Abstract
Objective. Uterine cancer, primarily comprising endometrial carcinoma, is a significant gynecological malignancy affecting women globally, It often presents with abnormal vaginal bleeding, particularly in postmenopausal women. Risk factors include obesity, hormonal imbalances, age, and genetic predispositions, such as Lynch syndrome. Diagnosis typically involves pelvic examinations, imaging studies, and biopsy. Treatment strategies include surgery, radiation therapy, and hormone therapy, tailored to the cancers stage and histology. Recent advancements in targeted therapies and immunotherapy are showing promise. Early detection and individualized treatment plans are crucial for improving outcomes in uterine cancer patients.
Keywords
uterine cancer, endometrial cancer, uterine sarcoma, prevention, diagnosis, treatment.
Introduction
Cancer is the uncontrolled growth of cells, which may disrupt normal tissue function and cause potential harm to the body. Most of cancers form tumors but not all tumors are cancerous. Benign or noncancerous tumors are not spread to other body parts and do not create new tumors. Malignant or cancerous tumors crowed out healthy cells, interfere with body functions and draw nutrients from body tissue. Uterine cancer, primarily encompassing endometrial cancer, is one of the most prevalent gynaecologic malignancies worldwide. It typically arises from the endometrium, the inner lining of the uterus, and is most commonly diagnosed in postmenopausal women. The incidence of uterine cancer has been increasing, influenced by various risk factors such as obesity, hormonal imbalances, diabetes, and genetic predispositions, particularly in women with a family history of certain hereditary syndromes. Common symptoms include abnormal uterine bleeding, pelvic pain, and changes in menstrual patterns, which often prompt individuals to seek medical evaluation. Early diagnosis is crucial, as the prognosis is significantly better when the disease is detected in its initial stages.
Treatment usually involves surgical intervention, including hysterectomy, often accompanied by radiation or hormonal therapies based on the cancer's stage and type. Research continues to explore the molecular mechanisms underlying uterine cancer, paving the way for more targeted and personalized treatment options. Understanding uterine cancer is vital for improving prevention strategies, enhancing early detection, and optimizing therapeutic approaches, ultimately aiming to reduce mortality and improve quality of life for affected individuals.
Causes of cancer -
Cancer is a complex group of diseases characterized by the abnormal reproduction of genetically damaged cells that can spread throughout the body, causing damage to tissues and organs. The causes of cancer can be categorized into genetic and environmental factors. Here are some key causes:
1. Genetics
Inherited genetic mutations can significantly increase cancer risk. Certain types of cancer, like breast, colon, and ovarian cancer, have strong hereditary links.
2. Tobacco
Tobacco use is a major risk factor for several cancers, including lung and throat cancer. It contains carcinogens that can damage DNA, leading to cancer and other serious health issues.
3. Diet
A diet high in processed foods, red meat, sugar, and trans fats may elevate the risk of cancers, particularly colorectal and stomach cancers.
4. Lack of Exercise
While lack of exercise doesn’t directly cause cancer, it can contribute to obesity, which increases the risk of developing various cancers, including breast and colon cancer. Regular physical activity supports immune function and reduces inflammation.
5. Alcohol
Excessive alcohol consumption is linked to several cancers. While the exact mechanism isn’t fully understood, it’s believed to involve toxic compounds produced during alcohol metabolism. Limiting alcohol to one drink per day is recommended to reduce cancer risk.
6. Radiation
High levels of radiation exposure, such as ultraviolet rays from the sun and radon gas, can damage cells. Sensitivity to radiation varies, with children and adolescents being more susceptible than adults.
7. Air Pollution
Air pollution is associated with several cancers, including lung, breast, and liver cancer. Common sources include vehicle exhaust, burning trash, and emissions from power generation.
8. Infections
Certain infections can increase cancer risk. For example, Hepatitis B and C are linked to liver cancer, while Human Papillomavirus (HPV) is associated with cervical and vaginal cancers.
9. Household Chemicals
Exposure to various household chemicals, such as benzene, asbestos, and arsenic, can contribute to cancer development.
Symptoms of cancer
- Fatigue.
- Fever that occurs mostly at night.
- Loss of appetite.
- Night sweats.
- Persistent pain
- Skin changes particularly moles that changes shape and size or new moles.
- Unexplained wight loss.
- Blood in pee or stool.
- Coughing up blood.
