Abstract
A typical nail fungal infection that can cause thickness, discolouration, and occasionally nail detachment is called onychomycosis. Dermatophytes, yeasts, and molds are the most common causes, and those with diabetes, weakened immune systems, or other medical disorders are more likely to have it. New topical treatments, such as tavaborole and efinaconazole, offer effective alternatives to older oral antifungals, with fewer side effects and improved cure rates. Diagnosis typically involves mycological testing, including microscopy and culture. Early diagnosis and appropriate treatment are key to managing onychomycosis and preventing complications. This review highlights the causes, symptoms, diagnostic methods, and emerging therapies for onychomycosis, emphasizing the promise of new antifungal options.
Keywords
Onychomycosis, Fungal Nail Infection,
Introduction
Fungal infections of the nails, hair, and skin, including tinea pedis and hard tinea and tinea unguium are common worldwide [1,2]. The newest class of topical antifungal treatment are a new class of drug called oxaboroles, that contain boron. It has been found that boron has a unique capacity to bind functional group to certain enzyme target sites, rendering them inaccessible and reducing their functionality. The first molecule in this therapeutic family, the Food and Drug Administration (FDA) authorized a topical solution containing 5% to treat toenail onychomycosis in July 2018 [3]. Onychomycosis is a chronic nail fungal infection that results in deformation, discolouration, thickness, and nail separation [2]. Onychomycosis affecting 50% of all nail diseases of the global population and is one of the most prevalent nail conditions in adulthood.The increase number of patient with diabetes mellitus and the increase in peripheral vascular disease [4]. Patients with impaired immune systems, like those who have HIV (human immunodeficiency virus), may experience serious health complications from onychomycosis. The patient is constantly reminded of their own worsening health by the challenging illness, and there is a chance that they might spread a very high titer of fungal infections to someone else.
Individuals who suffer from HIV, or human immunodeficiency virus illness, have a 25% greater prevalence [5,6]. There are several different types of fungi that can cause onychomycosis, a common fungal infection of the fingernails and toenails. Yeast, dermatophytes, and non-dermatophyte molds (NDMs) are the most frequent causes of this disease. Non-dermatophytes were the most prevalent fungus found in the patients in those investigations, such as candida spp.(69%). Additionally, the study found that diabetes patient had on 88% higher risk of developing onychomycosis than non-diabetic individual and that each year of age increases the chance of onychomycosis by 1.9% [7,8].
Etiology: -
A wide range of fungi can cause onychomycosis, and the main reason why this changes from one region to another is because of the climate [9].
Dermatophytes: -
The most often identified causal agents of onychomycosis (about 90% in toenails and 50% in fingernails) are dermatophytes. The invasion of the nail plate by dermatophytes is known as tinea unguium. Trichophyton rubrum (T. rubrum) is the most common causative agent, followed by T. mentagrophytes [9,10].
Nondermatophytes Molds (NDM): -
mostly impact toenails, with fingernails being affected typically. NDM makes up 1.5–6% of all onychomycoses, which are separated into two categories: The initial group includes fungi like Scytalidium dimidiatum and Scytalidium hyalinum As etiologic agents, they are often isolated from nails, whereas the second group includes opportunistic fungus like Aspergillus sydowii, Onychocola canadensis, and others that can potentially be identified as pollutants, and Scopulariopsis brevicaulis [11,12]. Acremonium species and other NDMs can penetrate the nail surface, however Scytalidium species and other NDMs are more frequently linked to lateral and distal subungual onychomycosis. When the following conditions are met, molds are regarded as pathogens:
- Abnormalities of the nails that match the diagnosis.
- The hyphae in the nail keratin may be seen using positive direct microscopy.
- The culture's inability to isolate a dermatophyte.
- The development of at least five colonies of the same mold in two nail samples in a row [11].
Consideration should be given to mold involvement if there is no history of trauma, tinea pedis, or the emergence of one or two infected toenails with periungual inflammation [9].
