Abstract
Managing blood glucose levels is a significant challenge for patients with advanced type 2 diabetes mellitus (T2DM) and type 1 diabetes mellitus (T1DM), often necessitating insulin therapy. Traditional subcutaneous insulin injections, while effective, are associated with drawback such as pain, anxiety and non-compliance. To address these limitations, researchers are exploring alternative, minimally invasive and non-invasive insulin delivery methods. This review article provides a comprehensive overview of the evaluation of insulin delivery technologies, highlighting past successes and failures, current advancements and future prospects. We examine various emerging routes of insulin administration, including oral, buccal, nasal, peritoneal and transdermal delivery. This review also explores the potential for a new drug development and innovation in insulin delivery, with a focus on improving patient outcomes and quality of life.
Keywords
Revolutionizing Insulin Delivery, Trends and Technology, pain, anxiety and non-compliance.
Introduction
The global burden of diabetes continues to escalate, with the International Diabetes Federation projecting a rise in prevalence from 537 million in 2021 to 643 million by 2030 and 784 million by 2045. Type 2 diabetes mellitus (T2DM) remains the dominant form, accounting for approximately 90% of all diabetes cases. However, the incidence of type 1 diabetes mellitus (T1DM) is also increasing, particularly among children and adolescents in certain regions. As one of the most prevalent non-communicable diseases worldwide, diabetes poses a significant threat to public health, emphasizing the need for continued research, improved treatment options, and enhanced prevention strategies.
Diabetes Mellitus
Diabetes mellitus (DM) is a complex metabolic disorder characterized by chronic hyperglycaemia, defined by fasting plasma glucose levels ?126 mg/dL and/or ?200 mg/dL 2 hours after a 75-g oral glucose challenge. The condition is often accompanied by glycosuria, hyperlipidaemia, negative nitrogen balance, and occasionally ketonemia. At the molecular level, DM is associated with widespread pathological changes, including thickening of capillary basement membranes, increased vascular matrix deposition, and cellular proliferation. These alterations contribute to the development of vascular complications, such as accelerated atherosclerosis, glomerular sclerosis, retinopathy, neuropathy, and peripheral vascular insufficiency, ultimately leading to significant morbidity and mortality.
Types of Diabetes Mellitus
- Type 1 Diabetes: An autoimmune disease where the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas, resulting in a complete deficiency of insulin production.
- Type 2 Diabetes: A metabolic disorder characterized by insulin resistance and impaired insulin secretion, often associated with obesity, physical inactivity, and a diet high in sugar and unhealthy fats.
- Gestational Diabetes: A type of diabetes that develops during pregnancy, usually in the second or third trimester, due to hormonal changes and insulin resistance.
- LADA (Latent Autoimmune Diabetes in Adults): A form of type 1 diabetes that develops in adults, often after the age of 30, and is characterized by a slow progression to insulin dependence.
Symptoms
Hyperglycaemia include excessive thirst (polydipsia), frequent urination (polyuria), increased hunger (polyphagia), blurred vision, and unexplained weight loss. Additionally, hyperglycaemia can lead to growth impairment in children and adolescents, and increase the risk of developing various infections.
Diabetes Related Complications
Prolonged diabetes can lead to severe complications, including nephropathy (renal failure), retinopathy (vision loss), and peripheral neuropathy (Charcot joints, foot ulcers, and amputations). Additional complications may include sexual dysfunction, autonomic neuropathy (gastrointestinal, cardiovascular, and genitourinary symptoms), and increased risk of peripheral arterial, cerebrovascular, and cardiovascular diseases. These cardiovascular risks are often exacerbated by dyslipidaemia and hypertension.
Insulin
Insulin is a pivotal hormone regulating glucose metabolism, was first discovered in 1921 by Frederick Banting and Charles Best. Their groundbreaking work demonstrated the hypoglycemic effect of an extract from the pancreas, obtained after degenerating the exocrine portion through pancreatic duct ligation. Subsequent research led to the purification of insulin, with the first crystalline form obtained in 1926. The chemical structure of insulin was fully elucidated by Frederick Sanger in 1956. Insulin is a two-chain polypeptide, comprising 51 amino acids with a molecular weight of approximately 6000. The A-chain consists of 21 amino acids, while the B-chain contains 30 amino acids. This unique structure enables insulin to play a crucial role in glucose homeostasis.
