Abstract
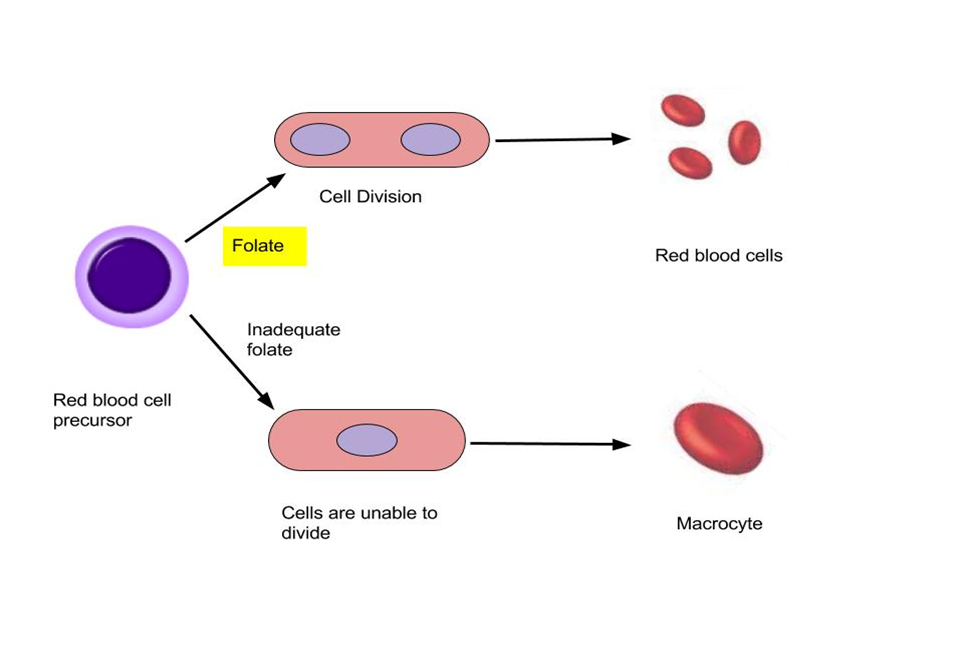
The use of resealed erythrocytes as drug carriers has emerged as a promising strategy in drug delivery systems, offering unique advantages in terms of drug targeting, prolonged circulation time, and reduced side effects. This comprehensive review explores the various aspects of resealed erythrocytes as drug carriers, with a focus on their application in targeted drug delivery. To overcome drawbacks of conventional drug delivery system, modern drug delivery approach such as resealed erythrocytes can be a potential delivery system. Resealed RBC's are biodegradable, biocompatible and have prolonged life cycle. A number of mammalian RBC’s are being utilized in drug encapsulation and resealing for their utilization in enzyme and drug delivery. Resealed erythrocytes can be used for drug targeting, carrier for drug, enzyme, macromolecules and proteins. For getting drug loaded erythrocytes collect the sample of blood, then separate erythrocyte from plasma; then loading of drug into erythrocyte and the resulted drug loaded erythrocytes resealed. There are different methods of drug loading such as dialysis method, dilution method, endocytosis method etc. The survival time of RBC is dependent on the shape, size, senescent cells antigen, surface charge and haemoglobin content lost at the time of loading. The survival time decide their entrapment efficiency. Resealed RBC's have potential treatment in hepatic tumour, parasitic disease, removal of toxic agents, replacement therapy, oxygen deficiency therapy. Therefore, resealed can be better delivery method for target drug delivery.
Keywords
Resealed erythrocytes, Drug targeting, Drug delivery systems, Erythrocyte carriers, Biocompatibility, Erythrocyte encapsulation, Controlled release, Pharmacokinetics.
Introduction
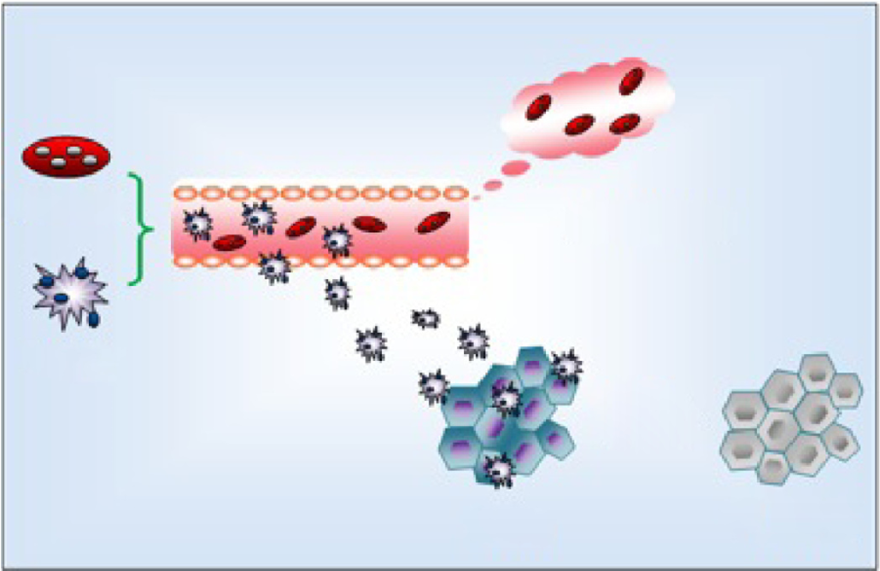
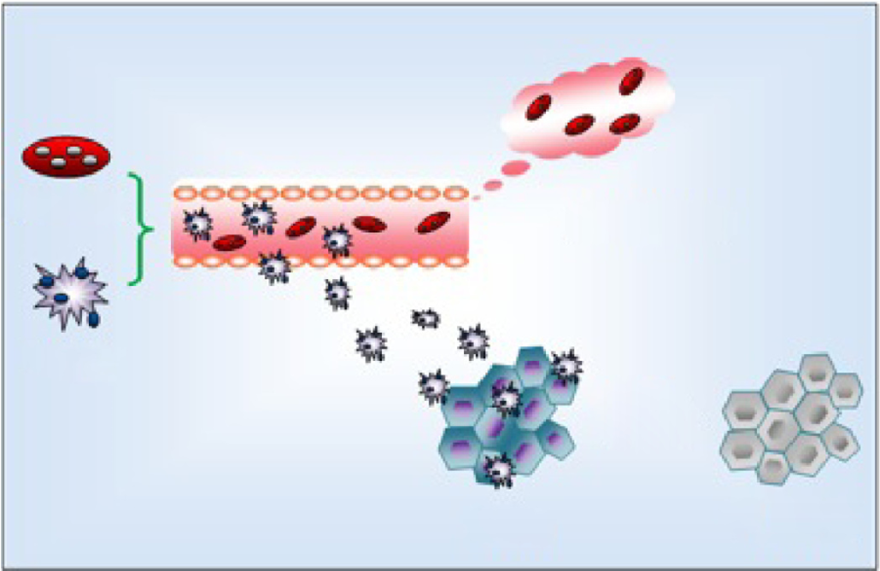
Erythrocytes have been exploited extensively for their potential applications as drug delivering microspheres. These carriers offer some unique characteristics such as excellent biocompatibility and biodegradability as well as considerably long life-span in circulation. Generally, “carrier erythrocytes” are prepared by collecting some blood samples from the organism of interest, separation of erythrocytes from plasma and leukocytes, entrapment of the drug in the erythrocytes, and finally resealing the resulting cellular carriers [1]. Upon reinjection to the same organism, these drugloaded microsphere can serve as the intravenous slow release carriers and/or target the drug to the reticuloendothelial system (RES). In this article, some biological aspects of the erythrocytes, methods of preparation, in vitro and in vivo characteristics, and therapeutic applications of the carrier erythrocytes are reviewed. [2].