- New lumps or bumps
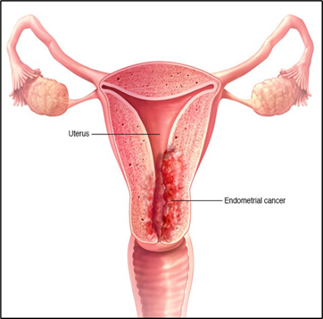
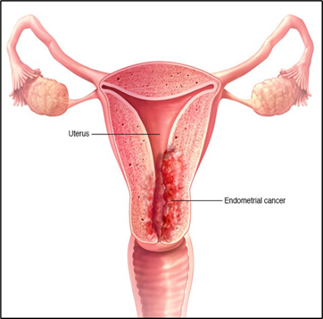
Figure 1
Uterine Cancer
Uterine cancer originates in the uterus, the pear-shaped organ where a baby develops during pregnancy. The two primary types of uterine cancer are:
1. Endometrial Cancer
Endometrial cancer is the most common form of uterine cancer, starting in the endometrium, the inner lining of the uterus.
Characteristics:
Primarily affects postmenopausal women.
Often diagnosed at an early stage due to symptoms like abnormal vaginal bleeding.
Early diagnosis allows for effective treatment, typically through surgical remova
Epidemiology:
It is the most common cancer of the female genital tract and the fourth most common cancer overall among women in the U.S., with about 61,880 new cases and 12,160 deaths reported annually.
Globally, the incidence peaks between ages 65 and 75, with North America showing the highest rates.
The worldwide incidence of endometrial cancer has increased by over 130% in the past 30 years.
In India, the incidence is lower compared to developed countries, with 16,413 cases reported in 2020 and a mortality rate of 6,385.
Symptoms of endometrial cancer: Endometrial cancer often presents with specific symptoms, particularly in its early stages. Awareness of these symptoms is crucial for early detection. Common symptoms include:
- Abnormal Vaginal Bleeding.
- Unusual bleeding between periods.
- Heavy or prolonged menstrual bleeding.
- Bleeding after menopause.
- Pelvic Pain:
- Pain or discomfort in the pelvic area that is persistent or worsening.
- Unexplained Weight Loss:
- Significant weight loss without changes in diet or exercise.
- Changes in Menstrual Cycle:
- Irregular menstrual cycles or changes in the pattern of bleeding.
- Pain During Intercourse:
- Discomfort or pain during sexual activity.
- Unusual Vaginal Discharge:
- Watery or blood-stained discharge that is not related to menstruation.
- Fatigue:
- Persistent tiredness or lack of energy that is not typical.
Stages of endometrial cancer:
Stages I: In stage I, cancer is found in the uterus only . Stage I is divided into stages IA and IB .
Stage 1A: Cancer is in the endometrium only or less than halfway through the myometrium (muscle layer of the uterus).
Stage IB: Cancer has spread halfway or more into the myometrium.
Stage II: In stage II cancer has spread into connective tissue of the cervix, but has not spread outside the uterus.
Stage III: In stage III cancer has spread beyond the uterus and cervix, but has not spread to the pelvis. Stage III is divided into stages IIIA, IIIB and IIIC.
Stage IIIA: Cancer has spread to the outer layer of the uterus or to the fallopian tubes,ovaries and ligaments of the uterus .
Stage IIIB: Cancer has spread to the vagina or parametrium (connective tissue and fat around the uterus)
Stage IIIC: Cancer has spread to lymph nodes in the pelvis or around the arota (largest artery in the body, which carries blood away from the heart).
Stage IV: In stage IV, cancer has spread beyond the pelvis . Stage IV is divided into stages IVA and IVB.
Stage IVA: Cancer has spread to the bladder and bowel wall.
Stage IVB: Cancer has spread to other parts of the body beyond the pelvis , including the abdomen or lymph nodes in the groin.
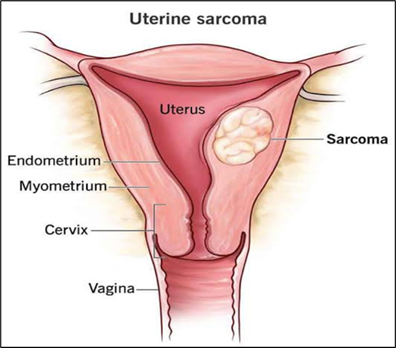
2. Uterine sarcoma –
Uterine sarcoma is much rare type of uterine cancer that forms in the muscles and connective tissue of the uterus . Uterine sarcoma is a malignant tumor that can be difficult to detect because its symptoms are similar to other uterine conditions. Past treatment with radiation therapy to the pelvis can increase the risk of uterine sarcoma.