Yeasts: -
About 70% of candida albicans is the cause of onychomycosis brought on by yeast. Candida also includes the species Candida tropicalis and Candida parapsilosis. The yeast organism is more likely to infect patients with immunodeficiency and chronic mucocutaneous candidiasis, particularly in the fingernails [10,13].
Sing and Symptoms: -
The most typical signs of onychomycosis are nail thickening (hyperkeratosis) and discolouration (green, yellow, black, or white). Additionally, the nail bed may become infected, exhibiting scaly skin next to the nail or white or yellow areas on the nailbed. In general, onychomycosis is may not produce physical discomfort, but if treatment is not received, the infection may progress and the and irritation and soreness of the skin may result. Dermatophytids can occasionally show up as a red, scaly, itchy, circular rash [14,15]. Dermatophytoma is another way that onychomycosis manifests itself. This is distinguished by a profusion of fungi. Compressed filaments, big spores, or both that combine to form a fungal ball. Clinically, a spherical mass of white or yellowish color or a linear band can be observed; microscopically, the presence of a fungus can be confirmed in nail samples from those suspected of having onychomycosis using chlorazol black E or potassium hydroxide (KOH) preparation [16].
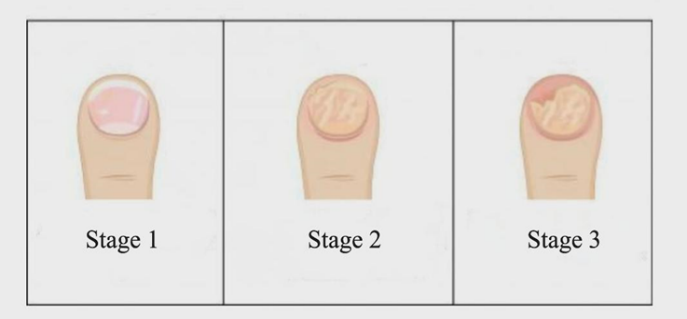
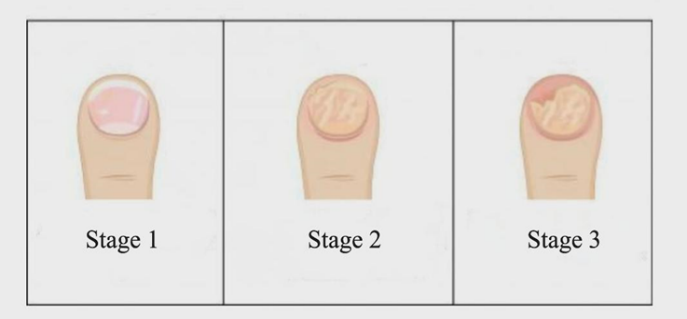
Fig: - A fungal infection on the nail's stages
Stage 1: - The nail plate remains transparent and glossy, but it has started to become yellow and white.
Stage 2: - The entire nail plate is covered in yellowish patches, and the plate has lost its sheen and clarity. It started to partially destroy the nail.
Stage 3: - The thickness of the nail plate is increasing. The nail lags behind the nail bed and starts to disintegrate.
Clinical Characteristics: -
There are five main ways that onychomycosis manifests clinically
- Distal and Lateral subungual Onychomycosis (DLSO)
- Proximal Subungual Onychomycosis (PSO)
- Superficial White Onychomycosis (SWO)
- Endonxy Onychomycosis
- Total Dystrophic Onychomycosis (TDO)
- Distal and Lateral Subungual Onychomycosis (DLSO): -
Distal lateral subungual is the most common clinical subtype of onychomycosis. A fungal invasion that starts at the hyponychium and spreads to the distal nail bed and nail plate is the cause of distal lateral subungual onychomycosis. The fungus then forms "spikes" or linear channels as it travels proximally through the nail plate [17]. Trichophyton rubrum is the most prevalent source of this clinical subgroup, while Trichophyton mentagrophytes is less frequent. Distal lateral subungual onychomycosis manifests clinically as a darkening of the distal corner of a nail that is yellowish, white, or brownish. Onycholysis, onychauxis, and/or distal subungual hyperkeratosis of the nail plate's distal and lateral regions are commonly observed [18].

