Abstract
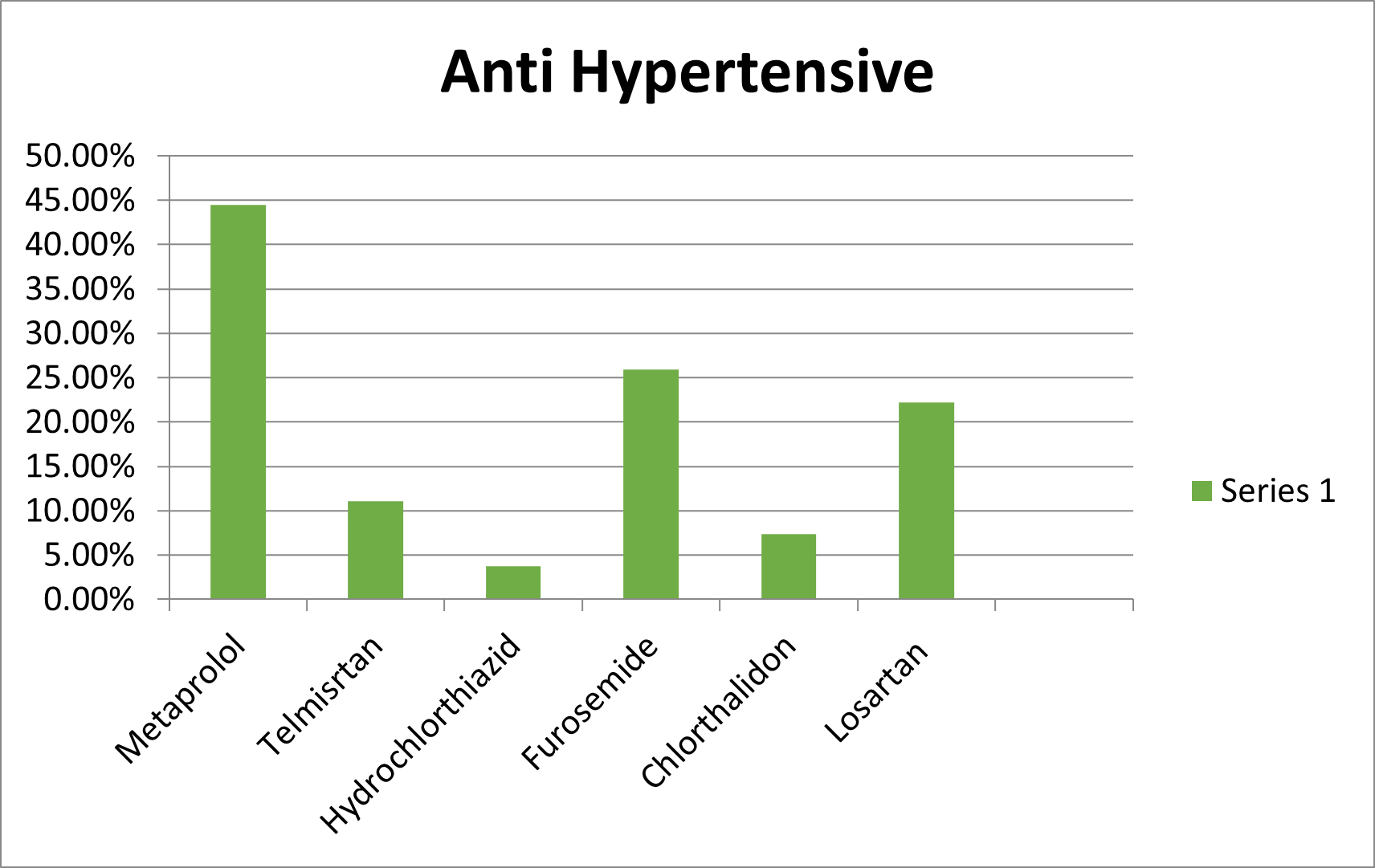
Antihypertensive medications are critical in managing hypertension, a prevalent and potentially life-threatening condition. However, the benefits of these medications can be offset by adverse drug reactions (ADRs), which can significantly affect patient compliance, quality of life, and overall treatment outcomes. This study aims to investigate the incidence, types, and severity of ADRs associated with antihypertensive drugs in a hospital setting, contributing to pharmacovigilance efforts and enhancing patient safety. The survey was conducted on 108 patients. Their mean age is 55.14 years, and the male majority is 66%. Most of the study participants lived in urban areas and were married. The number of anti-hypertensive medications used by patients ranges from one to six. Metaprolol was the most commonly prescribed medication, followed by furosemide and losartan. Nearly one-third of patients had poor adherence (< 80%) to their antihypertensive medications. Forgetfulness (25.9%) and fasting (9.2%) were the two most commonly mentioned reasons for poor adherence. Among the reported adverse effects, an increase in urination ranked highest, affecting 22.22% of patients.