History:
For the first time, erythrocytes were described in samples of human blood by Dutch scientist Lee Van Hock in 1674. About hundred years later, Howson found that these cells are flat discs rather than the globules described by Van Hock, and in the 19th century, Hope Seyler identified hemoglobin and its crucial role in oxygen delivery to different tissues. The first efforts for entrapment of chemicals in erythrocytes were made in 1953 by Gardos, who tried to load the “erythrocyte ghosts” by ATP [3]. In 1959, Marsden and Ostling reported the entrapment of dextrans with molecular weights of 10 to 250 KD in erythrocyte ghosts [4]. Fourteen years later, the first reports on loading the erythrocyte ghosts by therapeutic agents for delivery purposes were published independently by Ihler et al. And Zimmerman [5]. And the term “carrier erythrocytes” was used for the first time in 1979 to describe the drug-loaded erythrocytes [6].
Various carriers has been used for the drug targeting among which cellular carrier offer a greater potential advantages related to its biodegradability, non-pathogenicity, nonimmunogenicity, biocompatibility, selfdegradability along with high drug loading efficiency. Leukocytes, platelets and erythrocytes have been proposed as cellular carrier systems [7].
Basic Features Of Erythrocytes:
A healthy adult male and female has about 5.4 million RBC per µL of blood and 4.8 million RBC per µL of blood respectively. Erythrocytes are biconcave discs with a diameter of 7-8 µm. They contain the O2 carrying protein Hb, which is a pigment that gives whole blood red colour. Erythrocytes are highly specialized for their O2-CO2-transport function. Matured mammalian erythrocytes are devoid of nucleus so all their space is available for O2 transport, moreover erythrocytes lacks mitochondria and generates ATP anaerobically. Erythrocytes live only for 120 days because of the wear and tear that their plasma membrane undergoes as they squeeze through blood capillaries. In some species the removal of erythrocytes from circulation occurs randomly, and in others, old erythrocytes are selectively removed (largely in spleen) by the action of phagocytotic cells which recognize old erythrocytes on the basis of senescent cell antigen. Physiologic removal of old and damaged erythrocytes is initiated by the appearance of an aging antigen that marks them for death by initiating the binding of IgG autoantibody and subsequent removal by phagocytes [8].
Characterization Of Red Blood Cell-Derived Particles:
RBC-derived particles exhibit prolonged circulation time, and can readily evade the phagocytic clearance in the biological environment, due to the retention of RBC membrane proteins and their specialized chemical structure. Besides, the physical characteristics of the RBC-derived particles, the biochemical parameters are also very significant for evaluation of the particle systems. The mechanical characterization of the RBCderived systems needs further exploration, though.
Sources And Isolation Of Erythrocytes:
· Blood is collected into heparin zed tubes by venipunture
· Blood is withdrawn from cardiac/splenic puncture (in small animal) and through veins (in large animals) in a syringe containing a drop of anti-coagulant.
· The whole blood is centrifuged at 2500 rpm for 5 min. at 4 ±1 0 C in a refrigerated centrifuge.
· The serum and buffy coats are carefully removed and packed cells washed three times with phosphate buffer saline (pH=7.4).
· The washed erythrocytes are diluted with PBS and stored at 4oC until used.
· Various types of mammalian erythrocytes have been used for drug delivery, including erythrocytes of mice, cattle, pigs, dogs, sheep, goats, monkeys, chicken, rats, and rabbits. To isolate erythrocytes, blood is collected in heparinized tubes by venipunture. Fresh whole blood is typically used for loading purposes because the encapsulation efficiency of the erythrocytes isolated from fresh blood is higher than that of the aged blood. Fresh whole blood is the blood that is collected and immediately chilled to 4 C and stored for less than two days. The erythrocytes are then harvested and washed by centrifugation. The washed cells are suspended in buffer solutions at various hematocrit values as desired and are often stored in acid– citrate–dextrose buffer at 4 0C for as long as 48 h before use. Jain and Vyas have described a well-established protocol for the isolation of erythrocytes [9]. Erythrocyte ghost can be used as adenosine triphosphate (ATP). Entrapment of dextran (molecular weight 10–250 k Da) and loading of drugs in erythrocytes was reported separately.
· Their biocompatibility, particularly when autologous cells are used, hence no possibility of triggered immune response [10].
Requirements For Encapsulation
Wide varieties of biologically active substances are encapsulated in erythrocytes: Generally, they should be polar or hydrophilic but non-polar molecules have also been successfully encapsulated in their respective salt form. (E.g. Adriamycin dipropionate salt can be entrapped in bovine erythrocytes) [11]. Molecules, which interfere with the membrane and cause deleterious effect on membrane structure, are not considered to be appropriate for encapsulation. E.g. Daunomycin. The molecule should neither interfere with the membrane transport system nor with glycolysis within the erythrocytes [12].
