Abstract
Barleria cuspidata, a plant in the Acanthaceae family, is known for its medicinal properties, including anti-diabetic and anti-asthmatic properties. Studies suggest these effects are attributed to the use of antibiotics and anti-diabetic extracts. However, there is limited research on other species. This review examines the phytochemistry and biological characteristics of Barleria, focusing on its traditional uses. betic extracts. Diabetes mellitus, a global health issue, affects 285 million people, 6.4% of the adult population, due to obesity and aging. With 50% of presumed This chapter discusses various forms of diabetes, their associated complications, emerging therapies, and current management and treatments, including immune system damage, periodontal disease, retinopathy, nephr The opathy, neuropathy, cardiovascular disorders, and diabetic foot. diabetics not receiving a diagnosis for ten years, the true prevalence of diabetes is expected to be high.
Keywords
anti-asthmatic properties, anti-diabetic, emerging therapies, retinopathy.
Introduction
A chronic metabolic condition known as diabetes mellitus is typified by high blood glucose (also known as blood sugar) levels.[1]. The most prevalent kind of diabetes, known as type 2 diabetes, primarily affects adults and is brought on by insu?cient or resistant insulin production[2]. Frequent urination, increased thirst, and increased appetite are common symptoms[3]. Diabetes can have a number of consequences if it is not addressed. Death, hyperosmolar hyperglycemia condition, and diabetic ketoacidosis are examples of acute complications [4]. Cardiovascular illness, stroke, chronic kidney disease, foot ulcers, nerve damage, ocular damage, and cognitive decline are examples of severe long-term consequences [5].The most typical Type 1 diabetes, which affects 5% of the population, is an autoimmune disease, while type 2 diabetes, which affects 95% of people, is linked to obesity[6]. Pregnancy is the primary cause of gestational diabetes; other types of the disease are extremely uncommon and result from a single gene mutation[7].. Diabetes does not have a treatment. But you can live a long, healthy life if you receive the right care and alter your lifestyle[8].
Pathophysiology:
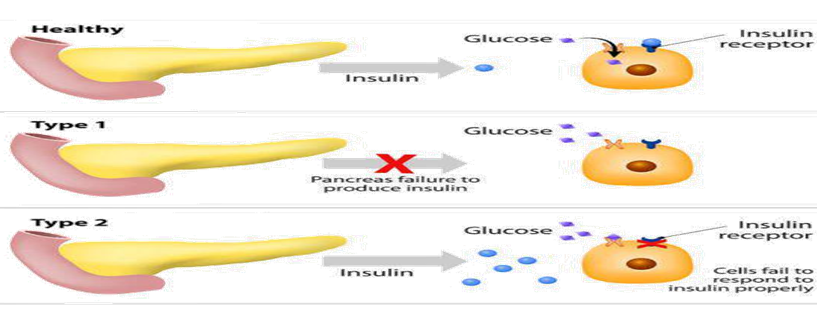
Types Diabetes comes in two primary forms: Type 1 and Type 2.[9]
Diabetes Type 1
It happens as a result of i
njury to the pancreatic beta cells, which produce insulin[10]. When diabetes type 1 occurs, the pancreas produces insu?cient or no insulin, which prevents sugar from entering the body's cells to be used as fuel[11]. Insulin injections are necessary for people with Type 1 diabetes to manage their blood sugar levels[12]. Diabetes can strike anyone at any age, although among those under 30, type 1 is the most frequent type[13]. Type 1 diabetes affects ten percent of those with diabetes[14].
Diabetes Type 2
The pancreas produces insulin in this type of situation, but either insu?cient amounts or improper insulin function are produced. Type 2 diabetes affects nine out of ten diabetic patients[15]. This kind primarily affects adults over 40, though it can happen to children as well if certain risk criteria are met[16]. Exercise, weight control, and diet can occasionally be used to manage type 2 diabetes. [17] However, further therapy options include insulin injections or oral glucose-lowering drugs that are taken orally[18].