Keywords
Antihypertensive medications, adverse drug reactions, pharmacovigilance, hypertension, hospital survey, patient safety.
Introduction
Pharmacovigilance:
Any medical intervention that seeks to improve patient safety by evaluating the risk-benefit profile of medications must include pharmacovigilance [1]. "The science and activities related to the detection, assessment, understanding and prevention of adverse drug effects toxicity or any other possible drug related problems" is how the World Health Organization defines it. [2]. The National Pharmacovigilance Programme for Ayurvedic, Siddha, and Unani Drugs was launched in 2008 by the Department of AYUSH, Ministry of Health and Family Welfare, Government of India, in recognition of the importance of this field [3]. The Central Sector initiative for promoting "Pharmacovigilance of Ayurveda, Siddha, Unani, and Homoeopathy (ASU&H) drugs" was reintroduced in 2018 by the Ministry of AYUSH, Govt. of India, with the inclusion of Homoeopathy [4]. The Institute for Post Graduate Teaching and Research in Ayurveda (IPGT& RA), Jamnagar, a constituent institute of Gujarat Ayurved University and the first institute of its kind dedicated to Ayurvedic Education and Research, launched a national program in 2008 to monitor the safety of Ayurveda Siddha and Unani (ASU) drugs. The national government of Gujarat has given conditional approval to 24 Ayurvedic institutes in total to accept students for Ayurvedic studies for the current academic year 2021–2022 [5].
Anti-Hypertensive Drugs:
In both developed and emerging economies, hypertension is a significant public health concern. It is estimated that 1.5 million fatalities in India occur each year as a result of cardiovascular diseases (CVDs) [6]. Due to demographic shifts, emerging nations are disproportionately seeing an increase in the prevalence of hypertension, a key risk factor for CVDs that includes stroke and myocardial infarction [7]. There are several published national and international guidelines available for the management of hypertension. Diuretics are advised as the first-line treatment for hypertension in the JNC 7 guideline [8]. On the other hand, the European guideline recommends using any of the five antihypertensive classes as first-line treatment unless there is a particular justification [9]. Numerous symptoms and adverse effects, including fatigue, mood swings, disturbed sleep, dry mouth, blurred vision, and impotence, are linked to antihypertensive medication [10, 11]. The success of the therapeutic regimen in the treatment of hypertensives is significantly influenced by side effects and the patient's perception of them. According to certain research, individuals even find that taking their hypertension medicine causes them more anxiety than their ostensibly asymptomatic condition [12, 13], However, some research has shown that antihypertensive drugs enhance quality of life connected to health [14, 15]. Unpleasant side effects from medications might cause noncompliance and negatively impact quality of life in relation to health [16]. Lowering blood pressure (BP) is the primary objective of antihypertensive medication therapy in order to minimize renal and cardiovascular morbidity and mortality. Patients should be urged to follow the recommended pharmacologic and non-pharmacologic therapy techniques in order to accomplish this goal [17]. Poor adherence to antihypertensive medications and persistently elevated blood pressure may be responsible for a significant portion of cardiovascular events, including angina, myocardial infarction, chronic heart failure, kidney failure, transient cerebral ischemic attacks and strokes, premature mortality and disability, and increased hospitalization costs [18–21]. Conversely, hypertension patients who report rigorous adherence to recommended pharmaceutical therapy have considerably lower systolic and diastolic blood pressure than those who disclose even a small slip-up in taking their antihypertensive drugs [22, 23].