I] Different methods of drug loading:
These methods have been employed for drug loading in erythrocytes:
1.Elecron-insertion/Electro encapsulation method
2. Hypo-osmotic lysis method
a) Dialysis method
b) Dilution method
c) Isotonic osmotic lysis method
d) Preswell method
3. Membrane perturbation Method
4. Endocytosis method
5. Lipid fusion method
1 Electro-insertion / electro encapsulation method:
In 1973, Zimmermann develop an electric pulse technique (electroporation) for encapsulation of bioactive substances [13]. The technique utilize electric shock by bringing irreversible alternation in RBC’s membrane. Kinosita and Tsog utilize transient electrolysis. The RBC membrane opened by dielectric breakdown. Then resealed pore through incubation at 37OC in buffer. This technique depends on the difference in potential across the membrane which is created directly by using intra and intercellular electrode and indirectly by application of electric field to cells. The formation of pores takes place after breaking of RBC through electro chemical compression. This depends on ionic strength of medium pulse duration and strength of uniform loading of cells as compared to osmotic technique [14]. But there is need of speed of instrument and also sophisticated process. The entrapment efficiency is about 35%. The examples of compounds entrapped by this method are urease and sucrose [15].
2. Hypo-osmotic lysis method:
This method depends on the ability of RBC’s toplacedin isotonic saline solution. The exchange of intracellular and extracellular RBC’s takes place through resealing and lead to osmotic lysis. Finally drug encapsulated in RBC.
a) Dialysis Method:
Klibansky utilize this technique for the entrapment of proteins then modified by Jarde First a suitable hematocrit is made by making a mixer of drug and RBC suspension which is then collected in dialysis tubes. The inner side volume is inflated by using airbubble and then sealed so that the suspension of RBC cover only 75% of inner side volume. The role of air bubble is very critical. The dialysis tubes are placed in bottle containing swelling solution (100ml) for desired lysis and shaked for their proper mixing at 4OC. After that dialysis tube placed in resealing solution (100ml) at 20-30o C, then give washing to loaded RBC by cold phosphate buffer solution at 4OC. then again resuspended in phosphate buffer solution. This method has entrapment efficiency 30-50% and recovery percentage is 70-80% [16].
b) Dilution Method:
In it RBC placed in 0.4% Nacl (hypotonic solution) which lead to their rupturing and allow escaping of cellular contents then swelling of cells takes place. (i.e. 6 times of their original weight). This swelling allows the formation of pores having diameter 200-500Å [17]. For equilibrium of intracellular and extracellular concentration treat 1 volume of RBC with 2-20 volume of solution for allowing their loading in hypotonic solution at 0O C for 5 minutes. Tonicity of solution can be resorted by mixing hypertonic solution [18]. This method is used for low molecular weightt drugs rapidly. It has very low entrapment efficiency i.e. 1-8%. Dilution method is applicable for enzymes like arginase asparaginase, ?-galactosidase, ?-glucosidase, and bronchodialotors like sulbutanol [19].
c) Isotonic osmotic lysis method:
This method depends on the transient RBC membrane permeability and utilize polyethylene glycol Diffusion of biologically active drug maintain equilibrium inside the environment . RBC are incubated under isotonic solution then resealed the equilibrated RBC’s. This method is applicable for very small molecules and utilize urea solution, polyethylene glycol and ammonium chloride for isotonic osmotic lysis [20].
d) Preswell method
Rechesteiner [45] used this method firstly and then modifications performed by pitt et al [46] This include the principle swelling of RBC in slightly hypotonic solution. Swollen cells recoverd by using centrifution then aqueous solution of drug is added in small amount until lysis takes places. The swelling of cells takes places slowly which result in best retention of cellular content. This method is simple and form RBC carrier ith best life lifespan in vivo. This method is applicable to insulin [21]. levothyroxine, asparaginase cyclophosphate propanolol, metronidazole, isoniazide, methotrexate.
3) Membrane perturbation method
This method is used by Hattori and ketao for entrapment of daunomycin in human RBC and mouse RBC. The permeability of RBC membrane is initiated on exposure to amphotericin B [22]
4) Endocytosis method
Schrier et al explain the endocytosis is method for entrapment of drug in RBC carrier 1 volume of RBC is placed in 9 volume of buffer (2.5m MATP,1mm CaCl2, 2.5mm MgCl2) then incubated at 25OC for 2 minute. Creation of pores they are resealed by use of 154mm Nacl then incubated at 37O C for 2 minutes. The endocytosed material separated from cytoplasm by vesicle membrane and prevent it from RBC and vice versa. This method is applicable for entrapment of drugs like vitamin A, chloropromazine, primaquine, phenothiazine, tetracaine, hydrocortisone and vinblastine [19].
5) Lipid fusion method
Drug entrapped in vesicular lipid carrier mixed with human RBC and human result in exchange of encapsulated drug. Gresoneleand Nicholau applied this method for entrapment of inositol monophosphate for [19]
J] In vivo characterization of resealed RBC:
The characterstics of resealed RBC depends on following parameters: -
1. Physical characterisation:
Surface and Shape Morphology: The shape is examined by comparing the ghost RBC untreated RBC for this Scanning electron microscope, TEM is used for this purpose.
Drug Release: Drug release is calculated by diffusion and dialysis method.
Percentage encapsulation of drug content: First, by using acetonitrile/ methanol, membrane of loaded RBC are deproteinized. Then centrifused at 3000 rpm. The clear supernatant is used for calculation of drug content.
Electrical surface potential and surface pH: Surface pH and electrical surface potential is calculated by use of pH sensitive probes and zeta potential measurements.
2. Cellular characterisation:
In vitro haemoglobin content and release of drug
From drug loaded cells, haemoglobin and in vitro release of drug can be estimated. Cell suspension (5% hematocrit in phosphate buffer solution) are stored in ambered colour glass container at 4O C and observed for haemoglobin drug content.
It can be estimated by by “counting the number of intact cells per cubic mm of packed erythrocytes”. The equipment used for this technique is Neubeur’s chamber and Hematological analyser.
It is estimated by calculating the resistance of erythrocytes uptohemolysis after exposing a step wise dilute saline solution.
After dilution of RBC suspension with distilled water, centrifuged for 15 min at 3000 rpm. The resulted clear supernatant is measured by drug and HB content in using spectrophoto meter.