Fig: - Distal and Lateral Subungual Onychomycosis
- Proximal Subungual Onychomycosis (PSO):-
The fungus that causes proximal subungual onychomycosis spreads away from the underside of the proximal nail fold and toward the cuticle. Fusarium spp. and Trichophyton rubrum are often the causes of this clinical subgroup [19]. The clinical disorder known as proximal subungual onychomycosis starts as the nail grows, it begins as a leukonychia that spreads distally from the proximal nail plate. Patients with immunodeficiency, particularly those with acquired immunodeficiency syndrome (AIDS), have a higher chance of developing proximal subungual onychomycosis [20].

Fig: - Proximal Subungual Onychomycosis
- Superficial White Onychomycosis (SWO): -
Colonies of fungi that penetrate the dorsal nail plate are readily scraped away and have an opaque white appearance. Trichophyton interdigitale is responsible for the classical form, in which dermatophytes proliferate the nail plate's outermost layers without entering it; nevertheless, Fusarium spp. and other white superficial onychomycosis (WSO) with a deeper nail invasion can be brought on by molds. It is common 2 for T. interdigitale to cause tinea pedis interdigitalis, often known as athlete's foot [22,23,18].

Fig: - Superficial White Onychomycosis
- Endonyx Onychomycosis: -
Endonyx onychomycosis is caused by fungus that infects the nail plate without infecting the nail bed. Trichophyton violaceum and Trichophyton soundanense are the primary culprits of this clinical subgroup [21]. Clinical indicators of endonyx onychomycosis include milky patches, indentations, and lamellar cracking of the nail plate. The nail plate and nail bed are securely linked, and there is no subungual hyperkeratosis [24].

Fig: - Endonyx Onychomycosis
Total Dystrophic Onychomycosis (TDO): -
The nail crumbles because the entire nail plate is damaged and vanish, leaving behind an abnormally swollen nail bed that still contains keratotic nail debris. It can happen as a secondary consequence of any of the four primary patterns [20,24]. Only individuals with CMC or immunodeficient conditions have primary TDO, when the distal phalanx swells and becomes more bulbous than clubbed due to the swelling of soft tissues and a thickened, opaque, yellow-brown nail plate [25].

Fig: - Total dystrophic onychomycosis
Diagnosis of Onychomycosis: -
Onychomycosis requires a thorough diagnosis before treatment can begin. Mycology should validate the onychomycosis clinical suspicion. The two components of the mycological examination are the culture and the direct microscopic inspection [19]. In order to check for hyphae and spores, the nail material from the infected nail is first taken, submerged in a 40% KOH solution, and thereafter put on a slide for optical microscope examination. The kind of fungus causing onychomycosis cannot be identified with KOH; a culture is required for a more precise diagnosis. The periodic acid-Schiff (PAS) stain, which makes fungal hyphae readily visible, can be used to histopathologically examine nail clippings in order to identify onychomycosis [26]. Onychoscopy, also known as digital dermoscopy, is a rapid and simple technique that enables onychomycosis to be differentiated from other common nail dystrophies.
Raman spectroscopy, fluorescence microscopy, and dermatophyte test strips are a few more intriguing new methods for diagnosing onychomycosis [27]. The monoclonal antibody-based immunochromatography test in the dermatophyte test strip interacts with Trichophyton species and, after 15 minutes, generates a favorable indication when coming into touch with one of these dermatophytes [28]. This kit is ready to use, quick, simple, and reasonably priced. Because of the test's great sensitivity and negative predictive value, onychomycosis may be ruled out in any situation where there is any question. The technique was previously applied in a brief onychomycosis series [29]. Microscopy using fluorescence is the process of using a fluorescent microscope to examine nail clippings stained with PAS from suspected cases of onychomycosis. This technique is less expensive than PAS stain, however it cannot differentiate between various fungal species or between living and dead hyphae [4,29]. The drawbacks include the requirement for expertise and training, the challenge of distinguishing genuine fungal fluorescence from false positives, and the reduced specificity in contrast with PAS and other unique stains [30]. A vibrational spectroscopic technique called Raman spectroscopy looks at the molecular specificity of spectral bands in a vibration spectrum to determine the molecular makeup of materials. Smijis et al. only presented initial findings because the study was conducted in vitro on fungal-infected nail clippings [31].