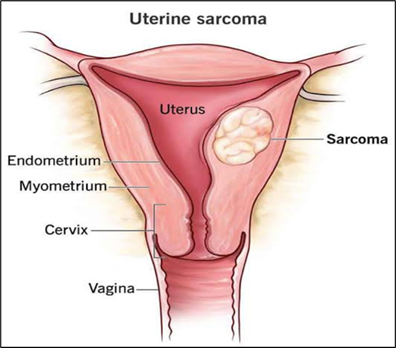
Figure 2
Types of uterine sarcoma are as follows:
Uterine leiomyosarcoma – The most common type which is develops in the muscle walla of the uterus.
Endometrial stromal sarcoma - A less common type which is forms in the tissue that connects the uterine lining to the walls of the uterus.
Undifferentiated uterine sarcoma – The rarest type which can begin in the uterine mucles or uterine lining.
Signs of uterine sarcoma
Bleeding that is not part of menstrual periods.
Bleeding after menopause.
A mass in the vagina.
Pain or feeling of fullness in the abdomen.
Frequent urination
The following FIGO staging system is used for uterine leiomyosarcomas and endometrial stromal sarcomas:
1.Stage I –In stage I, the tumor is found in the uterus only. The stage I is divided into stages IA and IB.
In stage IA the tumor is 5 centimeters or smaller.
In stage IB the tumor is larger than 5 centimeters.
2. Stage II – In stage II the tumor has spread beyond the uterus but has not spread beyond the pelvis. Stage II is divided into stages IIA and IIB:
In stage IIA the tumor has spread to the ovary, fallopian tube or connective tissue around the uterus.
In stage IIB the tumor has spread to the other tissue in the pelvis.
3.Stage III– In stage IA the tumor has spread into tissue in the abdomen. Stage III is divided into IIIA, IIIB, IIIC:
In stage IIIA the tumor has spread to one site in the abdomen.
In stage IIIB the tumor has spread to more than one site of the abdomen.
In stage IIIC the tumor has spread to lymph nodes in the pelvis and around the abdominal aorta (largest blood vessels in the abdomen)
Stage IV – In stage IV is divided into stages IVA and IVB.
In stage IVA the tumor has spread into the bladder or rectum.
In stage IVB the tumor has spread to distant parts of the body.
Treatments-
1. Surgery-
Total Hysterectomy: Removal of the uterus and cervix. This can be done via:
Vaginal Hysterectomy: Through the vagina.
Total Abdominal Hysterectomy: Through a large abdominal incision.
Total Laparoscopic Hysterectomy: Through small incisions using a laparoscope.
Bilateral Salpingo-Oophorectomy: Removal of both ovaries and fallopian tubes.
Radical Hysterectomy: Removal of the uterus, cervix, part of the vagina, and possibly nearby lymph nodes.
2. Chemotherapy
Involves using drugs to kill cancer cells or stop their growth.
Systemic Chemotherapy: Taken orally or injected, allowing the drug to circulate throughout the body.
Regional Chemotherapy: Administered directly into specific areas, such as the abdomen.
3. Targeted Therapy
Targets specific cells, usually causing less harm to normal cells compared to chemotherapy or radiation. Monoclonal Antibody Therapy: Laboratory-made antibodies that attach to specific targets on cancer cells, helping to kill them or inhibit their growth. For example, Bevacizumab is used for advanced or recurrent endometrial cancer.
Here’s a comprehensive overview of the risk factors and protective factors associated with endometrial (uterine) cancer:
Risk Factors
1. Endometrial Hyperplasia
- Abnormal thickening of the endometrium that can increase the risk of developing endometrial cancer.
2. Estrogen Exposure
- Estrogen-Only Hormone Therapy: Long-term use of estrogen alone (especially in postmenopausal women without a uterus) increases cancer risk.
- Menstrual Factors:
- Early Menstruation: Starting periods at a young age increases lifetime estrogen exposure.
- Late Menopause: Reaching menopause later extends estrogen exposure.
- Reproductive History: Never being pregnant increases estrogen exposure over a lifetime.
3. Tamoxifen Use
- While effective for breast cancer prevention, long-term use of tamoxifen can elevate endometrial cancer risk, particularly in postmenopausal women.
4. Obesity and Metabolic Factors
- Obesity: Associated with higher estrogen levels, particularly in postmenopausal women.