Traditional Therapy of Hypertension
Alkalyting Agent:
The first family of anticancer drugs, known as alkylating agents, originated from sulfur mustard gas, which was deployed in World War I [24, 25]. Alkylating drugs are utilized in myeloablative conditioning regimens before hematopoietic stem cell transplants, as well as in the treatment of solid tumors and leukemias [26]. The primary cause of their harmful action is DNA alkylation, which obstructs transcription and DNA replication [24]. Because alkylating drugs are virtually often taken in conjunction with other anti-cancer medications, the exact relationship between them and the development of hypertension is unclear. 36% of individuals in early clinical trials utilizing busulfan and cyclophosphamide for myeloablative conditioning experienced any grade hypertension, and 7% experienced grade 3/4 hypertension [27]. Only a few numbers of later research have verified this discovery or even mentioned hypertension as a frequent side effect. Alterations in sodium homeostasis, endothelial damage, decreased VEGF circulation, and renal injury are among the potential mechanisms of hypertension with alkylating drugs [28–30].
Anthracyclines:
Doxorubicin is one of the anthracyclines that works well against a variety of solid tumors and hematologic malignancies by inhibiting topoisomerase 2, which in turn stops DNA replication. Despite the lack of evidence linking anthracyclines to hypertension, it is crucial to monitor and maintain normal blood pressure before, during, and after therapy, as individuals with hypertension are more likely to have cardiac damage [31]. Fascinatingly, beta-blockers and RAS inhibitors prevent cardiotoxicity in hypertensive patients using anthracyclines, according to clinical research. It's unclear if there's a direct impact on cardiac myocytes or if this is only because of the antihypertensive effect [32].
METHOD:
The Study was conduct from 29 Feb to 2 May, at four hospitals Farate Multispecialty Clinic, Alshifa Clinic, Shinde Clinic and Sadunkhe Clinic of Maharashtra in Kolhapur city. Kolhapur is a historical part of Maharashtra India, 1634 km from the capital city of New Delhi.
RESULT:
