Abstract
Hyperthyroidism is characterized by an overproduction and release of thyroid hormones from the thyroid gland. In contrast, thyrotoxicosis refers to the clinical symptoms arising from excessive circulating thyroid hormones, regardless of their source. Graves’ disease is the most common cause of hyperthyroidism, followed by toxic nodular goiter. Other significant causes of thyrotoxicosis include thyroiditis, iodine-induced or drug-induced thyroid dysfunction, and factitious ingestion of thyroid hormones. The treatment for hyperthyroidism typically Involves antithyroid drugs, radioactive iodine therapy, or surgery. However, antithyroid drugs are generally not used long-term in toxic nodular goiter due to a high recurrence rate of thyrotoxicosis. Beta-blockers are employed to manage the symptoms of thyrotoxicosis and may be the sole treatment required for conditions where thyroid hormones are not excessively produced or released. Thyroid storm, hyperthyroidism during pregnancy, and the postpartum period are special cases that necessitate careful evaluation and treatment.
Keywords
Goitre, Hyperthyroidism, Iodine, Overproduction, Thyroid, Thyroidectomy.
Introduction
The thyroid gland, a butterfly-shaped organ located in the neck, plays a pivotal role in regulating various bodily functions, particularly metabolism. It produces hormones that influence how the body uses energy, grows, and develops.?1;
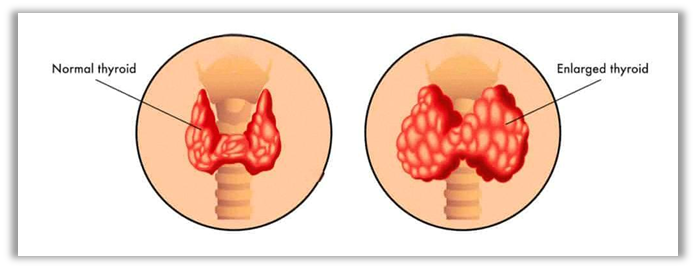
The thyroid gland, a butterfly-shaped organ situated below the larynx, is comprised of two lateral lobes connected by an isthmus anterior to the trachea. Approximately half of thyroid glands possess a smaller third lobe known as the pyramidal lobe. The normal weight of the thyroid gland is approximately 30 grams. The majority of the thyroid gland is composed of microscopic spherical sacs called thyroid follicles. The walls of these follicles consist primarily of follicular cells, many of which extend into the lumen of the follicle. A basement membrane encircles each follicle. When follicular cells are inactive, their shape is low cuboidal to squamous; however, under the influence of thyroid-stimulating hormone (TSH), they become active in secretion and assume a cuboidal to low columnar shape. Follicular cells produce two hormones: thyroxine (T4), also known as tetraiodothyronine, and triiodothyronine (T3). T4 and T3, collectively referred to as thyroid hormones, contain four and three iodine atoms respectively. A few cells called parafollicular cells or C cells are located between follicles. These cells produce the hormone calcitonin, which plays a crucial role in regulating calcium homeostasis.