Treatment: -
Treatment options for onychomycosis include debridement, surgical nail plate removal (nail avulsion), antifungal medications applied topically and orally, as well as device-based therapies (such laser therapy). It is recommended to use topical medications to treat mild to severe onychomycosis and device-based therapies, although oral antifungal medications are often advised for moderate to severe cases [32,33]. If the fungus is exclusive to the nail plate, nail avulsion, an invasive procedure, may occasionally be successful in curing the infection. Debridement can reduce the fungal burden and support topical treatment, although it does not always cure nail infections [34,35].
Oral treatment: -
This is the earliest therapeutic approach used when fungus affects at least 50% of the nails. For onychomycosis, antifungal medications such as ketoconazole and terbinafine, itraconazole, fluconazole, and griseofulvin are available orally [5]. Because nail development is sluggish, oral antifungal therapy requires a long time and is therefore not patient-friendly. Long-term treatment causes serious side effects and drug interactions. The dose, spectrum of activity, and method of action of the antifungal drugs [36].
Terbinafine: - Terbinafine is the first allylamine that has been thoroughly researched when taken orally [37]. It works against dermatophytes, but not against yeasts like Candida albicans.13 Terbinafine caused a mycological cure in 82% of cases at 1 year in a trial of individuals with nail dermatophyte infections who received 250 mg/d for three months [38].18- Compared to prior systemic medications, terbinafine considerably shortens the duration of therapy. It takes a minimum of three weeks, and perhaps as long as eight weeks, for the medication to be initially identified in the distal nail plate [39].
Kitoconazole: - Traditional imidazole antifungals like ketoconazole are used to treat dermatophytes. A dosage of 200 mg per day can induce a cure rate of up to 50%, but it has a number of disadvantages, including a lengthy course of therapy, liver toxicity, a low treatment rate, and the potential for teratogenicity, nausea, allergies, and hormone imbalance. It is thus not used to treat onychomycosis [2,39].
Itraconazole: - Itraconazole pulse therapy and continuous terbinafine are both safe and efficient treatments for diabetics with dermatophyte toenail onychomycosis. These routines may use topical nail lacquers. 400 mg of itraconazole per day for one week every month is the dose used in pulse treatment. The length of treatment for fingernails is two months, and for toenails, it is three months [40].
Fluconazole: - For dermatophyte onychomycosis, fluconazole, which works better than topical therapies, is not always licensed in every country. For fingernail onychomycosis, For six to nine months, take 150–300 mg once weekly, and for toenail onychomycosis, 9–18 months, is recommended for complete outgrowth of the affected nail [14,15].
Griseofulvin: - Griseofulvin inhibits the development of mitotic spindles, which is how it only combats dermatophytes. The nail takes a long time to become saturated, and after treatment is stopped, it remains there for almost two weeks [41]. Low compliance results from this, and it takes a long time to administer (10–18 months for toenails and 4–9 months for fingers, respectively). Griseofulvin is the least prescribed drug due to the low rates of mycological cure, which around 70% for fingernails onychomycosis and For toenail onychomycosis, 30–40%. Adults should take 500 mg to 1 g per day, following a high-fat meal [27].
Topical treatment: -
Topical medications are suggested only for individuals who cannot take systemic treatment or in circumstances where the distal nail plate is impacted in less than half. In the US, agents like efinaconazole 10% nail solution and ciclopirox olamine 8% are available. Outside of the United States, amorolfine and bifonazole/urea are accessible [29].
Common Topical Antifungal Agents:
Ciclopirox: - A broad-spectrum antifungal medication called ciclopirox is sold as nail lacquer. For several months (generally 6–12 months), it is administered directly to the damaged nail and surrounding tissue once a day. It is believed that ciclopirox functions by preventing the production of fungal cell membranes. Studies have indicated that it is somewhat effective in treating onychomycosis, with long-term treatment leading to cure rates of 8–30% [29,43].