A total of 108 patients were included in the final analysis with a mean age of 55.14 years and a male majority (66%). Most of the study participants lived in urban areas and were married. The number of antihypertensive medications used by patient’s ranges from one to seven.Nearly one-third of the study participants also used additional medications for the management of other chronic conditions. [Table 1] Metaprolol was the most commonly prescribed -medication, followed by Furosemide and Losartan [Fig 1]. The median (minimum-maximum) daily doses of HCT, enalapril, amlodipine, and nifedipine were 25 mg (12.5–50), 5mg (2.5–20), 5 mg [33,34] and 20mg (5–40), respectively.
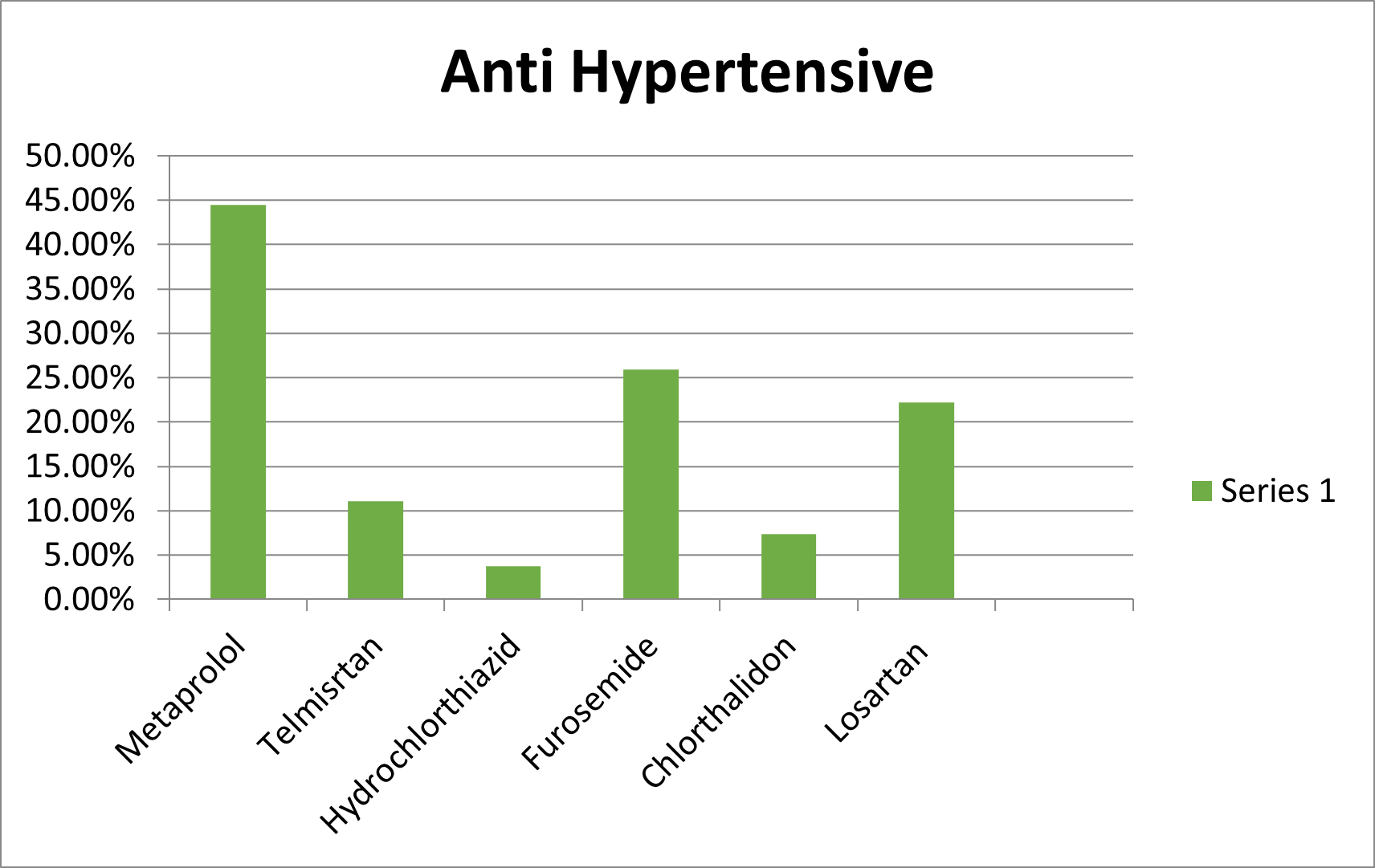
Figure 1: Anti-Hypertensive Drug Prescribed by Doctors
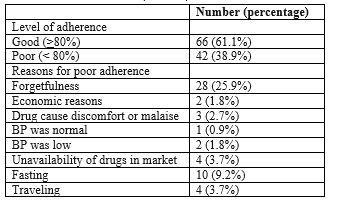
Nearly one-third of patients had poor adherence (< 80>
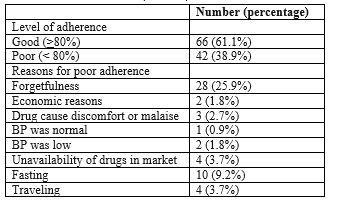
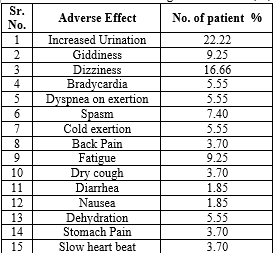
Table 1: Number Patient having adverse effect (%)
Among the reported adverse effects, an increase in urination ranked highest, affecting 22.22% of patients. This symptom, often associated with diuretic medications, underscores the importance of fluid balance management in medication regimens.Giddiness, another prevalent adverse effect, was reported by 9.25% of patients, highlighting the impact of medications on balance and sensory perception. Similarly, dizziness affected 16.66% of individuals, indicating a significant concern regarding medication tolerability and potential impacts on daily activities.Bradycardia, a condition characterized by a slower-than-normal heart rate, was experienced by 5.55% of patients. Such cardiovascular effects underscore the need for careful monitoring and adjustment of medication dosages to avoid adverse outcomes.Other reported adverse effects included dyspnea on exertion (5.55%), muscle spasms (7.40%), and cold extremities (5.55%), reflecting the diverse physiological responses to medication therapies.Fatigue, dry cough, stomach pain, and back pain were also reported, albeit at lower frequencies (ranging from 3.70% to 9.25%). These symptoms can significantly impact quality of life and may necessitate adjustments in treatment plans to minimize discomfort and enhance patient adherence.Understanding and addressing adverse effects are crucial aspects of patient care, requiring healthcare providers to balance therapeutic benefits with potential risks. Patient education, close monitoring, and collaborative decision-making between patients and healthcare professionals are essential for mitigating adverse effects and optimizing treatment outcomes [Table 1].