Structure of Insulin
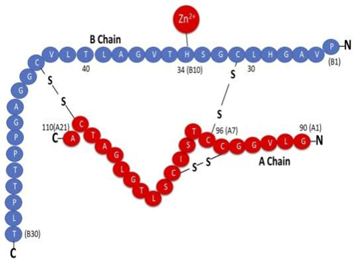
Insulin is a polypeptide hormone with a molecular weight of approximately 6,000. It consists of two chains: the A-chain, comprising 21 amino acids, and the B-chain, comprising 30 amino acids. These chains are linked by two disulphide bridges. The precursor to insulin, proinsulin, is synthesized within pancreatic ?-cells and consists of the A and B chains connected by a 31-amino acid “connecting” peptide, also known as the C-peptide. Proinsulin has a molecular weight of 9,000. Notably, insulin has been fully synthesized; however, the majority of current insulin supplies are derived from the pancreas of cattle (bovine).
Insulin’s Mechanism of Action:
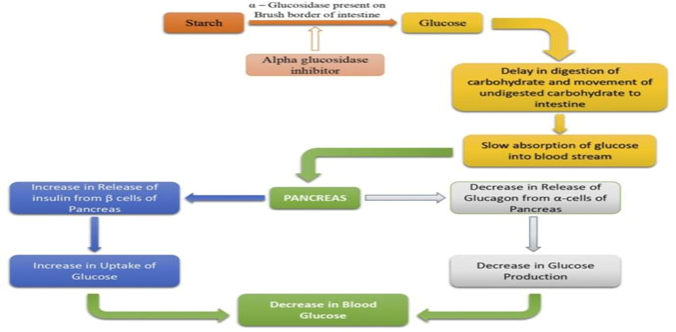
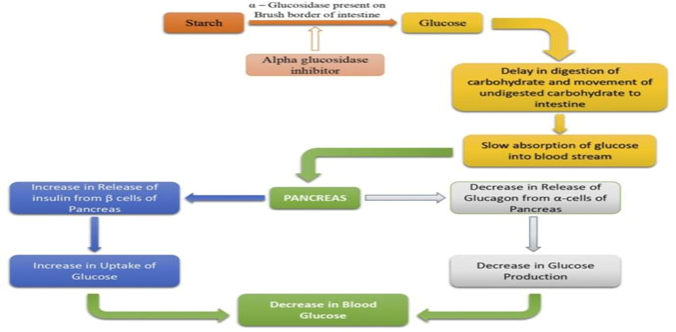
Insulin plays a crucial role in maintaining blood glucose homeostasis by regulating gluconeogenesis and glycogenolysis. The primary mechanism involves inhibiting glucose production in the liver, thereby enhancing glucose uptake in muscles and other tissues. Following a meal, hyperglycaemia stimulates pancreatic ?-cells to release insulin within 1-10 minutes. The released insulin enters systemic circulation, facilitating its distribution to target cells, including hepatocytes. In hepatocytes, insulin promotes glycogen deposition, reducing blood sugar levels. Additionally, insulin stimulates glucose consumption in skeletal muscles and adipose tissues. This coordinated mechanism involving insulin secretion and distribution helps restore plasma sugar levels to fasting state levels, maintaining glucose homeostasis.
Current Insulin Delivery Systems
The range of insulin delivery systems currently available includes traditional syringes, insulin infusion pumps, jet injectors, and modern insulin pens.
- Insulin Syringes

Insulin syringes are most widely used and economical insulin delivery devices available today. Insulin syringes have undergone significant design improvements. Modern syringes enhance user experience, accuracy and patient comfort. Key features include thin needles, coated needles and calibrated gradation. Initially, syringes were large, heavy and made of reusable glass. However, advances in technology and materials science have led to improvements. Today’s syringes are lightweight, disposable and made of versatile plastics. These advancements have significantly improved insulin administration. They enhance safety, convenience and overall user experience. Modern insulin syringes cater to individual patient needs, with various needle gauges and syringe capacities available.