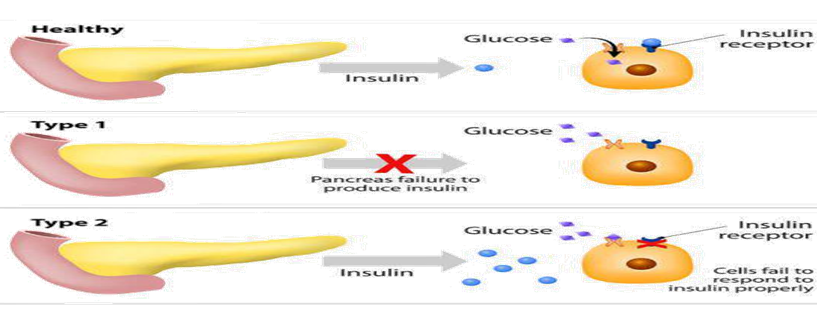
Fig 1.1Types Of Diabetes Mellitus
? Symptoms
An increase in blood sugar is the cause of diabetes symptoms. Overall Symptoms[19]
? Among the common signs of diabetes are: increased thirst
heightened hunger reduction in weight a lot of urinating hazy vision extreme tiredness non-healing sores[20]
Men's Symptoms
Men with dbetes may experience low physical strength, erectile dysfunction (ED), and weakened sex drive in addition to other typical symptoms of the disease.[21]
Women's Symptoms
Symptoms of diabetes in women can also include dry, itchy skin, yeast infections, and urinary tract
infections.
Diabetes Type 1[22]
Type 1 diabetes symptoms can include:
Intensive thirst
heightened appetite
accidental loss of weight
a lot of urinating
hazy vision
fatigue [23]
Diabetes Type 2
Type 2 diabetes symptoms can include:
heightened appetite
heightened desire
elevated urination
hazy vision
fatigue
wounds that take a while to heal[24]
Also, it might result in recurrent infections. This is because the body finds it more di?cult to mend when glucose levels are elevated[25].
Risk Factor : The incidence of diabetes mellitus has surged worldwide, leading to an intensifying public health concern[26]. The disease itself actually begins when a number of risk factors come together[27]. The main risk factors for pre diabetes and DM are genetics, environment, loss of the first phase of insulin launch, sedentary lifestyle, lack of exercise, smoking, alcohol consumption, dyslipidemia, diminished ?-cell sensitivity, hyper insulinemia, and increased glucagon activity[28]. These factors seem to be important in the development of insulin resistance or non functionality, which in turn leads to the progression of the disease. According to WHO (2011), T2DM affects 90% of patients and is mostly caused by increased body weight[29]. Adults who are overweight and suffer from obstructive sleep apnea and sleep disorders are at a common risk for developing insulin resistance and glucose sensitivity, which together lead to prediabetes and ultimately type 2 diabetes[30]. It is believed that a diet high in GI and low in fiber has a positive correlation with the onset of diabetes. Free fatty acids have been shown to be a significant mediator between insulin resistance and type 2 diabetes. The most harmful aspect of soft drinks is their high fructose content, which has metabolic consequences on the liver and can lead to obesity and a rise in body mass index (BMI), both of which can result in type 2 diabetes. Being overweight results in increased adipose tissue bulk and increased adipokine and resistin production, all of which are dysregulated and cause the development of type 2 diabetes. Numerous research have looked into the relationship between hyperuricemia and the onset of T2DM. Insulin resistance and hyperuricemia cause ? cell activity to be activated from its compensatory state[31]. In a different study, patients with T2DM and obesity exhibited higher C-peptide levels when compared to four study groups (control, T2DM: with and without obesity, and T1DM)[32]. The behavior of uric acid seems to be tightly associated with the function of ? cells.[33] High serum uric acid was linked to an increased risk of type 2 diabetes in a different follow-up trial, regardless of obesity, dyslipidemia, or hypertension[34]. Still, uric acid has been found to mediate systemic inflammation and endothelial dysfunction as well as to play a part in cytokine release[35]. A favorable correlation between the incidence of type 2 diabetes and uric acid plasma concentration was observed in a Chinese population study[36]. After accounting for metabolic syndrome, the connection was somewhat diminished, indicating that metabolic syndrome, in particular insulin resistance, may have played a role in mediating the link between hyperuricemia and diabetes.[37] Previous research has demonstrated that the formation of reactive oxygen species (ROS) inside the metabolic syndrome's complex cellular milieu, which is linked to oxidative stress, can cause uric acid's antioxidant characteristics to change into a pro-oxidant state . Additionally, there's a chance that this will have a negative impact on endothelial function and trigger a pro inflammatory response, both of which are linked to newly diagnosed T2DM[38].