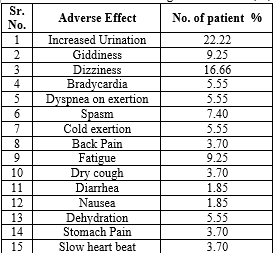
Table 2:Adherence to antihypertensive medications among hypertensive patients attending UOGCSH (N = 108)
Among patients prescribed antihypertensive medications, a range of factors influencing adherence emerged, providing valuable insights into patient behaviors and challenges in medication management.Forgetfulness emerged as the primary reason for non-adherence, affecting 25.9% of patients. This highlights the importance of implementing strategies such as medication reminders or pill organizers to help patients stay on track with their treatment regimen.Economic reasons were cited by a smaller proportion of patients (1.8%), indicating that financial constraints may pose a barrier to medication adherence for some individuals. This underscores the need for affordable healthcare options and support programs to ensure access to essential medications.Discomfort or malaise caused by the drugs themselves contributed to non-adherence in 2.7% of cases. This highlights the importance of patient-provider communication to address and manage medication side effects effectively.Interestingly, a small percentage of patients reported non-adherence because their blood pressure was either normal (0.9%) or low (1.8%). This suggests a misunderstanding or lack of awareness regarding the importance of continued medication adherence for long-term health maintenance, even when blood pressure appears to be under control.The unavailability of drugs in the market was cited by 3.7% of patients, indicating potential supply chain issues that can disrupt medication access and adherence. Efforts to ensure consistent availability of essential medications are crucial for supporting patient adherence and continuity of care.Other factors contributing to non-adherence included fasting (9.2%) and traveling (3.7%), highlighting the challenges patients may face in maintaining their medication schedule during lifestyle disruptions.
CONCLUSION:
The comprehensive analysis of antihypertensive medication adherence, adverse effects, and influencing factors provides valuable insights into the complex landscape of hypertension management. With a considerable portion of patients exhibiting poor adherence to their medication regimens, it's evident that addressing barriers such as forgetfulness, economic constraints, and medication side effects is essential for optimizing treatment outcomes.The prevalence of adverse effects underscores the importance of vigilant monitoring and proactive management to mitigate potential risks and enhance patient comfort. Furthermore, the diverse range of reported adverse effects highlights the need for personalized approaches to medication selection and dosage adjustment to minimize discomfort and improve adherence.Efforts to enhance patient education, promote medication adherence strategies, and address socioeconomic barriers are crucial for empowering patients to take an active role in managing their hypertension effectively. Collaborative decision-making between healthcare providers and patients is essential for navigating treatment complexities and ensuring patient-centered care.Moving forward, a holistic approach to hypertension management that considers patient preferences, lifestyle factors, and individualized treatment goals is paramount. By addressing adherence challenges and optimizing medication regimens, healthcare providers can strive towards improving patient outcomes and reducing the burden of hypertension-related complications in the long term.
REFERENCE:
- WHO, 2002a. The importance of pharmacovigilance – Safety monitoring of medicinal products. UK. Available from: http://apps.who.int/medicinedocs/pdf/s4893e/s4893e. pdf?ua=1. [Last accessed on 2020 Nov 28].
- Hadi MA, Neoh CF, Zin RM, Elrggal ME, Cheema E. Pharmacovigilance: Pharmacists’ perspective on spontaneous adverse drug reaction reporting. Integr Pharm Res Pract2017;6:91–8.
- Galib, Acharya R. National Pharmacovigilance Programme for Ayurveda, Siddha and Unani Drugs. AYU 2008;29:195 200.
- Ayushsuraksha. Pharmacovigilance of Ayurveda, Siddha, Unani & Homoeopathy (ASU & H) drugs. Available from: https://www.ayushsuraksha.com/. [Last accessed on 2021 May 13].
- Ccim. Central Council of Indian Medicine. Available from: https://www.ccimindia.org/colleges ayurveda.php. [Last accessed on 2021 May 13].
- Gaziano T, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Cardiovascular disease. In: Jamison DT, Mosley WH, editors. Disease control priorities in the developing world. Oxford: Oxford University Press; 2006. p. 645-62.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005;365:217- 23.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. The JNC 7 report. JAMA 2003;289:2560-72.
- Mancia G, Backer GD, Dominiczak A, Cifkova R, Fagard R, Germano G et al. "2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the management of arterial hypertension". Eur Heart J. 2007;28:1462-1536.