Advantages
- Insulin syringes are an economical option for insulin delivery.
- Insulin syringes are widely available at pharmacies and online.
- Insulin syringes are relatively simple to use, with a straightforward injection process.
- Insulin syringes are lightweight and portable, making them easy to carry.
- Insulin syringes allow for precise dosing, reducing the risk of overdose or under dose.
- Insulin syringes can be used with various types of insulin and can be easily adjusted to accommodate changing insulin needs.
Disadvantages
- Insulin injections can be painful, especially for those with needle phobia.
- Improper syringe handling and reuse can lead to infection.
- Disposable syringes contribute to medical waste and environmental concerns.
- Syringes may not provide the same level of precision as other insulin delivery devices, such as pumps.
- Used syringes require proper storage and disposal to prevent accidental needle sticks and infection transmission.
- Frequent injections can lead to emotional distress and decreased adherence to treatment.
- Insulin Infusion Pump
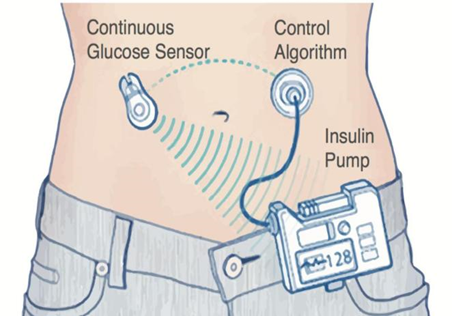
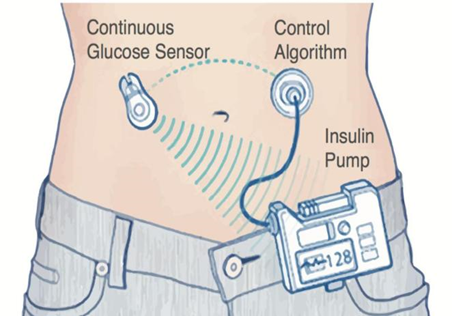
Insulin pumps provide continuous subcutaneous insulin infusion (CSII) therapy for diabetes management. The first CSII pumps were introduced in 1974. Modern pumps offer adjustable settings to meet individual patient needs. It consists of a Pump, reservoir, infusion set, cannula, control system, battery and user interface. The pump delivers insulin from the reservoir through the infusion set and cannula, inserted under the skin. The control system allows patients to program basal rates and bolus doses. These doses are delivered continuously throughout the day. The pump is powered by a battery and adjusted using the user interface. Insulin pumps provide a continuous supply of insulin.
Advantages
Insulin pumps offer improved glycaemic control, reduced hyperglycaemia risk and increased flexibility in insulin delivery, enhancing quality of life. These devices provide accurate and flexible insulin delivery, allowing tight control over plasma glucose levels. Ideal for patients requiring intensive insulin therapy, struggling with glucose management, or experiencing frequent hypoglycaemia, insulin pumps offer a valuable treatment option.
Disadvantages
Limitations and concerns include interruption of insulin delivery due to infusion set malfunction or pump dysfunction, and patient concerns about wearing a device constantly. Despite these limitations, insulin pumps are a valuable treatment option for patients with diabetes, offering improved glycaemic control, increased flexibility, and enhanced quality of life.
- Jet Injectors for Insulin Delivery

Jet injectors, introduced in 1980, are medical devices that utilize high-pressure jets of liquid to deliver insulin through the skin, eliminating the need for hypodermic needles. Powered by compressed air or gas, these devices offer a needle-free alternative for insulin administration. Jet injectors are designed with a dial-a-dose operation, allowing for precise control over insulin dosing. The devices can deliver insulin in half-unit increments, with a dose range of 2-50 units. The insulin is absorbed rapidly, minimizing the risk of subcutaneous infection.
Clinical Benefits
Studies have shown that jet injection therapy is associated with reduced anti-insulin antibody (AIA) production and improved postprandial glycaemia in patients with gestational diabetes. These findings suggest that jet injectors may be a valuable treatment option for individuals with diabetes.