Causes:
It is also known as Etiology
The Greek term "aetiologia" is where the word "etiology" originates.Therefore, etiology is described since it is the study of determining the causes and origins of illness. It comprises Currently, the juvenile-onset (insulin-dependent) variety is thought to have a partially autoimmune etiology.[39]
2. Viruses may also have a role in the genesis of polygenic diseases such as coxsackie B.[40]
3. It has been demonstrated that the German measles virus and epidemic parotitis both cause morphologic alterations in the islet-cell structure.[41]
4. There is debate on the genetic component in the etiology of polygenic illness. A genetic characteristic most likely renders an individual's exocrine gland more susceptible to one of the above viruses. The reasons for polygenic illness The disturbances or abnormalities in the ß cell's gluco-receptor that cause them to react to elevated aldohexose concentrations or relative ß cell deficit. Either way, there is a reduction in the release of hypoglycaemic agents, which may lead to ß cell failure the theory that minor vascular disease causes neural drive and, as a result, the direct effects of hyperglycemia on the metabolism of vegetative cells[42].
1. Diminished insulin sensitivity in peripheral tissues: a decrease in the hypoglycemic agent receptors' range and their "down regulation." Several hypersensitized and hyperinsulinemia patients, despite being conventionally glycaemic, are also linked to dyslipidemia, hyperuricemia, and abdominal obesity. Consequently, there is some resistance to hypoglycemic agents, especially when it comes to the liver, muscle, and fat. Angiopathy has been associated with hyperinsulinemia.
2.relative hypoglycemia; the ß cells lag behind due to internal secretion (glucagon) and other factors that lead to hyperglycemia. According to two views, there are debatable anomalies in the metabolism of nitric oxide that result in altered perineural blood flow and nerve damage.
3. Various unusual forms of diabetes mellitus (DM) include those caused by particular genetic flaws (type 3), such as diabetes mellitus of the young (MODY), various endocrine illnesses, pancreatectomy, and physiological state diabetes mellitus (GDM).
Polygenic disease mellitus is brought on by a particular receptor imbalance. Certain receptors include the PPAR? (peroxisome proliferator activated) receptor, the ?-glycosidase receptor, the beta3 (ß3) ardent receptor, and the dipeptidyl protease IV enzyme, among others.
The polyol pathway, protein kinase C, advanced glycation end products, and oxidative stress are the main topics of current research on diabetes pathophysiology.
Complications:
With improvements in the treatment of diabetes mellitus, there is growing evidence of an elevated risk and burden of an additional group of less well-known consequences associated with the disease.With improvements in the treatment of diabetes mellitus, there is growing evidence of an elevated risk and burden of an additional group of less well-known consequences associated with the disease. As the death rate from vascular diseases has decreased, the two main causes of death for those with diabetes mellitus are now dementia and cancer. [43] Diabetes mellitus is linked to a higher risk of cancer in general and female-specific cancer in particular as well as tumors of the gastrointestinal tract.
Diabetes mellitus patients had higher rates of hospitalization and death from a variety of infections, such as COVID-19, pneumonia, foot, and kidney infections. Diabetes mellitus patients frequently experience depression, obstructive sleep apnea, nonalcoholic fatty liver disease, and cognitive and functional impairment. The therapy of diabetes mellitus should be approached holistically since new problems continue to arise, and screening recommendations should take diseases like depression, liver disease, and cancer into account. Barleria Cuspidata used for Management of DM : The study details the antidiabetic properties of an alcoholic extract made from the leaves of the traditional Ayurvedic plant B. prionitis Linn. B. prionitis has been shown by phytochemical study to include flavonoids, tannins, sterols, and saponins. Well-known bioactive antidiabetic principles include flavonoids, phenolics, tannins, and sterols/triterpenoids. It is also known that in rats with alloxan diabetes, flavonoids can repair damaged beta cells. Alloxan was utilized as a diabetogen in this investigation. By partially damaging the pancreatic ?-cells and producing reactive oxygen species, it causes diabetes. The potential of an alcoholic extract of roots and leaves to prevent diabetes was evaluated. In diabetic rats induced with alloxan, the blood glucose level was significantly reduced by the alcoholic leaf extract. There was a non-significant drop in the alcoholic root extract. However, a therapeutic benefit of both therapies is that they did not cause hypoglycemia in normal rats. Rats with diabetes caused by alloxan showed a reduction in insulin levels. Upon therapy, the leaf extract reversed this effect. This could mean that the leaf extract is more effective in regenerating the islet cells and that the group treated with leaf extract had a more pronounced reduction in the alloxan-induced degenerative alterations than the group treated with root extract. It can be deduced that the extract has the ability to improve the glucose-dependent insulin release from the pancreatic beta cells and thereby lower the blood glucose level only in rats that have been induced with alloxan. However, the same treatment did not raise the serum insulin level in normoglycemic rats. Extract functions in a manner that is strikingly similar to biguanides, another name for "euglycemics." Biguanides do not cause hypoglycemia; instead, they return the raised blood sugar level to normal. Biguanides have a positive impact on the lipid profile, i.e., a reduction in TGs, and they also enhance peripheral blood glucose uptake and utilization. B. prionitis has been shown to be strong hepatoprotective in a study that showed a highly substantial reduction in TGs. This implies that the examined herb's mechanism is comparable to biguanides'.