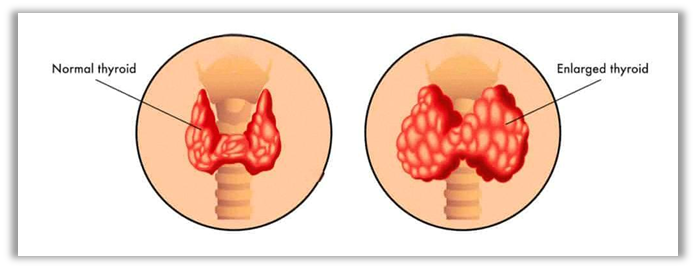
Fig 1 – Thyroid gland (Normal v/s Hyperthyroidism)
The thyroid gland, one of the body’s largest endocrine glands, originates as an epithelial thickening in the pharyngeal floor. This thickening extends outward from the pharynx, eventually losing its connection with the gastrointestinal tract. It subsequently develops into two lobes situated laterally to the trachea, positioned below the larynx. These lobes are joined by a thin band of tissue on the anterior side, known as the isthmus. The thyroid gland is highly vascularized, receiving a substantial blood supply. It is composed of hollow spherical follicles lined by cuboidal cells. The shape of these follicular cells varies with their activity, becoming taller and more columnar during periods of active secretion and flattening when inactive. The follicular cells secrete the hormones thyroxine (T4) and triiodothyronine (T3). Interspersed between the follicles are a few cells called parathyroid cells, which secrete the hormone calcitonin.?2; These hormones regulate a wide range of bodily functions, including:
Metabolism, Growth and development, Body temperature, Heart rate, Bone health.?1;
Etiology of Hyperthyroidism:-
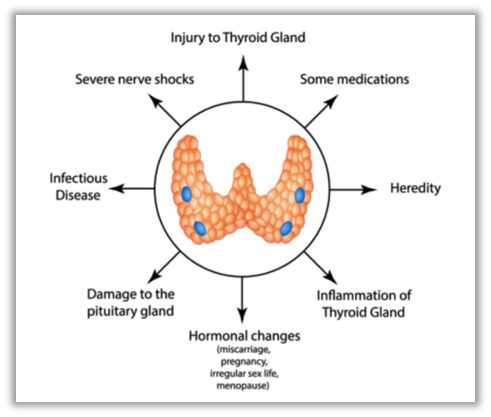
Hyperthyroidism arises when the thyroid gland releases an excessive quantity of thyroid hormones into the bloodstream. Several conditions can contribute to this state, including:
a) Graves’ Disease: An autoimmune disorder characterized by the immune system’s aberrant attack on the thyroid gland. This assault stimulates the thyroid to produce an overabundance of thyroid hormone, making it the most prevalent cause of hyperthyroidism.
b) Overactive Thyroid Nodules: Also referred to as toxic adenoma, toxic multinodular goiter, or Plummer disease, this condition occurs when a thyroid adenoma secretes excessive thyroid hormone. An adenoma is a compartmentalized region within the gland that forms non-malignant lumps, often leading to an enlarged thyroid.?3;
c) Thyroiditis: This condition involves inflammation of the thyroid gland, frequently due to an autoimmune disorder or an unidentified cause. The inflammation can result in the leakage of stored thyroid hormone into the bloodstream, causing symptoms of hyperthyroidism.
d) Excessive Iodine Intake: Iodine is a vital nutrient for thyroid hormone synthesis. However, excessive iodine consumption can lead to hyperthyroidism, a condition characterized by the overproduction of thyroid hormones. Certain cough syrups, medications, particularly heart medications, and seaweed-based products are known to contain significant amounts of iodine.
e) Too much thyroid hormone medications: Individuals with hypothyroidism who rely on thyroid hormone replacement therapy must exercise caution to avoid overdosing. Additionally, interactions between thyroid hormone medication and other drugs can elevate hormone levels, necessitating careful consideration when starting new treatments.?
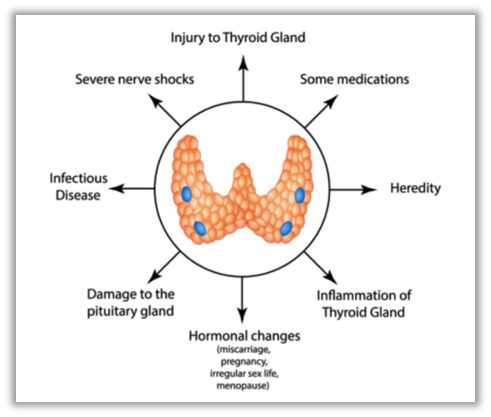
Fig 2 – Basic etiology of Hyperthyroidism
Epidemiology of Hyperthyroidism: -
Several studies have investigated the prevalence of hyperthyroidism. An epidemiological study conducted in Cochin found that subclinical and overt hyperthyroidism were present in 1.6% and 1.3% of participants in a community survey, respectively.? A hospital-based study of women in Pondicherry revealed that subclinical and overt hyperthyroidism were present in 0.6% and 1.2% of subjects, respectively. More than one-third of community-detected hyperthyroid cases had positive anti-TPO antibodies, and approximately 39% of these individuals had a goiter.?