Disadvantages
Jet injectors have several limitations, including pain, bruising and swelling at the injection site. Dosage inconsistencies, noise and limited availability are also concerns. Additionally, users must undergo training and perform regular maintenance tasks and the devices are often more expensive than traditional insulin delivery methods.
- Insulin Pen
Insulin pens have revolutionized insulin administration, offering a user – friendly alternative to traditional syringes. Introduced in 1987, insulin pens combine the insulin container and syringe into a single unit. Available in reusable and prefilled types, they offer convenience, flexibility and discretion. Insulin pens have become popular choice, potentially leading to better glycaemic control and lifestyle flexibility.
Advantages
Insulin pens offer a convenient and discreet way to manage diabetes, ideal for individuals with busy lifestyle. They provide accurate dosing, reducing the risk of overdose or underdose. With their pen like design, insulin pens are easy to use in public and their fine, short needles minimize pain and discomfort. Simple to operate, insulin pens feature a straightforward dial or button system for setting doses.
Disadvantages
Insulin pens have some limitations, including higher costs, proper needle disposal requirements, limited dose flexibility and the need for regular battery and cartridge replacements.
Novel Approaches Of Insulin Delivery
- Inhaled Insulin
Inhaled insulin delivery involves using a device to inhale insulin in the form of a fine powder or aerosol into the lungs, where it is rapidly absorbed into the bloodstream to help control blood sugar levels. It is designed as a needle-free alternative to traditional insulin injections.
How it works:

Inhaled insulin is delivered via a portable inhaler, allowing users to inhale insulin powder before meals. The insulin is absorbed into the bloodstream through the lungs, working similarity to fast -acting injected insulin to reduce Post – meal blood sugar spikes. With a faster onset than injected insulins, inhaled insulin start working within minutes, but its effects are shorter-lasting.
Common Devices for Inhaled Insulin:
Afrezza Inhaler:
The most widely used system currently is Afrezza, which delivers insulin as a powder. Afrezza’s inhaler is small and portable, and it uses pre-measured cartridges that are inserted into the device. The insulin is inhaled directly into the lungs at mealtime. The insulin starts acting quickly, and the device is typically used in conjunction with long-acting insulin for overall blood sugar control.
AeroDose Inhaler (discontinued):
Another inhaled insulin delivery system was AeroDose, which was developed by Novo Nordisk but was discontinued due to issues like lung complications and inconsistent absorption.
Advantages:
Needle-Free: Inhaled insulin removes the need for injections, which can be more convenient for some people.
Quick Onset: It works faster than long-acting insulin and can be used specifically around meal times to help control post-meal blood sugar spikes.
Convenience: The device is portable and relatively easy to use, making it a good option for those who prefer not to inject insulin multiple times a day.
Considerations:
Lung Function: Since it involves inhaling insulin, it may not be appropriate for individuals with lung conditions, such as asthma, COPD, or other respiratory issues.
Monitoring: People using inhaled insulin may need to monitor lung health regularly and may be advised to do pulmonary function tests to ensure the inhalation does not negatively affect their lungs.
Availability: Inhaled insulin is not as widely prescribed as injectable insulin, and the use of devices like Afrezza is not as common in all regions.
As with any diabetes management strategy, it’s important to discuss with your healthcare provider to determine if inhaled insulin is a suitable option based on your health, lifestyle, and diabetes needs.
- Oral Insulin
Oral insulin delivery is an emerging area of research aimed at providing an alternative to injectable insulin for people with diabetes. Unlike inhaled insulin, which is absorbed through the lungs, oral insulin is designed to be taken by mouth and absorbed through the digestive system. However, delivering insulin orally has been challenging because insulin is a protein, and when taken orally, it is typically broken down in the stomach before it can have any effect.
Challenges:
Digestive Breakdown: Insulin is a peptide hormone, and like most proteins, it would normally be digested in the stomach and rendered ineffective if taken orally.