Efinaconazole: - A newer and effective topical antifungal medication is finaconazole. In clinical studies, this once-daily topical solution has been demonstrated to be more effective than previous therapies. Usually used for 48 weeks, finaconazole is administered directly to the afflicted nail. It works very well against dermatophytes, which are the most frequent cause of onychomycosis. Clinical trials show cure rates between 10% and 20%, with mild-to-moderate patients showing better results [44,45].
Tavaborole: - A boron-based solution called tavaborole 5% stops the development of fungal cells and prevents the nail plate's protein production. This medication is especially useful if an infection doesn't seem to respond well to other antifungals [50]. For 48 weeks, tavaborole should be used every day to cure toenail onychomycosis brought on by T. rubrum and T. interdigitale [46]. Although effectiveness against yeasts and NDM is not yet proven, action taken against these species has been seen in vitro. Long-term advantages of tavaborole is extensible, as seen by the 29% full cure rates at 60 days in those who had become entire or nearly clean nails 52 weeks in. Onychomycosis can be concealed during treatment since cosmetic nail polish has minimal impact on the entry of 5% tavaborole and 10?inaconazole into the nail [47].
The two recently authorized antifungal topical, tavaborole and finaconazole, are solutions rather than lacquers [48,49].
CONCLUSION: -
A common and chronic fungal infection that affects nails is called onychomycosis, with higher prevalence in people with diabetes and weakened immune systems. The condition is caused by dermatophytes, molds, and yeasts, and can lead to nail thickening, discoloration, and sometimes pain.
Recent advancements in treatment, including new topical antifungals like tavaborole (oxaborole class) and efinaconazole, offer effective alternatives to older oral medications, which often have lengthy treatment durations and side effects. Tavaborole, in particular, has shown promise in treating infections that resist traditional antifungals. While treatments have improved, early diagnosis through methods like onychoscopy and fungal cultures remains critical. Continued research into safer, more effective therapies is needed to better manage onychomycosis and reduce its impact, especially for vulnerable groups.
REFERENCES
- Sahni, Kanika, Sanjay Singh, and Sunil Dogra. "Newer topical treatments in skin and nail dermatophyte infections." Indian dermatology online journal 9.3 (2018): 149-158.
- Aggarwal, Rohan, et al. "Onychomycosis: Novel strategies for treatment." Journal of Drug Delivery Science and Technology 57 (2020): 101774.
- Jinna, Sphoorthi, and Justin Finch. "Spotlight on tavaborole for the treatment of onychomycosis." Drug design, development and therapy (2015): 6185-6190.
- Piraccini, Bianca Maria, and Aurora Alessandrini. "Onychomycosis: a review." Journal of Fungi 1.1 (2015): 30-43.
- Aggarwal, R., Targhotra, M., Kumar, B., Sahoo, P. K., & Chauhan, M. K. (2020). Treatment and management strategies of onychomycosis. Journal de mycologie medicale, 30(2), 100949.
- Gupta, Aditya K., Richard K. Scher, and Piet De Doncker. "Current management of onychomycosis: an overview." Dermatologic clinics 15.1 (1997): 121-135.
- Eftekhari, H., Saheli, Y. H., Ashoobi, M. T., Mahjoob, M., Leyli, E. K., & Toolaroud, P. B. (2024). The prevalence of onychomycosis in patients with chronic renal failure undergoing dialysis: A cross-sectional study. Heliyon, 10(4).
- Haneke, E. (2024). Onychomycosis in Foot and Toe Malformations. Journal of Fungi, 10(6), 399.
- Singal, Archana, and Deepshikha Khanna. "Onychomycosis: Diagnosis and management." Indian journal of dermatology, venereology and leprology 77 (2011): 659.
- Ngwogu, A. C., Mba, I. E. K., & Ngwogu, K. O. (2014). Onychomycosis: Etiology, diagnosis, and treatment. Journal of medical Investigations and Practice, 9(1), 43.