Signs and Symptoms of Hyperthyroidism: -
The signs and symptoms of Hyperthyroidism includes-
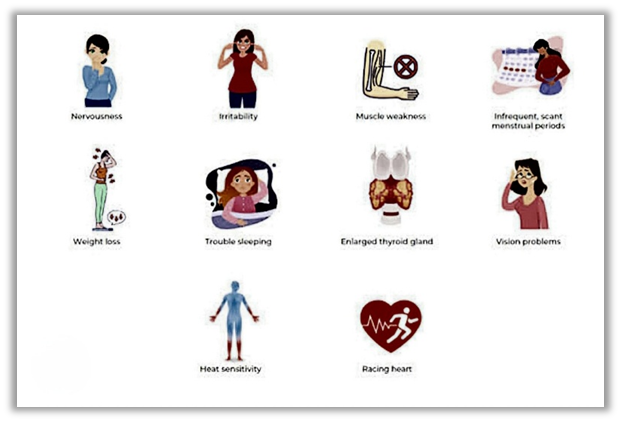
1.Enlarged thyroid gland –
The enlargement of the thyroid gland in hyperthyroidism is due to the increased workload placed on the gland to produce excess thyroid hormones. This overactivity can lead to the growth of thyroid tissue.
2. Intolerance to heat –
As the body’s metabolic rate increases, it produces more heat as a byproduct. This excess heat can make individuals feel warmer than usual.
3. Increased sweating –
The heightened metabolic rate associated with hyperthyroidism is a primary driver of excessive sweating. When thyroid hormones are present in excess, they stimulate various bodily functions, including cellular metabolism and heat production. This increased metabolic activity generates more heat, which the body attempts to dissipate through sweating.
4. Mild to extreme weight loss –
The elevated thyroid hormones stimulate the breakdown of tissues, including muscle and fat, contributing to weight loss.
5. Diarrhea –
Thyroid hormones can stimulate the gastrointestinal tract, leading to increased peristaltic activity and more rapid passage of stool.
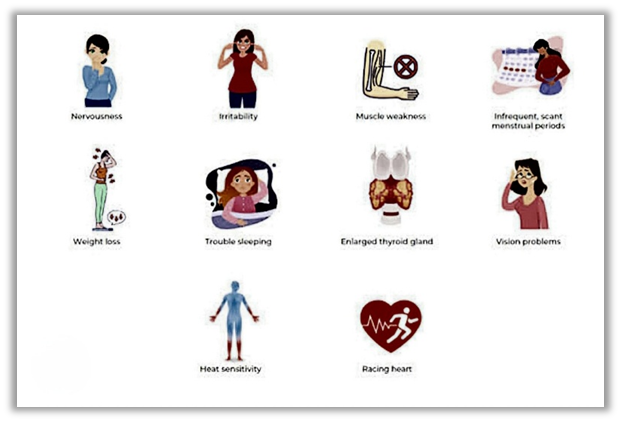
Fig 3 – Signs and Symptoms of Hyperthyroidism
Muscle weakness –
The elevated metabolic rate can cause muscle protein breakdown, leading to muscle wasting and weakness.
Extreme fatigue but inability to sleep –
Excess thyroid hormones can disrupt the body’s natural sleep-wake cycle, making it difficult to fall asleep or stay asleep.
Tremor of the hands -
Hyperthyroidism can lead to heightened activity of the sympathetic nervous system, which controls the body’s “fight-or-flight” response. This increased activity can cause muscle tremors.?
Diagnosis of Hyperthyroidism :-
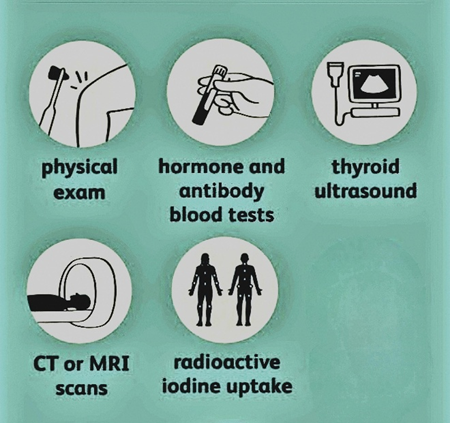
Hyperthyroidism is diagnosed with a medical history, physical exam and blood tests.
I] Medical history and physical exam - The doctor/ physician may check for the following activities –
A) Slight tremor in your fingers and hands.
B) Overactive reflexes.
C) Rapid or irregular pulse.
D) Eye changes.
E) Warm, moist skin.