Bioavailability: Achieving sufficient absorption of insulin into the bloodstream after oral administration has been a significant hurdle, as the insulin needs to bypass the digestive system’s breakdown processes.
Recent Developments:
While an oral insulin product hasn’t yet been widely available, there has been progress in the development of oral insulin formulations, including new methods to protect insulin from digestion and improve its absorption.
Oral Insulin Capsules (Oral Insulin Technology):
Researchers are exploring ways to encapsulate insulin in a form that can survive stomach acid and be absorbed effectively. Some technologies use capsules with enteric coatings, which protect the insulin from stomach acids and release it in the small intestine, where absorption is more efficient.
Technologies Under Development:
Insulin Inhalation Systems: While this is not strictly “oral,” some newer systems aim to bridge the gap by delivering insulin via the gastrointestinal tract indirectly. Nanoparticles and Microcapsules: Research is being conducted on using nanoparticles or microcapsules that could deliver insulin effectively across the digestive barrier.
Currently Available Oral Insulin:
One example of oral insulin being explored is Oral Insulin (Oral-Rapid®), which is under clinical trials. This formulation uses a combination of insulin and absorption enhancers to help insulin pass through the stomach lining. However, this technology is still in the experimental stages and has not yet received widespread approval or availability.
Potential Benefits:
Convenience: Oral insulin would provide a more convenient and less invasive method for insulin administration compared to injections or pumps.
Patient Preference: Many patients prefer oral medications to injections, so oral insulin could improve adherence to insulin therapy and quality of life.
Challenges and Considerations:
Effectiveness: It remains to be seen whether oral insulin can be as effective as injected insulin in managing blood sugar levels. Approval and Regulation: Many oral insulin formulations are still in the clinical trial phase, meaning they are not yet available to the general public. Cost and Accessibility: The development of these oral formulations could be costly, which may limit accessibility for some patients. In conclusion, while oral insulin delivery offers exciting potential and convenience, it remains an area of active research, with no widely available products yet on the market. If you’re interested in this option, it’s important to keep an eye on future developments and consult with your healthcare provider about the best options for managing your diabetes.
- Colonic Insulin Delivery
Colonic insulin delivery is an innovative method that utilizes the colon as an absorption site, bypassing the stomach and small intestine. This approach aims to overcome the limitations of oral insulin, as digestive process in the upper GI tract often breaks down insulin before absorption.
How Colonic Insulin Delivery Works:
Colonic insulin delivery system takes advantage of the colon’s unique characteristics, including reduced digestive enzymes and a rich blood supply. This allows insulin to remain intact and be absorbed into the bloodstream. Insulin is delivered via specially designed capsules or tablets with protective coatings and absorption enhancers, ensuring targeted release and absorption in the colon.
Challenges of Colonic Insulin Delivery:
Colonic insulin delivery faces several challenges, including ensuring controlled release of insulin in the colon, addressing variability in gastric emptying and transit time and optimising Bioavailability of insulin. Additionally, regulatory approval is pending, requiring extensive testing to determine safety, effectiveness and long-term outcomes.
Research and Development:
Several research teams and companies are working on developing colonic insulin delivery systems. Some of the approaches being explored include:
Microparticles and Capsules: These could be designed to resist stomach acid and release insulin in the colon, utilizing natural mechanisms to enhance absorption. Enzyme Inhibitors and Absorption Enhancers: Some formulations may combine insulin with substances that enhance its ability to cross the intestinal wall and enter the bloodstream.
Potential Advantages:
Non-Invasive: Like oral insulin, colonic insulin delivery is less invasive than injections, which could improve patient adherence and quality of life.
Targeted Delivery: Delivering insulin to the colon could allow for better absorption and more controlled release compared to other oral delivery methods.
Reduced Digestive Breakdown: Colonic delivery could reduce the issues of insulin being broken down in the stomach and small intestine, improving the bioavailability of the insulin.
Considerations:
Colonic insulin delivery is an experimental approach that requires further research to determine its effectiveness and technological maturity. While promising, it faces challenges in insulin absorption and controlled release. As with emerging therapies, ongoing research and consultation with healthcare providers are essential to assess its potential as a less invasive treatment options for diabetes.