Glycogen content falls in diabetes as a result of increased glycogenolysis, and insulin shortage impairs the liver's normal Glycogen content falls in diabetes as a result of increased glycogenolysis, and insulin shortage impairs the liver's normal ability to synthesize glycogen. The diabetic control group was found to have reduced liver glycogen levels. When alcoholic leaf extract was administered, there was a noticeable rise in the amount of liver glycogen, which may have been caused by an increase in insulin. Reversal of the depletion is indicative of a reduction in the severity of diabetes and may serve as a barometer for the test drug's antidiabetic properties. Proteins have the universal ability to bind non-enzymatically to nearby glucose or other carbohydrates. The amount of sugar present in the surrounding medium directly relates to the degree of glycation.
As a result, measurement of glycosylated hemoglobin (HbA1c) best corresponds with the degree of glycemia and provides an accurate picture of the mean plasma glucose concentration during this time. A 1% shift in HbA1c would correspond to a roughly 30% change in blood glucose. When leaf extract was used, the treated rats showed a substantial decrease (P<0>
Rats given alloxan to induce diabetes showed a notable decrease in body weight. Diabetes patients' weight decreases as a result of their constant glucose excretion as well as a reduction in peripheral glucose and glycogen synthesis uptake
When alcoholic leaf extract was administered, the weight loss was more significantly stopped than when root extract was. The test medication, alcoholic leaf extract, may have potential as an antidiabetic based on all of the aforementioned observations[44].
CONCLUSION: Barleria cuspidata extracts, extracted in methanol and chloroform, have significant antidiabetic, comparable to glibenclamide medication. Potential diabetes treatment applications involve separating active
ingredients. and describing activity componentsResearch findings indicate that the alcoholic leaf extract of B. prionitis may serve as a valuable supplement to the current therapeutic toolkit for the management of diabetes. At the cellular and molecular level, more research may be done to help clarify its mechanism in more depth.
REFERENCES
- Wang RZ, Zhang WS, Jiang CQ, Zhu F, Jin YL, Xu L. Inflammatory age and its impact on age-related health in older Chinese adults. Archives of Gerontology and Geriatrics. 2024 Oct 1;125:105476.
- Rachdaoui N. Insulin: the friend and the foe in the development of type 2 diabetes mellitus. International journal of molecular sciences. 2020 Mar 5;21(5):1770.
- Gregory Ns. Excessive Thirst, Hunger, And Urination In Diabetes. Introduction to Clinical Pharmacology: From Symptoms to Treatment. 2023 Sep 14:304.
- Gosmanov AR, Gosmanova EO, Kitabchi AE. Hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Endotext [Internet]. 2021 May 9.
- Mauricio D, Alonso N, Gratacòs M. Chronic diabetes complications: the need to move beyond classical concepts. Trends in Endocrinology & Metabolism. 2020 Apr 1;31(4):287-95.
- Frazzei G, van Vollenhoven RF, de Jong BA, Siegelaar SE, van Schaardenburg D. Preclinical autoimmune disease: a comparison of rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis and type 1 diabetes. Frontiers in immunology. 2022 Jun 30;13:899372.