It is estimated when cell suspension is passed through hypodermic needle (10ml/min) for calculation of drug and Hb content
- ESR (Erythrocyte sedimentation rate)
It is estimated by using ESR apparatus by determining the stability of suspension in plasma. It depends on relatives concentration of plasma proteins number and size of RBC
3.Biological Characterisation:
It involves sterility testing in which testing of pyrogens is carried out by checking response for rabbit fever or LAL i.e limulus amoebocytes lysate and animal toxicity test [19].
K] RELEASE MECHANISMS:
The various mechanisms proposed for drug release include [23,24]:
- Passive diffusion
- Specialized membrane associated carrier transport
- Phagocytosis of resealed cells with senescent antigen by macrophages of RES, subsequent accumulation of drug into the macrophage interior, followed by slow release
Accumulation of erythrocytes in lymph nodes upon subcutaneous administration followed by hemolysis to release the drug.
IMMUNOLOGICAL CONSIDERATION
- The immunological characterization of a drug carrier is of two types:
- The immunogenisity of the carrier itself
- The ability of the carrier to protect an entrapped drug from immunological detection.
The autologous erythrocytes are not immunogenic. However, there is concern that the lysis procedure utilized for drug entrapment might elicit some cryptic antigens [25,26,27].
Drug-Loaded Erythrocytes As A Slow-Release System:
The use of erythrocytes as a controlled release of drug is predominantly devoted to small molecules that are minimally retained within erythrocytes and progressively leak from the cell into the plasmatic compartment. The major problem with the slow release is that once encapsulation is performed, the molecule may escape rapidly. To address this problem, Magnani et al patented a procedure that retains small drugs within the intra-erythrocytic compartment by means of high affinity intracellular components [28]. Immunophilin proteins that noncovalently bind to immunosuppressive drugs are entrapped within erythrocytes to increase drug retention [29]. Although clever and suitable for industrial application, this method is restricted to molecules that are ligands of proteins. Another possibility is to encapsulate a prodrug that will be progressively cleaved by intraerythrocytic enzymes to deliver the active drug. This method has been successfully applied to the entrapment of dexamethasone-21-phosphate, the active drug (dexamethasone) being released after the removal of the phosphate group by intraerythrocytic esterases. For other drug classes, researchers have resorted to crosslinking agents such as glutaraldehyde (GA) and bis(sulfosuccinimidyl) suberate (BS3) to rigidify the erythrocyte membrane and reduce leakage [30,31]. The resulting chemically modified erythrocytes present a marked decrease in deformability and membrane fluidity. This membrane alteration reduces erythrocyte biocompatibility and leads to their rapid elimination by the monocyte–macrophage system of the spleen [32]. Thus, the employment of crosslinkers to induce “slow drug release” is not recommended for clinical use. Recently, the coating of loaded erythrocytes with biocompatible polyelectrolytes (polyl-lysine hydrobromide and dextran sulfate.) has been explored to counterbalance the inability of erythrocytes to control protein and drug release. It was demonstrated that adjusting the number of polyelectrolyte layers could regulate the release profile of the encapsulated protein. However, the industrial feasibility of polyelectrolyte layers may be an issue [33].
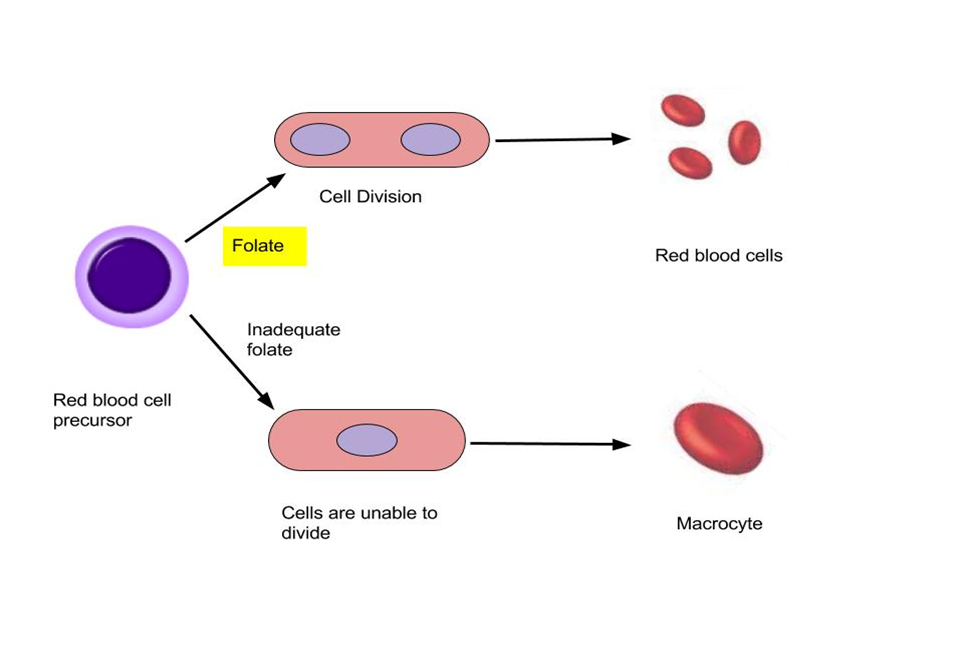
Life-Span:
The survival time of the carrier erythrocytes in circulation upon re-injection is one of the most important factors influencing the in vivo drug delivering efficacy of these cellular carriers. It is obvious that if the purpose of drug delivery is prolonged drug release in circulation, the longer life-span is desired and, contrarily, if the goal of drug encapsulation in erythrocyte is targeting to RES, the rapid phagocytosis of carrier cells (shorter lifetime) is preferred. The life-span of the carrier erythrocytes in circulation depends on the size, shape, surface electrical charge, and the extent of the loss of hemoglobin and the other cell constituents during the loading procedure. Different methods to determine the carrier erythrocytes’ lifetime in circulation include labeling the carrier cells by Cr51 or the fluorescence markers such as fluorescein isothiocyanate (FITC) and encapsulation of C14-containing sucrose or gentamicin [59]. The last two compounds remain within the erythrocytes during its entire lifetime and consequently their extracellular concentration in plasma can be used as a measure of the carrier cell lysis. In general, the disappearance of carrier erythrocytes in circulation follows a bi-exponential kinetics with a rapid initial decline phase up to 24 hrs after injection (including 15 to 65% of total injected cells) and a slow decline phase with a half-life in the order of days or weeks depending on the animal species used. The initial rapid disappearance is a result of a considerable number of erythrocytes with abnormal sizes and shapes among the carrier erythrocytes’ population. These cells have not re-gained their normal morphology during the restoration period of the loading procedure. The life-span of the white ghosts from the hypotonic dilution method is considerably shorter in comparison to normal erythrocytes. The carrier cells produced by the hypotonic dialysis hypotonic preswelling, and electrical breakdown have shown some normal survival times in circulation [34].