- Nasal Insulin Delivery
Nasal insulin delivery is another innovative approach aimed at providing an alternative to traditional injectable insulin for individuals with diabetes. Instead of injecting insulin via needles or using insulin pumps, nasal insulin is delivered through the nose in the form of a spray or powder. It is absorbed through the nasal mucosa (the lining inside the nose) and enters the bloodstream more quickly than injected insulin.
How Nasal Insulin Delivery Works:
Nasal insulin is delivered as a fine powder, absorbed through the nasal mucosa’s rice blood supply. Insulin is then quickly absorbed into the bloodstream, acting similarly to rapid acting injectable insulin to control post – meal blood sugar levels. This method offers a convenient, injection free alternative for insulin administration.
Advantages of Nasal Insulin Delivery:
Needle-Free: One of the main advantages of nasal insulin is that it provides an alternative for people who dislike or fear injections, helping to improve adherence to treatment.
Rapid Onset: Nasal insulin has a faster onset of action compared to many injectable insulin, which can make it useful for controlling post-meal blood sugar spikes.
Convenience: The device used to administer nasal insulin is often small and portable, making it easier to use in various settings without the need for refrigeration or multiple injection sites.
Challenges and Considerations:
Nasal insulin delivery poses several challenges, including nasal irritation, limited use as mealtime insulin and absorption variability. Additionally, there is a risk of infection if the device is not properly cleaned. Regulatory approval and long-term effectiveness also require further research and clinical trials.
Currently Available Nasal Insulin:
Exubera (discontinued):
Exubera was one of the first commercially available nasal insulin products. It was introduced in the mid-2000s, but it was withdrawn from the market in 2007 due to low demand and concerns about side effects like lung irritation.
Afrezza (MannKind Corporation):
Afrezza is a modern, inhaled insulin product that is delivered via a small inhaler device (not strictly nasal but very similar in delivery route). It is rapid-acting insulin used around meals to help control post-meal blood sugar. Although it is inhaled through the mouth rather than the nose, it functions similarly in terms of providing a needle-free insulin delivery option. Afrezza is currently approved for use in the United States and some other countries for both type 1 and type 2 diabetes.
Potential Benefits:
Nasal insulin offers several benefits, including improved quality of life and treatment adherence by avoiding injections. It provides fast -acting blood sugar control and is a convenient, needle free alternative, reducing the psychological barrier to diabetes treatment.
- Buccal Insulin Delivery
Buccal insulin delivery refers to the administration of insulin through the mucous membrane inside the cheek (the buccal mucosa), where it is absorbed directly into the bloodstream. This method aims to provide an alternative to traditional insulin injections or other non-invasive methods like nasal or inhaled insulin.
How Buccal Insulin Delivery Works:
Buccal insulin is formulated as a gel, spray or tablet that’s absorbed through the buccal mucosa. The insulin enters the bloodstream quickly through the thin lining, bypassing digestive enzymes. This method is convenient, portable and less invasive than injections.
Advantages of Buccal Insulin Delivery:
Buccal insulin offers several benefits, including a needle free alternative, rapid onset of action and convenience. It’s easy to use discreetly, improving patient adherence. Additionally, buccal delivery avoids digestive breakdown, preserving insulin effectiveness.
Challenges and Considerations:
Buccal insulin faces challenges, including mucosal irritation, absorption variability due to individual factors and limited availability. Regulatory approval is pending and more research is needed to determine its long term effectiveness and safety.
Research and Development:
Research is ongoing into buccal insulin delivery, and various companies are exploring this method as a non-invasive, rapid-acting alternative to injections. Some of the key technologies being developed involve:
Buccal Insulin Sprays: These products are designed to deliver insulin in a fine mist, which is absorbed through the cheek lining.
Buccal Insulin Tablets or Gels: These are intended to dissolve in the mouth, allowing insulin to be absorbed through the buccal mucosa.
Potential Benefits:
Buccal insulin may improve quality of life, offer rapid acting blood sugar control and provide easy to use with discreet and convenient administration.