- Li LM, Jiang BG, Sun LL. HNF1A?From Monogenic Diabetes to Type 2 Diabetes and Gestational Diabetes Mellitus. Frontiers in Endocrinology. 2022 Mar 1;13:829565.
- American Diabetes Association. 4. Lifestyle management: standards of medical care in diabetes—2018. Diabetes care. 2018 Jan 1;41(Supplement_1):S38-50.
- Eizirik DL, Pasquali L, Cnop M. Pancreatic ?-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nature Reviews Endocrinology. 2020 Jul;16(7):349-62.
- Sharma RB, Landa-Galván HV, Alonso LC. Living dangerously: protective and harmful ER stress responses in pancreatic ?-cells. Diabetes. 2021 Nov 1;70(11):2431-43.
- Lema-Pérez L. Main organs involved in glucose metabolism. Sugar intake-risks and benefits and the global diabetes epidemic. 2021 Sep 1:1-5.
- Perkins BA, Sherr JL, Mathieu C. Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation. Science. 2021 Jul 30;373(6554):522-7.
- Ziegler AG. The countdown to type 1 diabetes: when, how and why does the clock start?. Diabetologia. 2023 Jul;66(7):1169-78.
- Green A, Hede SM, Patterson CC, Wild SH, Imperatore G, Roglic G, Beran D. Type 1 diabetes in 2017: global estimates of incident and prevalent cases in children and adults. Diabetologia. 2021 Dec;64:2741-50
- Rachdaoui N. Insulin: the friend and the foe in the development of type 2 diabetes mellitus. International journal of molecular sciences. 2020 Mar 5;21(5):1770.
- Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, Butalia S, Leung AA, Harris KC, Cloutier L, Zarnke KB. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Canadian Journal of Cardiology. 2020 May 1;36(5):596-624.
- Magkos F, Hjorth MF, Astrup A. Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nature Reviews Endocrinology. 2020 Oct;16(10):545-55.
- Feingold KR. Oral and injectable (non-insulin) pharmacological agents for the treatment of type 2 diabetes. Endotext [Internet]. 2022 Aug 26.
- Alam S, Hasan MK, Neaz S, Hussain N, Hossain MF, Rahman T. Diabetes Mellitus: insights from epidemiology, biochemistry, risk
- Kwakye IN. Lived Experiences of Diabetics Living in Rural Areas in the Eastern Region (Doctoral dissertation, University of Cape Coast)
- Defeudis G, Mazzilli R, Tenuta M, Rossini G, Zamponi V, Olana S, Faggiano A, Pozzilli P, Isidori AM, Gianfrilli D. Erectile dysfunction and diabetes: A melting pot of circumstances and treatments. Diabetes/metabolism research and reviews. 2022 Feb;38(2):e3494.
- Dwivedi M, Pandey AR. Diabetes mellitus and its treatment: an overview. J Adv Pharmacol. 2020;1(1):48-58.
- Baynes K. Diabetes Mellitus, Obesity, Lipoprotein Disorders and other Metabolic Diseases. InMedicine for Finals and Beyond 2022 Jun 19 (pp. 429-470).CRC Press.
- Anandhanarayanan A, Teh K, Goonoo M, Tesfaye S, Selvarajah D. Diabetic neuropathies. Endotext [Internet]. 2022 Mar
- Tang L, Chang SJ, Chen CJ, Liu JT. Non-invasive blood glucose monitoring technology: a review. Sensors. 2020 Dec 4;20(23):6925.
- Koliaki C, Dalamaga M, Liatis S. Update on the obesity epidemic: after the sudden rise, is the upward trajectory beginning to flatten?. Current Obesity Reports. 2023 Dec;12(4):514-27.
- Milardi D, Gazit E, Radford SE, Xu Y, Gallardo RU, Caflisch A, Westermark GT, Westermark P, Rosa CL, Ramamoorthy A. Proteostasis of islet amyloid polypeptide: a molecular perspective Pof risk factors and protective strategies for type II diabetes. 28.Chemical Reviews. 2021 Jan 11;121(3):1845-93.
- Khan RM, Chua ZJ, Tan JC, Yang Y, Liao Z, Zhao Y. From pre-diabetes to diabetes: diagnosis, treatments and translational research. Medicina. 2019 Aug29;55(9):546.