Routes Of Administration:
The carrier cells are injected mainly intravenously or intraarterially, however, intraperitonial and subcutaneous routes can also be utilized [27].
Novel Approaches:
Erythrosomes are made by modifying reverse phase evaporation process. In this method, the human RBC’s are used having cross linkage on which lipid bilayer is coded. This encapsulation system is useful for large molecular drugs [35].
Nanoerythrosomes have average diameter of 100nm. These nano-vesicle are made from membrane of erythrocytes by breakdown method such as sonification, extrusion, electrical breakdown to form uniform size. Mishra and Jain reported that reverse bio-membrane vesicle having doxorubicin drug [36]. Nanoerythrosomes have gave potential significance in clinical treatment.
Major Risk And Limitations:
- Problem in drug loading:
- For this formulation there in a requirement of blood and during manufacturing process of isolation, encapsulation. There is a risk of damage to erythrocytes due to which the resulted formulation will have fraction of initial amount of blood used. This problem limits the manufacturing and availability of the formulation.
- Another problem is of quality control and storage parameters and regulation of drug loaded in erythrocytes. Drug loaded RBC’s have phospholipid bilayer with glycocalyx [65]. This complex allows RBC to circulate up to 3 months.
- Drug loading on RBC’s causes reduction of compatibility with biological system up to some extent. d) Some of the drugs may diffuse out from RBC’s and can interact with blood, cells etc [37].
- This delivery system results in loss of plasticity of RBC up to some extent.
- Due to RBC based drug delivery system there is a inhibition of functions of CD47.
- In, Modified RBC’s elimination gets reduced because of adhesion to endothelium and entrapment in microvascular. Due to which inflammation may arise [38].
- In vitro testing of this formulation such as ionic strength, osmotic resistance shows alteration of RBC’s membrane physiology [39].
Biomedical Applications Of Resealed Erythrocytes:
Resealed erythrocytes have several possible applications in human and veterinary medicine. A majority of drug delivery studies using carrier erythrocytes are in preclinical phase.
1. As Drug/Enzyme Carriers:
Erythrocytes can be used as a carrier for delivery of bioactive compounds as circulatory depots. They can also be used as carriers for targeting drugs to liver, spleen and lymph nodes.
- Erythrocytes as Carriers for Enzymes:
Resealed erythrocytes serve as an ideal carrier for enzymes in the treatment of inherited metabolic disorders. The enzymes used include catalase, urease, uricase, invertase, arginase, asparginase, - glucoronidase, -galactosidase, - fructouronidase, alcohol dehydrogenase, acetaldehyde dehydrogenase and glutamate dehydrogenase (GDH) [40].
- Erythrocytes as Carriers for Drugs:
Erythrocytes are loaded with various bioactive compounds for slow release particularly for antineoplastics, antiparasitics, veterinary antiamoebics, steroids, antibiotics and cardiovascular drugs [41].
- Erythrocytes as Carriers for Proteins and Macromolecules:
Erythrocytes have been used for delivery of various proteins and macromolecules which includes insulin, mycotoxin, recombinant human erythropoietin (rHuEpo) and recombinant interleukin-2 (rIL-2) [42].
2. For Drug Targeting:
Resealed erythrocytes can be used for site-specific and targetoriented drug delivery of loaded drugs. Chemically surface modified erythrocytes are targeted to organs of mononuclear phagocytic system/reticuloendothelial (MPS/RES) system because the changes in the membrane are recognized by macrophages [43].
a) To The RES Organs:
Phagocytic Kupffer cells located in liver and spleen quickly removes the damaged erythrocytes from the circulation. Resealed erythrocytes have been proposed for passive targeting to MPS/RES system where modified surface characteristics provide them selectivity and specificity towards target cells. The various approaches to modify the surface characteristics of erythrocytes include,
- Surface modification with antibodies
- Surface modification with glutaraldehyde
- Surface modification with carbohydrates such as sialic acid
- Surface modification with sulphydryl
- Surface chemical cross-linking e.g. delivery of 125I-labeled carbonic anhydrase loaded in erythrocytes cross-linked with bisulfosuccinimidyl suberate and 3,3- dithiosulfosuccinimidyl propionate [44].
b) To the Liver:
I. Enzyme Deficiency/Replacement Therapy
Enzymes can be injected into blood stream to replace the missing or deficient enzymes in metabolic disorders. Exogenous enzyme therapy is complicated by the short half-life of enzymes in blood stream, allergic reactions and occasionally toxicity against normal tissues. A strategy to eliminate or minimize the problems of immunological nature and toxicity, enzymes loaded erythrocytes have been employed. The enzymes used include -glucosidase, - glucoronidase, -galactosidase. DeLoach and Ihler reported use of glucocerebrosides encapsulated erythrocytes in the disease caused by accumulation of the glucocerebrosides in the liver and spleen [45].
II. Treatment of Hepatic Tumors
Antineoplastic drugs encapsulated in erythrocytes can be used for targeting to hepatic carcinoma. Various agents like methotrexate, bleomycin, asparginasecand andriamycin have been successfully delivered by erythrocytes. The drugs such as daunorubicin rapidly diffuse from the cell upon loading and produce problem which is overcome by covalently linking daunorubicin to the erythrocytic membrane with glutaraldehyde and cis-aconitic acid [46].
III. Treatment of Parasitic Diseases
Erythrocytes can be used for targeting of drugs in the treatment of parasitic disease in which the parasite resides in the RES organs because erythrocytes are selectively accumulated within RES organs. Pentamidine, primaquine phosphate and metronidazole have been successfully utilized for treatment of antimalarial, antileishmanial and antiamoebic drugs in experimental laboratory models. [47].