- Transdermal Insulin Delivery
Transdermal insulin delivery refers to the method of administering insulin through the skin without the need for injections, using patches or devices that facilitate the absorption of insulin into the bloodstream. This approach aims to provide an alternative to traditional needle-based insulin injections and could offer a more convenient, non-invasive way to manage diabetes.
How Transdermal Insulin Delivery Works:
Insulin Patches: The most common form of transdermal insulin delivery being explored involves insulin patches that are applied to the skin. These patches are designed to release insulin gradually over time, similar to how a traditional insulin pump works but without the need for a catheter or injection.
Microneedles: Another technology being investigated is the use of microneedles, which are tiny needles that create microchannels in the skin, allowing insulin to be absorbed into the bloodstream. These needles are much smaller and less invasive than traditional needles, offering a painless or minimally painful experience.
Electroporation and Iontophoresis: These techniques use electrical currents to temporarily open up the skin’s barrier, allowing insulin to penetrate more easily. Electroporation uses electrical pulses, while iontophoresis uses a low electrical charge to help move insulin through the skin.
Liposomes and Nanoparticles: Some transdermal delivery systems use liposomes or nanoparticles to carry insulin across the skin barrier. These small particles can encapsulate insulin and help it pass through the skin more efficiently.
Advantages of Transdermal Insulin Delivery:
Transdermal insulin delivery offers several advantages, including a needle free experience, convenience and discreet use. It provides continuous or long- acting insulin release, simplifying diabetes management. Additionally, it reduces the risk of injection site issues, such as pain and lipohypathy
Challenges and Considerations:
Challenges persist in transdermal insulin delivery, including skin absorption limitations due to the stratum corneum barrier. Consistency and effectiveness are also concerns, as absorption rates vary based on skin type, hydration and temperature. Additionally, high cost, limited availability and risk of skin irritation hinder widespread adoption of this technology.
Current Research and Development:
Several companies are actively developing transdermal insulin delivery systems, with some focusing on:
Transdermal Patches: These patches are designed to deliver a continuous or controlled release of insulin over a period of time. Research is ongoing to improve their effectiveness and to create patches that can provide both rapid-acting and long-acting insulin.
Microneedle Patches: These small, painless needles could deliver insulin through the skin by creating tiny channels. Microneedles are being explored for their ability to provide more accurate and efficient delivery than traditional patches.
Electroporation and Iontophoresis: These methods are being studied to help insulin penetrate the skin barrier more effectively, using small electrical currents.
Potential Benefits:
Transdermal insulin delivery may offer several benefits, including improved quality of life by reducing pain and stigma associated with injections. It may also be more convenient for individuals with active lifestyles and reduce injection site issues, such as scarring and lumps.
- Intra-Peritoneal (Intra-Portal)
Intra-peritoneal insulin delivery refers to the administration of insulin directly into the peritoneal cavity, which is the space surrounding the abdominal organs. This method leverages the peritoneum, the membrane that lines the abdominal cavity, as a site for insulin absorption. The concept behind intra-peritoneal delivery is based on the idea that insulin delivered directly into the peritoneal cavity might be absorbed faster and more efficiently than insulin administered subcutaneously (under the skin) or even through traditional methods.
How Intra-Peritoneal Insulin Delivery Works:
Intra – peritoneal insulin delivery involves administering insulin directly into the peritoneal cavity via a catheter, allowing for rapid absorption through the peritoneum’s rich blood supply. This method enabled faster insulin action compared to subcutaneous injections and has potential for continuous or semi- continuous delivery, offering a promising approaches for individuals with type 1 or 2 diabetes requiring dynamic insulin regimens.
Advantages of Intra-Peritoneal Insulin Delivery:
Intra- peritoneal insulin delivery offers several advantages, including rapid absorption, potential for continuous delivery and more precise control over blood sugar levels. This method could reduce the need for frequent injections, improve convenience and increase flexibility in basal and bolus insulin delivery. Additionally, it may provide better management of blood glucose, especially after meals or during periods of high insulin demand, ultimately leading to improved blood sugar control.