- Zhao X, An X, Yang C, Sun W, Ji H, Lian F. The crucial role and mechanism of insulin resistance in metabolic disease. Frontiers in endocrinology. 2023Mar 28;14:1149239.
- Akset M, Poppe KG, Kleynen , Bold I, Bruyneel M. Endocrine disorders in obstructive sleep apnoea syndrome: A bidirectional relationship. Clinical Endocrinology. 2023 Jan;98(1):3-13.
- Gong M, Wen S, Nguyen T, Wang C, Jin J, Zhou L. Converging relationships of obesity and hyperuricemia with special reference to metabolic disorders and plausible therapeutic implications. Diabetes, Metabolic Syndrome and Obesity. 2020 Mar 30:943-62.
- Esze R, Barna S, Fülöp P, Kempler P, Mikó M, Páll D, Paragh G, Somodi S, Emri M, Képes Z, Garai I. C-peptide: an essential ally in microvascular complications of type 2 diabetes mellitus and obesity. Diabetology & Metabolic Syndrome. 2024
- 3.Lu J, He Y, Cui L, Xing X, Liu Z, Li X, Zhang H, Li H, Sun W, Ji A, Wang Y. Hyperuricemia predisposes to the onset of diabetes via promoting pancreatic ?-cell death in uricase-deficient male mice. Diabetes. 2020 Jun 1;69(6):1149-63.
- Son YB, Yang JH, Kim MG, Jo SK, Cho WY, Oh SW. The effect of baseline serum uric acid on chronic kidney disease in normotensive, normoglycemic, and non-obese individuals: A health checkup cohort study. Plos one. 2021 Jan 27;16(1):e0244106.
- Russo E, Verzola D, Cappadona F, Leoncini G, Garibotto G, Pontremoli R, Viazzi F. The role of uric acid in renal damage-a history of inflammatory pathways and vascular remodeling. Vessel Plus. 2021;5(15):2574-1209.
- Ji P, Zhu J, Feng J, Li H, Yu Q, Qin H, Wei L, Zhang J. Serum uric acid levels and diabetic kidney disease in patients with type 2 diabetes mellitus: A dose-response meta-analysis. Primary care diabetes. 2022 Jun 1;16(3):457-65.
- Bovolini A, Garcia J, Andrade MA, Duarte JA. Metabolic syndrome pathophysiology and predisposing factors. International journal of sports medicine. 2021 Mar;42(03):199-214.
- Gora IM, Ciechanowska A, Ladyzynski P. NLRP3 inflammasome at the interface of inflammation, endothelial dysfunction, and type 2 diabetes. Cells. 2021 Feb 3;10(2):314.
- Hero C. Epidemiological Aspects on Assessing and Treating Dyslipidemia in Type 1 Diabetes.
- Carré A, Vecchio F, Flodström-Tullberg M, You S, Mallone R. Coxsackievirus and type 1 diabetes: diabetogenic mechanisms and implications for prevention. Endocrine reviews. 2023 Aug;44(4):737-51.
- Kumar R, Saha P, Kumar Y, Sahana S, Dubey A, Prakash O. A review on diabetes mellitus: type1 & Type2. World Journal of Pharmacy and Pharmaceutical Sciences. 2020 Aug 2;9(10):838-50.
- Azova. S, Rapaport R, Wolfsdorf J. Brain injury in children with diabetic ketoacidosis: review of the literature and a proposed pathophysiologic pathway for the development of cerebral edema. Pediatric diabetes. 2021 Mar;22(2):148-60.
- Wang X, Ma H, Li X, Heianza Y, Manson JE, Franco OH, Qi L. Association of cardiovascular health with life expectancy free of cardiovascular disease, diabetes, cancer, and dementia in UK adults. JAMA Internal Medicine. 2023 Apr 1;183(4):340-9.
- Gebremeskel L, Beshir Tuem K, Teklu T. Evaluation of antidiabetic effect of ethanolic leaves extract of Becium grandiflorum Lam.(Lamiaceae) in streptozotocin-induced diabetic mice. Diabetes, Metabolic Syndrome and Obesity. 2020 May 4:1481-9


 Adsul Samruddhi *
Adsul Samruddhi *
 Pandit Ashwini
Pandit Ashwini
 Dahale Raju
Dahale Raju
 10.5281/zenodo.14249778
10.5281/zenodo.14249778