IV. Removal of RES Iron Overload
RES cells are the primary and the major sites for iron accumulation upon repeated blood transfusion. Iron chelating drugs, desferroxamine has been entrapped in erythrocytes, for promising excretion of iron overload in the RES organs. This therapeutic method is approved in the United States as regular management tool of hemosydrosis since 1984 [48].
V. Removal of Toxic Agents
Cannon et al. Reported antagonism of cyanide intoxication with murine carrier erythrocytes containing bovine rhodanase and sodium thiosulfate. Antagonization of organophosphorus intoxication by using resealed carrier erythrocytes containing a recombinant phosphodiestrase also has been reported [49].
c) To Organs Other Than Those of RES:
Organs other than RES have been tried recently with resealed erythrocytes. Various approaches used for this includes,
- Magnet-responsive erythrocytes ghosts
- Photosensitized erythrocytes
- Antibody anchored erythrocytes (Immunoerythrocytes)
- Ultrasound mediated delivery of erythrocytes loaded drug(s)
Zimmermann and Beckers proposed that the encapsulation of small paramagnetic particles into erythrocytes might allow their localization to the particular location under the influence of external magnetic field. Sprandel et al. reported loading of ferrofluids (colloidal suspension of magnetite) in erythrocytes. Jain and Vyas reported entrapment of the anti-inflammatory drugs diclofenac sodium and ibuprofen in magnetoresponsive erythrocytes. Flynn and co-workers studied photosensitized erythrocytes as a photo-triggered carrier/delivery system for methotrexate in tumour therapy. Chiarantini et al. have reported in vitro targeting of erythrocytes to cytotoxic T-cells by coupling of Thy-1.2 monoclonal antibody. Price et al. reported delivery of colloidal particles and erythrocytes to tissue through microvessel ruptures created by targeted microbubble destruction withultrasound [50].
3. As Circulatory Bioreactors
Erythrocytes have been realized as carriers for enzymes to serve as circulatory bioreactors. This immobilization of enzymes which decreases the level of circulating metabolite can be used as bioreactors [51].
- Delivery of antiviral agents: Several reports have been cited in the literature about antiviral agents entrapped in resealed erythrocytes for effective delivery and targeting. Because most antiviral drugs are nucleotides or nucleoside analogs, their entrapment and exit through the membrane needs careful consideration. Nucleosides are rapidly transported across the membrane whereas nucleotides are not and thus exhibiting prolonged release profiles. The release of nucleotides requires conversion of these moieties to purine or pyrimidine bases. Resealed erythrocytes have been used to deliver deoxycytidine derivatives, recombinant herpes simplex virus type 1 (HSV-1) glycoprotein B, azidothymidine derivatives, azathioprene, acyclovir, and fludarabine phosphate. [52]
- Thrombotic Therapy: Anti-thrombotic agents loaded into the resealed erythrocytes have been proved effective as thrombolytic therapy. Several compounds have been reported for loading into the resealed erythrocytes includes heparin, aspirin and brinase [53].
4. In Oxygen Deficiency Therapy:
Inositol hexaphosphate is an allosteric effector of hemoglobin that has a limited capacity for penetration into erythrocytes. The incorporation of inositol hexaphosphate in erythrocytes produces a modification of the hemoglobin–oxygen affinity, increased O2 release and reduces cardiac output [54]. Encapsulated in red cells, it is irreversibly joined to the intracellular hemoglobin and as a result of its action it increases the transport of O2 and CO2 between lung and tissues. Some authors have studied the consequences of a substantial and long-term increase of the in vivo partial pressure of oxygen in piglets after exchange transfusion with inositol hexaphosphate enriched erythrocytes. The physiological modifications, such as reduced cardiac output in the absence of any other effects detectable, suggests the possible use of these inositol hexaphosphateloaded erythrocytes to restore normal oxygenation of impaired blood flow [55].
Advantages:
Resealed erythrocyte have following advantages:
- Biocompatibility.
- Large number of bioactive agents can be incorporated.
- Large amount of drug can be load in small volume of cell.
- Excretion, degeneration, inactivation of premature protein can be prevented.
- Resealed erythrocytes have long systemic activity.
- Target specific.
Disadvantages Of Resealed Erythrocytes:
Disadvantages of Resealed erythrocytes formulation are summarized as followed [56].
- Biodegradibility of natural cells and materials and this causes toxicological effects in biological system.
- Dose dumping and clumping of cells may take place.
- Alteration of physiological of erythrocytes.
- Possibility of leakage of encapsulation drugs in from loaded RBC’s.
Drawbacks Of Resealed Erythrocytes:
Similar to other drug delivery systems, carrier erythrocytes are limited by various factors. For example, encapsulation may cause an osmotic stress-induced damage to the RBC membrane. Coupling therapeutic moieties to RBCs can lead to the loss of the mechanical stability and plasticity of erythrocytes. These morphological and physiological changes in erythrocytes may trigger an unwanted removal of RBCs by RES; as a consequence, their circulation time in the bloodstream is decreased. Molecules encapsulated in or coupled with RBCs may induce erythrocyte leakage and thus elicit toxic effects. Furthermore, preparation strategies for erythrocyte carriers have yet to be standardized; these carriers are also more varied than synthetic carrier systems. The storage of erythrocyte carriers and risk of blood contamination before, during, and after drug loading should also be highly considered [57].
CONCLUSION:
In conclusion, the use of resealed erythrocytes as drug carriers holds immense promise and potential for targeted drug delivery. This review has shed light on the numerous advantages and challenges associated with this innovative approach. Resealed erythrocytes offer a unique and natural vehicle for drug delivery, mitigating the limitations of conventional drug administration. Their biocompatibility, long circulation half-life, and ability to evade the immune system make them an attractive choice for encapsulating and delivering therapeutic agents. Furthermore, they can be engineered to target specific sites or cells, enhancing drug efficacy while minimizing side effects. However, the technique is not without challenges. Issues related to scale-up, stability, and manufacturing processes need to be addressed for resealed erythrocytes to become a practical and widely adopted drug delivery system. Additionally, tailoring these carriers to specific drugs and disease conditions remains a complex endeavor. In summary, resealed erythrocytes are a promising drug delivery system with the potential to revolutionize the field of medicine. Further research and development are required to overcome existing challenges and bring this innovative technology to the forefront of pharmaceutical science, ultimately offering more effective and targeted therapies for a wide range of diseases.