Challenges and Considerations:
Intra- peritoneal insulin delivery poses several challenges, including the need for invasive catheter placement, risk of infection and potential complications such as catheter blockage or peritonitis. Additionally, this method is still in the experimental stages, with limited availability and ongoing investigations into its long term safety and effectiveness.
Current Research and Applications:
Intra-peritoneal insulin delivery has primarily been explored in the context of experimental treatments and clinical trials. Some studies have investigated its use in people with type 1 diabetes, especially those who require very tight control of their blood glucose. Some experimental systems use peritoneal insulin pumps or implantable devices that allow for continuous insulin delivery directly into the peritoneal cavity. Additionally, peritoneal dialysis patients (those undergoing dialysis for kidney failure) have been a focus of some research because their access to the peritoneal cavity is already established, and this could be a convenient site for insulin delivery.
- Ocular Insulin Delivery (Eye)
How it works: Insulin is delivered through the eye via a formulation that is absorbed through the ocular tissues (cornea or conjunctiva).
Advantages: Provides a non-invasive delivery route that bypasses the digestive system.
Challenges: This method is still in early stages of research, and the challenges of developing a safe and effective ocular formulation for insulin are considerable.
- Implantable Insulin Devices
How it works: These devices are surgically implanted under the skin and can deliver insulin continuously. Some devices can release insulin in response to changing glucose levels.
Advantages: Offers a more continuous and less invasive alternative to frequent injections.
Challenges: Requires surgical implantation and may carry risks of infection or device malfunction. It’s also limited by the need for maintenance and possible removal.
CONCLUSION
Despite significant advancements in the development of novel insulin delivery systems, traditional injection methods using syringes and insulin pens remain the most widely accepted and utilized. However, emerging technologies such as oral insulin and inhalation-based delivery systems hold great promise. If successfully developed and implemented, these innovative approaches are poised to revolutionize insulin administration, potentially replacing existing dosage forms and transforming the lives of individuals with diabetes.
REFERENCES
- An overview of oral insulin delivery strategies (OIDS) Author links open overlay panelGayatri Iyer a, Sathish Dyawanapelly a, Ratnesh Jain b, Prajakta Dandekar a https://www.sciencedirect.com/science/article/abs/pii/S0141813022006146#preview-section-references
- Tripathi KD, Essentials of Medical pharmacology, 5th edition, 2004, New Delhi, pp. 235-236., 246.
- Tyagi P, Indian Journal of Pharmacology” Insulin Delivery Systems: Present Trends and the Future Direction”, 2002; pp. 379-389.
- Insulin drug delivery systems: A review Amish Panchal*, Viral Shah, U.M. Upadhyay, Amish Panchal et al., Int. J. Res. Pharm. Sci., 2(4), 2011, 484-492. https://www.researchgate.net/publication/228835145_Insulin_drug_delivery_systems_A_review
- Insulin delivery methods: Past, present and future Rima B. Shah1, Manhar Patel2, David M. Maahs, Viral N. Shah. https://www.researchgate.net/publication/294732711_Insulin_delivery_methods_Past_present_and_future.
- https://idf.org/
- Recent advancements on novel approaches of insulin delivery Author links open overlay panelSandip Karmakar a, Manas Bhowmik b, Bibek Laha c, Sreejan Manna. https://doi.org/10.1016/j.medntd.2023.100253.
- File:Standard insulin syringe. JPG https://en.m.wikipedia.org/wiki/File:Standard_insulin_syringe. JPG
- AN OVERVIEW OF INHALED INSULIN https://www.adces.org/education/danatech/insulin-medicine-delivery/insulin-medicine-delivery-101/inhaled-insulin.
- Study: Insulin Pump Better Than Injections. https://www.ipag.co.uk/study-insulin-pump-better-than-injections/amp/
- Study of Key Commodity Aspects of Injection Pens for Insulin Administration and Needles for Them, T. Diadiun Published 21 December 2016.
- D.R. Whiting, L. Guariguata, C. Weil, J. Shaw IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030.


 Unnati Patel*
Unnati Patel*



 10.5281/zenodo.14850674
10.5281/zenodo.14850674