They can also examine the thyroid gland during swallowing to check if it is larger than usual or bumpy.?
II] Blood tests -
Blood tests that measure the levels of thyroid hormones T3, T4, and thyroid-stimulating hormone (TSH) are essential for diagnosing hyperthyroidism. Elevated T3 and T4 levels in conjunction with a low TSH level are indicative of this condition. It is particularly important to conduct these tests in older adults, as they may not exhibit the typical symptoms of hyperthyroidism.
(The accuracy of thyroid blood tests can be compromised by biotin supplementation. Biotin, a B vitamin commonly found in multivitamins, can interfere with the test results.)?
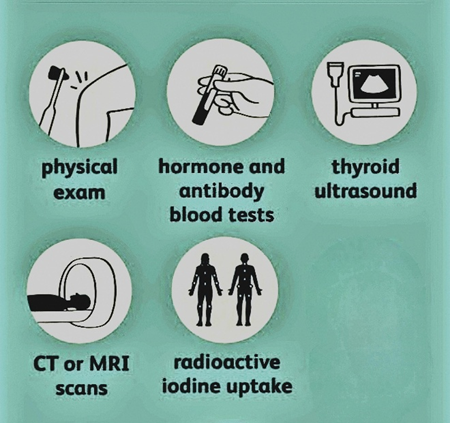
Fig 4 – Diagnosis of Hyperthyroidism
III] Radioiodine Scan and Uptake Test -
A radioiodine scan and uptake test involve administering a small dose of radioactive iodine to assess its accumulation in the thyroid gland. The quantity of radioiodine absorbed by the thyroid gland indicates its hormonal activity. Excessive iodine uptake suggests hyperthyroidism, potentially due to Graves’ disease or overactive thyroid nodules. Conversely, diminished iodine uptake may indicate thyroiditis, where stored thyroid hormones are prematurely released into the bloodstream.
IV] Thyroid Ultrasound -
A thyroid ultrasound employs high-frequency sound waves to generate images of the thyroid gland. This imaging technique excels in detecting thyroid nodules, offering an advantage over other diagnostic methods. As ultrasound does not involve radiation exposure, it is suitable for pregnant or breastfeeding individuals, as well as those who cannot tolerate radioiodine.?1;?
Treatment of Hyperthyroidism :-
A variety of treatments are available for hyperthyroidism. The most suitable approach is determined by individual factors such as age, overall health, the underlying cause of hyperthyroidism, and the severity of the condition.
I] Thyroidectomy –
The most direct treatment for hyperthyroidism is surgical removal of most of the thyroid gland. In general, it is desirable to prepare the patient for surgical removal of the gland before the operation by administering propylthiouracil, usually for several weeks, until the basal metabolic rate of the patient has returned to normal. Then administration of high concentrations of iodides for 1-2 wed immediately before operation causes the gland to recede in size and its blood supply to diminish.
II] Anti-thyroid Medications -
Anti-thyroid medications are employed to alleviate the symptoms of hyperthyroidism by inhibiting the thyroid gland’s production of excessive hormones. Methimazole and propylthiouracil are commonly prescribed medications within this category. Patients typically observe a reduction in symptoms within several weeks to months of initiating treatment.?1;?1;
Methimazole –
Methimazole, a thioamide drug, inhibits thyroid hormone production by blocking the action of thyroid peroxidase (TPO). TPO is an enzyme that catalyzes the iodination and coupling of tyrosine residues in thyroglobulin, leading to the
formation of T4 and T3. Methimazole binds irreversibly to TPO, preventing these reactions and thereby inhibiting thyroid hormones.?1;?2;
Pharmacokinetics of Methimazole –
- Absorption -
Methimazole, a widely used antithyroid medication, exhibits a predictable pharmacokinetic profile. Following oral administration, the drug is rapidly absorbed from the gastrointestinal tract with peak plasma concentrations attained within 1-2 hours. Food intake exerts minimal influence on absorption, allowing for flexible dosing regimens. Methimazole demonstrates a high bioavailability, indicating efficient systemic absorption.
- Distribution -
The drug is minimally bound to plasma proteins, ensuring a high concentration of unbound drug available for therapeutic action. Its low volume of distribution and lipophilic nature facilitate widespread tissue penetration.