REFERENCE
- Green, R., and Widder, K. J. 1987. Methods in Enzymology, vol. 149. San Diego: Academic Press.
- Zimmermann, U. 1983. Cellular drug-carrier systems and their possible targeting. In Targeted Drugs, ed. E. P. Goldberg, 153–200. New York: John Wiley & Sons.
- Gardos, G. 1953. Akkumulation de kalium onen durch menschiche Blutkorperchen. Acta Physiol. Acad. Sci. Hung. 6:191–196.
- Marsden, N. V. B., and Ostling, S. G. 1959. Accumulation of dextran in human red blood cells after hemolysis. Nature 184:723–724.
- Zimmermann, U. 1973. Jahresbericht der kernforschungsanlage Julich GmbH, Nuclear Research Center Julich, 55–58.
- Jain, S., and Jain, N. K. 1997. Engineered erythrocytes as a drug delivery system. Indian J. Pharm. Sci. 59:275–28
- Eicher H.G. and Ramies H., Survial of Gentamicine loaded carrier erythrocytes in healthy human volunteers. Eur. J. Clin. Invest. 1986 (1); 16: 39-42.
- Tortora GJ, Grabowski SR. The cardiovascular system: the blood, in principles of anatomy and physiology, Harper Collins College Publishers, New York, NY, 7th ed 1993; 566-90.
- Summers M.P., “Recent Advances in Drug Delivery,” Pharm. J. 1983; 230: 643–645
- Torotra G.J. and Grabowski S.R., “The Cardiovascular System: The Blood,” in Principles of Anatomy and Physiology (Harper Collins College Publishers, New York, NY, 7th ed., 1993), pp. 566–590.
- DeLoach JR, Harris RL, Ihler GM. An erythrocyte encapsulator dialyzer used in preparing large quantities of erythrocyte ghosts and encapsulation of a pesticide in erythrocyte ghosts. Anal Biochem 1998; 102: 220-7.
- Kitao T, Hattori K, Takeshita M. Agglutination of leukemic cells and daunomycin entrapped erythrocytes with lectin in vitro and in vivo. Cell Mol Life Sci 1978; 34(1): 94-5.
- Kinosita, K., Jr, &Tsong, T. T. (1977). Hemolysis of human erythrocytes by transient electric field. Proceedings of the National Academy of Sciences of the United States of America, 74(5), 1923–1927. https://doi.org/10.1073/pnas.74.5.1923
- Kinosita, K., Jr, &Tsong, T. Y. (1978). Survival of sucrose-loaded erythrocytes in the circulation. Nature, 272(5650), 258–260. https://doi.org/10.1038/272258a0
- Zimmermann, U., Riemann, F., & Pilwat, G. (1976). Enzyme loading of electrically homogeneous human red blood cell ghosts prepared by dielelctric breakdown. Biochimica et biophysica acta, 436(2), 460–474. https://doi.org/10.1016/0005-2736(76)90208-x
- Muldoon, L. L., Jamieson, G. A., Jr, &Villereal, M. L. (1987). Calcium mobilization in permeabilized fibroblasts: effects of inositol trisphosphate, orthovanadate, mitogens, phorbol ester, and guanosine triphosphate. Journal of cellular physiology, 130(1), 29–36. https://doi.org/10.1002/jcp.1041300106
- Ihler GM, Tsang HCW. Hypotonic hemolysis methods for entrapment of agents in resealed erythrocytes. Methods Enzymol (Series) 1987; 149: 221-9.
- Flynn, G., McHale, L., & McHale, A. P. (1994). Methotrexate-loaded, photosensitized erythrocytes: a photo-activatable carrier/delivery system for use in cancer therapy. Cancer letters, 82(2), 225–229. https://doi.org/10.1016/0304-3835(94)90016-7
- Vats V. Novel drug delivery system: Resealed Erythrocytes. Turkish Journal of Computer and Mathematics Education (TURCOMAT). 2020 Aug 28;11(2):706-19.
- Billah, M. M., Finean, J. B., Coleman, R., & Michell, R. H. (1977). Permeability characteristics of erythrocyte ghosts prepared under isoionic conditions by a glycol-induced osmotic lysis. Biochimica et biophysica acta, 465(3), 515–526. https://doi.org/10.1016/0005-2736(77)90269-3
- Rechsteiner M. C. (1975). Uptake of proteins by red blood cells. Experimental cell research, 93(2), 487– 492. https://doi.org/10.1016/0014-4827(75)90478-4
- Pitt, E., Lewis, D. A., & Offord, R. E. (1983). The use of corticosteroids encapsulated in erythrocytes in the treatment of adjuvant induced arthritis in the rat. Biochemical pharmacology, 32(22), 3355–3358. https://doi.org/10.1016/0006-2952(83)90362-3
- Bird, J., Best, R., & Lewis, D. A. (1983). The encapsulation of insulin in erythrocytes. The Journal of pharmacy and pharmacology, 35(4), 246–247. https://doi.org/10.1111/j.2042-7158.1983.tb02921.x
- Gothoskar AV. Resealed erythrocytes: a review. Pharm Technol 2004; 140-58.
- Jain S, Jain NK. Engineered erythrocytes as a drug delivery system. Indian J Pharm Sci 1997; 59: 275-81.
- Talwar N, Jain NK. Erythrocytes as carriers of primaquine preparation: characterization and evaluation. J Control Release 1992; 20: 133-42.
- Jain S, Jain NK. In: Jain NK Ed, Controlled and novel drug delivery 1st Ed, 1997; 256-91.
- Jain S, Jain NK. In: Jain N Ed, Advances in controlled and novel drug delivery. CBS Publishers, New Delhi, India 2000; 332-60.
- Magnani M, Rossi L, Bagiotti S, Bianchi M, inventors. Drug delivery systems. United States patent US WO2010145849 A3. 2011 Dec 15.
- Biagiotti S, Rossi L, Bianchi M, et al. Immunophilin-loaded erythrocytes as a new delivery strategy for immunosuppressive drugs. J Control Release. 2011;154(3):306–313.