- Schoenberger JA, Croog SH, Sudiovsky A, Levine S, Baume RM. Self-reported side effects from antihypertensive drugs. AJH 1990; 3: 123–32.
- Hansson L. The BBB study: the effect of intensi. Ed antihypertensive treatment on the level of blood pressure, side effects, morbidity and mortality in “well-treated” hypertensive patients. Blood Press 1994; 3: 248–54.
- Croog SH, Levine S, Testa MA, et al. The effects of antihypertensive therapy on the quality of life. N Engl J Med 1986; 314: 1657–64.
- Battersby C, Hartley K, Fletcher A, et al. Quality of life in treated hypertension: a case–control community based study. J Hum Hypertens 1995; 9: 981–86.
- Neaton JD, Grimm RH, Prineas R, et al. Treatment of mild hypertension study. Final results. JAMA 1993; 270: 713–24.
- Wiklund I, Halling K, Ryde’n-Bergsten T, Fletcher Aon behalf of the HOT Study Group. Does lowering the blood
- pressure improve mood? Quality-of-life results from the Hypertension Optimal Treatment (HOT) study. Blood Press 1997; 6: 357–64.
- Curb JD, Borhani NO, Blaszkowski TP, Zimbaldi N. Longterm surveillance for adverse effects of antihypertensive drugs. JAMA 1985; 253: 3263–68.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–71.
- Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, Moore C, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–8.
- Dragomir A, Côté R, Roy L, Blais L, Lalonde L, Bérard A, et al. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Med Care. 2010;48(5):418–25.
- World Health Organization. Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk. 2007 Available from: http://apps.who.int/iris/bitstream/handle/10665/43685/9789241547178_eng.pdf;jsessionid=26CDD2C8C638CCBD9CD27371D22A1F3C?sequence=1. [Cited 4 August 2017]
- World Health Organization. A global brief on hypertension: silent killer, global public health crisis. 2013. Available from: https://www.who.int/cardiovascularr_diseases/publications/global_brief_hypertension/en/. [Cited 4 August 2017
- Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol. 2013;4:91.
- Shin S, Song H, Oh S-K, Choi KE, Kim H, Jang S. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res. 2013;36(11):1000–5.
- 24.Puyo S, Montaudon D and Pourquier P. From old alkylating agents to new minor groove binders. Crit Rev OncolHematol2014; 89: 43–61.
- Eastman A. Alkylating and platinum-based agents. Curr Opin Oncol 1990; 2: 1109–1114.
- Abi Aad S, Pierce M, Barmaimon G, et al. Hypertension induced by chemotherapeutic and immunosuppressive agents: a new challenge. Crit Rev Oncol Hematol2015; 93: 28–35.
- FDA. NDA 20-954 Busulfex (busulfan) Injection. 1999. Berendes E, Cullen P, Van Aken H, et al. Endogenous glycosides in critically ill patients. Crit Care Med 2003; 31: 1331–1337.
- Graves SW, Eder JP, Schryber SM, et al. Endogenous digoxin-like immunoreactive factor and digitalis-like factorassociated with the hypertension of patients receiving multiple alkylating agents as part of autologous bone marrow transplantation. Clin Sci (Lond) 1989; 77: 501–507.
- Knijnenburg SL, Jaspers MW, van der Pal HJ, et al. Renal dysfunction and elevated blood pressure in long-term childhood cancer survivors. Clin J Am Soc Nephrol 2012; 7: 1416–1427.
- Hassen LJ, Lenihan DJ and Baliga RR. Hypertension in the Cardio-Oncology Clinic. Heart Fail Clin 2019; 15: 487–495.
- Geisberg CA and Sawyer DB. Mechanisms of anthracycline cardiotoxicity and strategies to decrease cardiac damage.Curr Hypertens Rep 2010; 12: 404–410.
- World Health Organization. A global brief on hypertension: silent killer, global public health crisis. 2013. Available from: https://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/. [Cited 4 August 2017]
- Saunders E, Weir MR, Kong BW, Hollifield J, Gray J, Vertes V, et al. A comparison of the efficacy and safety of a ?-blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med. 1990;150(8):1707–13


 Sonal Kumbhar *
Sonal Kumbhar *
 Ayan Noushad Sayyad
Ayan Noushad Sayyad
 10.5281/zenodo.12657664
10.5281/zenodo.12657664