- Kaur, R., Kashyap, B., & Bhalla, P. (2008). Onychomycosis-epidemiology, diagnosis and management. Indian Journal of Medical Microbiology, 26(2), 108-116.
- Scher, R. K., Rich, P., Pariser, D., & Elewski, B. (2013). The epidemiology, etiology, and pathophysiology of onychomycosis. , 32, 32(2), 2-4.
- da Silva, A. P., Nogueira, M. S., Jo, J., Bagnato, V. S., & Inada, N. M. (2016, April). Optical based diagnosis and treatment of onychomycosis. In Cancer Imaging and Therapy (pp. JTu3A-37). Optica Publishing Group.
- Gupta, A. K., Mays, R. R., Versteeg, S. G., Shear, N. H., & Piguet, V. (2018). Update on current approaches to diagnosis and treatment of onychomycosis. Expert Review of Anti-Infective Therapy, 16(12), 929-938.
- Welsh, Oliverio, Lucio Vera-Cabrera, and Esperanza Welsh. "Onychomycosis." Clinics in dermatology 28.2 (2010): 151-159.
- Behera, J. K., Kumar, S., Sharma, R., Jain, A., Garg, N. K., Khopade, A., ... & Nirbhavane, P. (2023). Novel Discoveries and Clinical Advancements for Treating Onychomycosis: A Mechanistic Insight. Advanced Drug Delivery Reviews, 115174.
- Dubljanin, Eleonora, et al. "Onychomycosis: clinical findings, etiological agents and evaluation of laboratory methods." Archives of Biological Sciences 66.2 (2014): 587-594.
- Elewski, Boni E. "Onychomycosis: pathogenesis, diagnosis, and management." Clinical microbiology reviews 11.3 (1998): 415-429.
- Piraccini, Bianca Maria, and Aurora Alessandrini. "Onychomycosis: a review." Journal of Fungi 1.1 (2015): 30-43.
- Baran, et al. "A new classification of onychomycosis." British Journal of Dermatology 139.4 (1998): 567-571.
- Leung, A. K., Lam, J. M., Leong, K. F., Hon, K. L., Barankin, B., Leung, A. A., & Wong, A. H. (2020). Onychomycosis: an updated review. Recent patents on inflammation & allergy drug discovery, 14(1), 32-45.
- Carney, C., Tosti, A., Daniel, R., Scher, R., Rich, P., DeCoster, J., & Elewski, B. (2011). A new classification system for grading the severity of onychomycosis: Onychomycosis Severity Index. Archives of dermatology, 147(11), 1277-1282.
- Gupta, Aditya K., et al. "Systematic review of nondermatophyte mold onychomycosis: diagnosis, clinical types, epidemiology, and treatment." Journal of the American Academy of Dermatology 66.3 (2012): 494-502.
- Shah, Vidhi V., and Antonella Tosti. "Endonyx Onychomycosis." Onychomycosis: An Illustrated Guide to Diagnosis and Treatment (2017): 57-60.
- Faergemann, J., & Baran, R. (2003). Epidemiology, clinical presentation and diagnosis of onychomycosis. British Journal of Dermatology, 149(s65), 1-4.
- Loeser, C. R., Nenoff, P., Mainusch, O., Dippel, E., & Balakirski, G. (2021). Common diseases of the nail: Diagnosis and therapy. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 19(12), 1761-1775.
- Gupta, Aditya K., et al. "Update on current approaches to diagnosis and treatment of onychomycosis." Expert Review of Anti-Infective Therapy 16.12 (2018): 929-938.
- Westerberg, Dyanne P., and Michael J. Voyack. "Onychomycosis: current trends in diagnosis and treatment." American family physician 88.11 (2013): 762-770.
- Singal, Archana, and Deepshikha Khanna. "Onychomycosis: Diagnosis and management." Indian journal of dermatology, venereology and leprology 77 (2011): 659.
- Tchernev, Georgi, et al. "Onychomycosis: modern diagnostic and treatment approaches." Wiener Medizinische Wochenschrift (1946) 163.1-2 (2012): 1-12.