- Metabolism -
Hepatic metabolism, primarily mediated by cytochrome P450 enzymes, is the primary route of elimination for methimazole. The drug is converted to its less active metabolite, 4-methyl-5-thiazolecarboxamide, which is subsequently excreted primarily through the kidneys.
- Elimination -
The elimination half-life of methimazole is relatively short, approximately 4-6 hours, necessitating frequent dosing to maintain therapeutic levels. Renal function may influence drug clearance, requiring dosage adjustments in patients with impaired renal function.
Adverse effects of Methimazole:
Nausea, vomiting, rash, itching, fever, joint pain, hair loss, agranulocytosis, hepatotoxicity, teratogenicity, hypothyroidism.?1;?3;
Table 1 – Dosage of some anti-thyroid medications
|
Drug
|
Dosage form
|
Dosage
|
|
Methimazole
|
Tablet
|
5 to 120 mg orally per day (can be given in divided doses)
|
|
Polythiouracil
|
Tablet
|
50 to 300 mg orally after every 8 hours.?1;?
|
III] Radioiodine Therapy -
Radioiodine therapy involves the administration of a radioactive isotope that is selectively absorbed by the thyroid gland. This treatment results in the shrinkage of the thyroid gland and subsequent reduction in thyroid hormone production. Symptoms typically diminish within several months following radioiodine therapy. This treatment often leads to hypothyroidism, a condition characterized by insufficient thyroid hormone production. As a consequence, patients may require long-term thyroid hormone replacement therapy.?1;?1;
REFERENCES
- Hedberg CW, Fishbein DB, Janssen RS, et al. An outbreak of thyrotoxicosis caused by the consumption of bovine thyroid gland in ground beef. N Engl J Med. 1987;316:993–98. [PubMed] [Google Scholar]
- Dr S.B.Bhise and Dr A.V.Yadav, Human Anatomy and Physiology 2, Third edition, Jan 2019, Nirali Prakashan , pg no – 6.7
- Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012;379:1142–54. [PubMed] [Google Scholar]
- Garmendia Madariaga A, Santos Palacios S, Guillén-Grima F, Galofré JC. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clin Endocrinol Metab. 2014;99:923–31. [PubMed] [Google Scholar]
- Desai PM. Disorders of the Thyroid Gland in India. Indian J Pediatr. 1997;64:11–20. [PubMed] [Google Scholar]
- Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H. High prevalence of undetected thyroid disorders in an iodine sufficient adult south Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- Harsh Mohan, A textbook of Pathology, Ninth edition, 2021, Jaypee publication, pg no – 817 & 818
- https://www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659.
- Vaidya B, Pearce SH. Diagnosis and management of thyrotoxicosis. BMJ. 2014;349:g5128. [PubMed] [Google Scholar]
- Bahn Chair RS, Burch HB, Cooper DS, et al.American Thyroid Association and American Association of Clinical Endocrinologists Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593–646. [PubMed] [Google Scholar]
- https://my.clevelandclinic.org/health/diseases/14129-hyperthyroidism
- Abraham P, Acharya S. Current and emerging treatment options for Graves’ hyperthyroidism. Ther Clin Risk Manag. 2010 Feb 02;6:29-40. [PMC free article] [PubMed]
- Jansson R, Lindström B, Dahlberg PA. Pharmacokinetic properties and bioavailability of methimazole. Clin Pharmacokinet. 1985 Sep-Oct;10(5):443-50. [PubMed] [Reference list]
- Abraham P, Avenell A, Park CM, Watson WA, Bevan JS. A systematic review of drug therapy for Graves’ hyperthyroidism. Eur J Endocrinol. 2005;153(4):489-498


 Naman Kishor Gandhi* 1
Naman Kishor Gandhi* 1
 Sneha S Kanase 2
Sneha S Kanase 2
 Tejas S Bagmar 3
Tejas S Bagmar 3
 Aditya D Dhiwar 4
Aditya D Dhiwar 4
 Abhishek A Choughule 5
Abhishek A Choughule 5
 Gaurav P Dhanwade 6
Gaurav P Dhanwade 6
 Ankita C Deokar 7
Ankita C Deokar 7
 Abhishek S Bhosale 8
Abhishek S Bhosale 8
 10.5281/zenodo.14014756
10.5281/zenodo.14014756