- Foroozesh M, Hamidi M, Zarrin A, et al. Preparation and in-vitro characterization of tramadol-loaded carrier erythrocytes for long-term intravenous delivery. J Pharm Pharmacol. 2011;63(3):322–332
- DeLoach JR, Barton C. Glutaraldehyde-treated carrier erythrocytes for organ targeting of methotrexate in dogs. Am J Vet Res. 1981;42(11): 1971–1974.
- Baskurt OK. The role of spleen in suppressing the rheological alterations in circulating blood. Clin Hemorheol Microcirc. 1999;20(3): 181–188.
- Luo R, Mutukumaraswamy S, Venkatraman SS, et al. Engineering of erythrocyte-based drug carriers: control of protein release and bioactivity. J Mater Sci Mater Med. 2012;23(1):63–71.
- Field, W. N., Gamble, M. D., and Lewis, D. A. 1989. A comparison of treatment of thyroidectomized rats with free thyroxine and thyroxine encapsulated in erythrocytes. Int. J. Pharm. 51:175–178.
- Hamidi M, Tajerzadeh H. Carrier erythrocytes: an overview. Drug delivery. 2003 Jan 1;10(1):9-20.
- Lewis DA, Alpar HO. Therapeutic possibilities of drugs encapsulated in erythrocytes. Int J Pharm 1984; 22: 137-46.
- Mishra, P. R., & Jain, N. K. (2003). Folate conjugated doxorubicin-loaded membrane vesicles for improved cancer therapy. Drug delivery, 10(4), 277–282. https://doi.org/10.1080/drd_10_4_277
- Svetina S. (2012). Red blood cell shape and deformability in the context of the functional evolution of its membrane structure. Cellular & molecular biology letters, 17(2), 171–181. https://doi.org/10.2478/s11658- 012-0001
- Bossa, F., Annese, V., Valvano, M. R., Latiano, A., Martino, G., Rossi, L., Magnani, M., Palmieri, O., Serafini, S., Damonte, G., De Santo, E., &Andriulli, A. (2013). Erythrocytes-mediated delivery of dexamethasone 21-phosphate in steroid-dependent ulcerative colitis: a randomized, double-blind Shamcontrolled study. Inflammatory bowel diseases, 19(9), 1872–1879. https://doi.org/10.1097/MIB.0b013e3182874065
- Antonelou, M. H., &Seghatchian, J. (2016). Update on extracellular vesicles inside red blood cell storage units: Adjust the sails closer to the new wind. Transfusion and apheresis science : official journal of the World Apheresis Association : official journal of the European Society for Haemapheresis, 55(1), 92–104. https://doi.org/10.1016/j.transci.2016.07.016
- Pan, D., Vargas-Morales, O., Zern, B., Anselmo, A. C., Gupta, V., Zakrewsky, M., Mitragotri, S., &Muzykantov, V. (2016). The Effect of Polymeric Nanoparticles on Biocompatibility of Carrier Red Blood Cells. PloS one, 11(3), e0152074. https://doi.org/10.1371/journal.pone.0152074
- DeLoach JR, Ihler GM. A dialysis procedure for loading of erythrocyte with enzymes and lipids. Biochim Biophys Acta 1977; 496: 136-45.
- Hirlekar RS, Patel PD, Dand N, Kadam VJ. Drug loaded erythrocytes: as novel drug delivery system. Current pharmaceutical design. 2008 Jan 1;14(1):63-70.
- Moyes RB, Kirch H, DeLoach JR. Enhanced biological activity of human recombinant interleukin 2 coupled to mouse red blood cells as evaluated using the mouse Meth A sarcoma model. Biotechnol Appl Biochem 1996; 23: 29-36.
- Alvarez FJ, Jordán JA, Calleja P, Lotero LA, Olmos G, Díez JC, et al. Cross-linking treatment of loaded erythrocytes increases delivery of encapsulated substance to macrophages. Biotechnol Appl Biochem 1998; 27(2): 139-43.
- Naqi A, DeLoach JR, Andrews K, Satterfield W, Keeling M. Determination if parameters for enzyme therapy using L-asparginase entrapped in canine erythrocytes. Biotechnol Appl Biochem 1988; 10(4): 65-72.
- Vyas SP, Khar RK. Resealed erythrocytes in targeted and controlled drug delivery: novel carrier systems, CBS Publishers and Distributors, India 2002; 387-416.
- Jaitely V, Kanaujia P, Venkatesan N, Jain S, Yyas SP. Resealed erythrocytes: drug carrier potentials and biomedical applications. Indian Drugs 1996; 33: 589-94.
- Summers MP. Recent advances in drug delivery. Pharm J 1983; 230: 643-5.
- Gothoskar AV. Resealed erythrocytes: a review. Pharm Technol 2004; 140-58.
- Pei L, Omburo G, Mcguinn WD, Petrikovics I, Dave K, Raushel FM, et al. Encapsulation of phosphotriesterase within murine erythrocytes. Toxicol Appl Pharmacol 1994; 124(2): 296-1.
- Ihler GM. Erythrocyte carriers. Pharmacol Ther 1983; 20: 151-69.
- Fraternale A, Rossi L., and M. Magnani, “Encapsulation,Metabolism, and Release of 2- Fluoro-Ara-AMP from Human Erythrocytes,” Biochim. Biophys. Acta.1996;1291(2):149–154.
- Thromb Res 1990; 57: 611-6. [77] Flynn G, McHale L, McHale AP. Methotrexate-loaded, photosensitized erythrocytes: a photo-activatable carrier/delivery system for use in cancer therapy. Cancer Lett 1994; 82(2): 225-9.
- illan CG, Marinero MLS, Castaneda AZ, Lanao JM. Drug, enzyme and peptide delivery using erythrocytes as carriers. J Control Release 2004; 95: 27-49.
- Hamidi, M., Zarrin, A., Foroozesh, M., &Mohammadi-Samani, S. (2007). Applications of carrier erythrocytes in delivery of biopharmaceuticals. Journal of controlled release: official journal of the Controlled Release Society, 118(2), 145–160. https://doi.org/10.1016/j.jconrel.2006.06.032


 Aishwarya Mahaveer Ingrole *
Aishwarya Mahaveer Ingrole *
 Bhartesh Shirdhone
Bhartesh Shirdhone
 10.5281/zenodo.12740027
10.5281/zenodo.12740027