- Falotico, J. M., & Lipner, S. R. (2022). Updated perspectives on the diagnosis and management of onychomycosis. Clinical, Cosmetic and Investigational Dermatology, 1933-1957.
- Gupta, Aditya K., Maryse Paquet, and Fiona C. Simpson. "Therapies for the treatment of onychomycosis." Clinics in dermatology 31.5 (2013): 544-554.
- Grover, Chander, and Ananta Khurana. "An update on treatment of onychomycosis." Mycoses 55.6 (2012): 541-551.
- Pajaziti, Laura, and Ermira Vasili. "Treatment of onychomycosis–A clinical study." Medical Archives 69.3 (2015): 173.
- Shirwaikar, A. A., Thomas, T., Shirwaikar, A., Lobo, R., & Prabhu, K. S. (2008). Treatment of onychomycosis: an update. Indian journal of pharmaceutical sciences, 70(6), 710.
- Zane, L. T., Chanda, S., Coronado, D., & Del Rosso, J. (2016). Antifungal agents for onychomycosis: new treatment strategies to improve safety. Dermatology Online Journal, 22(3).
- Jaffe, Rebecca. "Onychomycosis: recognition, diagnosis, and management." Archives of family medicine 7.6 (1998): 587.
- Darkes, Malcolm JM, Lesley J. Scott, and Karen L. Goa. "Terbinafine: a review of its use in onychomycosis in adults." American journal of clinical dermatology 4.1 (2003): 39-65.
- Drake, Lynn A., et al. "Oral terbinafine in the treatment of toenail onychomycosis: North American multicenter trial." Journal of the American Academy of Dermatology 37.5 (1997): 740-745.
- Botter, A. A., & Nuijten, S. T. M. (1981). Further experiences with ketoconazole in the treatment of onychomycosis. Mycoses, 24(3), 156-166.
- Hargreaves, G. K. (1960). The treatment of onychomycosis with griseofulvin. British Journal of Dermatology, 72(10), 358-364.
- Baran, R., & Kaoukhov, A. (2005). Topical antifungal drugs for the treatment of onychomycosis: an overview of current strategies for monotherapy and combination therapy. Journal of the European Academy of Dermatology and Venereology, 19(1), 21-29.
- Bohn, Manfred, and Karl Th Kraemer. "Dermatopharmacology of ciclopirox nail lacquer topical solution 8% in the treatment of onychomycosis." Journal of the American Academy of Dermatology 43.4 (2000): S57-S69.
- Lipner, S. R., & Scher, R. K. (2015). Efinaconazole in the treatment of onychomycosis. Infection and drug Resistance, 163-172.
- Eisman, S., & Sinclair, R. (2014). Fungal nail infection: diagnosis and management. Bmj, 348.
- Gupta, A. K., & Versteeg, S. G. (2016). Tavaborole–a treatment for onychomycosis of the toenails. Expert Review of Clinical Pharmacology, 9(9), 1145-1152.
- Sharma, N., & Sharma, D. (2015). An upcoming drug for onychomycosis: Tavaborole. Journal of Pharmacology and Pharmacotherapeutics, 6(4), 236-239.
- Elewski, B. E., & Tosti, A. (2014). Tavaborole for the treatment of onychomycosis. Expert opinion on pharmacotherapy, 15(10), 1439-1448.
- Poulakos, M., Grace, Y., Machin, J. D., & Dorval, E. (2017). Efinaconazole and tavaborole: emerging antifungal alternatives for the topical treatment of onychomycosis. Journal of Pharmacy Practice, 30(2), 245-255.
- Gupta, A. K., & Daigle, D. (2014). Potential role of tavaborole for the treatment of onychomycosis. Future Microbiology, 9(11), 1243-1250.


 Sangeeta Manjhi*
Sangeeta Manjhi*
 Bhishesar Sahu
Bhishesar Sahu
 Kamini Sonwani
Kamini Sonwani
 Dhatri Sahu
Dhatri Sahu
 Munmun Bhattacharya
Munmun Bhattacharya





 10.5281/zenodo.14245230
10.5281/zenodo.14245230