- Weight Gain: Gaining weight as an adult increases risk.
- Metabolic Syndrome: Includes high waist circumference, blood sugar, blood pressure, and triglycerides.
- Type 2 Diabetes: Linked to an increased risk of endometrial cancer.
5. Genetic Factors
- Lynch Syndrome: An inherited disorder significantly raises the risk of endometrial cancer.
- Polycystic Ovary Syndrome (PCOS) and Cowden Syndrome: Both are linked to higher cancer risk.
- Family History: Having a first-degree relative with endometrial cancer increases risk.
Protective Factors-
1.Pregnancy and Breastfeeding
- Lower estrogen levels during these periods reduce endometrial cancer risk.
2. Hormonal Contraceptives
- Use of combined oral contraceptives decreases risk, with a protective effect that can persist after discontinuation.
3. Weight Management
- Bariatric surgery has shown to lower endometrial cancer risk and improve related health conditions.
4. Physical Activity
- Regular exercise helps maintain a healthy weight, lowers estrogen levels, and improves insulin sensitivity, potentially reducing cancer risk.
5. Medications
- Bisphosphonates: Some studies suggest these drugs may lower endometrial cancer risk due to their anti-inflammatory properties.
- Aspirin: Regular use has been associated with reduced risk, potentially due to its anti-inflammatory effects.
CONCLUSION- Uterine cancer, primarily endometrial cancer, is a significant health concern affecting women, particularly those over 50. Early detection through regular gynecological exams and awareness of symptoms—such as abnormal bleeding—can lead to better outcomes. Treatment options typically include surgery, radiation, and chemotherapy, tailored to the cancer's stage and type. Ongoing research is crucial for improving prevention, diagnosis, and treatment strategies. Maintaining a healthy lifestyle and being vigilant about reproductive health can contribute to reducing risks associated with this disease. Overall, awareness and education are key in addressing uterine cancer effectively.
REFERENCES
- American Cancer Society. Endometrial Cancer (https://www.cancer.org/cancer/endometrial-cancer.html). Accessed 3/21/2023.
- Centers for Disease Control and Prevention. Uterine Cancer (https://www.cdc.gov/cancer/uterine/pdf/uterine_facts.pdf). Accessed 3/21/2023.
- Mahdy H, Casey MJ, Crotzer D. Endometrial Cancer (https://www.ncbi.nlm.nih.gov/books/NBK525981/). 2022 Sep 26. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022 Jan-. Accessed 3/21/2023.
- The American College of Obstetricians and Gynecologists. Endometrial Cancer (https://www.acog.org/womens-health/faqs/endometrial-cancer). Accessed 3/21/2023.
- U.S. Department of Health & Human Services. Office on Women’s Health. Uterine Cancer (https://www.womenshealth.gov/cancer/uterine-cancer). Accessed 3/21/2023.
- U.S. National Cancer Institute. Cancer Stat Facts: Uterine Cancer (https://seer.cancer.gov/statfacts/html/corp.html). Accessed 3/21/2023.
- U.S. National Cancer Institute. Uterine Cancer — Patient Version (https://www.cancer.gov/types/uterine/patient/uterine-sarcoma-treatment-pdq). Accessed 3/21/2023.
- Henley SJ et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 126, 2225–2249 (2020). - PMC - PubMed
- Sung H et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer. J. Clin 71, 209–249 (2021). - PubMed
- Morice P, Leary A, Creutzberg C, Abu-Rustum N & Darai E Endometrial cancer. Lancet. 387, 1094–1108 (2016). - PubMed
- Siegel RL, Miller KD & Jemal A Cancer statistics, 2018. CA. Cancer. J. Clin 68, 7–30 (2018). - PubMed
- Calle EE, Rodriguez C, Walker-Thurmond K & Thun MJ Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med 348, 1625–1638 (2003).
- Prospective study showing that excess body weight was assocaited with increased death rates for endometerial cancer and all malignancies combined.
- Lauby-Secretan B et al. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N. Engl. J. Med 375, 794–798 (2016). - PMC - PubMed
- Rahib L et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer. Res 74, 2913–2921 (2014). - PubMed


 Maya Jadhav * 1
Maya Jadhav * 1
 Prof. Komal Chavan 2
Prof. Komal Chavan 2
 Dr.kavita kulkarni 3
Dr.kavita kulkarni 3
 10.5281/zenodo.13986487
10.5281/zenodo.13986487