properties, has protective effects against streptozotocin-induced memory deficits in mice. Pharmacol Biochem Behav. 2007;8:797-805.
- Ramachandran S, Sanjay S, Dhanaraju M. Antiamnesic effect of Piracetam potentiated with Emblica officinalis and Curcuma longa in aluminum-induced neurotoxicity of Alzheimer's disease. Inter J Adv Res. 2013;1:185–196.
- Lee Y, Yuk D, Kim T, Hong J. Protective effect of the ethanol extract of Magnolia officinalis and 4-O-methyl honokiol on scopolamine-induced memory impairment and the inhibition of acetylcholinesterase activity. J Nat Med. 2009;63:274-282.
- Malhotra S, Singh A. Medicinal properties of ginger (Zingiber officinale Rosc.) Nat Prod Rad. 2003;2:296-301.
- Das A, Mandal S, Banerjee S, Sinha S, Das J. Studies on antidiarrhoeal activity of Punica granatum seed extract in rats. J Ethnopharmacol. 1999;168:205-208.
- Akhondzadeh S, Noroozian M, Mohammadi M. Salvia officinalis extract in the treatment of patients with mild to moderate Alzheimer's disease: a double-blind, randomized and placebo-controlled trial. J Clin Pharm Ther. 2003;28:53–59.
- Eidi M, Eidi A, Bahar M. An effect of Salvia officinalis leaves on memory retention and its interaction with the cholinergic system in rats. J Nut. 2006;2:321-326.
- Maeda A, Tanimoto S, Abe T, Kazama S. Chemical constituents of Myristica fragrans Houttuyn seed and their physiological activities. Yakugaku Zassh. 2008;128:129-133.
- Nahata A, Patil K, Dixit K. Effect of Evolvulus alsinoides Linn. on learning behavior and memory enhancement activity in rodents. Phytother Res. 2010;4:486-493.
- Faiyaz A, Narendra J, Sharath C. Acetylcholine and memory-enhancing activity of Ficus racemosa bark. Pharmacog Res. 2011;3:246-249.
- Rajagopal P, Ashlyjames K. Acorus calamus Journal of Internation Academic Research for Multidisciplinary. 2013;1(9):1-14.
- Sepide Miraj, Sara Kiani. A review study of therapeutic effects of Salvia officinalis L, Scholars Research Library. 2016;8(6):299-303.
- Giulio K, Pasinetti O. Role of grape seed polyphenols in Alzheimer’s disease neuropathology, NutrDiet Suppl .2010;2:97-103.
- Praveen, K., and Yellamma, K. Insilco Identification of Suitable Acetylcholinesterase Inhibitors from Morinda citrifolia Linn. Concerning Alzheimer’s disease. Int J Pharm Sci. 2014;5(12):5474-5481.
- Hussain G, Rasul A, Anwar H, Aziz N. Role of Plant-Derived Alkaloids and Their Mechanism in Neurodegenerative Disorders. Int J Biol Sci. 2018;14(3):341-357.


 Shruti*
Shruti*
 Kamal Kishore Maheshwari
Kamal Kishore Maheshwari

 10.5281/zenodo.13296522
10.5281/zenodo.13296522