Abstract
Joint pain is one of the common disorders caused due to various factors like lack of nutrients vitamin and age, general health condition physical weakness, disease, etc. To prepare the transdermal joint relief patch is medicated adhesive patch that is specialist are ongoing to explore for new method that can efficiently and painlessly transmit blood stream. It is a place on a skin to deliver a specific dose of medication through the skin and into the blood stream. The transdermal drug delivery system is a one of the novel drug delivery systems which over comes arises from the conventional dosage form. The transdermal patches are pharmaceuticals preparation of varying sizes containing one or more active ingredient to the systemic circulation. In the patch materials are used main API are (Thymol camphor, menthol camphor, natural camphor mustard oil, kalonji oil, mustard oil, clove oil, eucalyptus oil,) Polymers are (Ethyl cellulose, Polyethylene glycol, HPMC, Tween- 80,). The patch were formulated using combination of polymer and propylene glycol as a plasticizer. The physicochemical evaluation of the patches performed.
Keywords
Transdermal Patches, Arthritis ,Camphor, Systemic Circulation
Introduction
JOINT PAIN AND ARTHERITIS
Arthritis is derived from the Greek term “disease of the joints.”It is defined as an acute or chronic joint inflammation that often co-exists with pain and structural damage. Artheritis is not synonymous with arthralgia, which refers to pain localizeds to a joints, regardless of the origin of the pain (which may or may not be due to joint inflammation). There are several different types of artheritis, with management being different for each. History and physical examination are crucial in recognizing the type of artheritis, while additional laboratory and imaging may sometimes be necessary of confirming the diagnosis. This activity outlines the evaluation and treatment of artheritis and explains the role of the interprofessional team in managing patients with this condition. Arthritis is the swelling and tenderness of one or more of your joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. Although theres no cure for arthritis, treatment have improved greatly in recent years and, for many types of artheritis, particularly inflammatory artheritis, theres a clear benefit in starting treatment at an early stage. Cartilage is a firm but flexible connective tissue in your joints. It protects the joints by absorbing the pressure and shock created when you move and put stress on them.1 Arthritis represents one of the most prevalent chronic health problems and is a leading cause of disability. More than 40 millions people in the india have artheritis or chronic joint symptoms that are often accompanied by joint pain. By the year 2020, this number is expected to reach 60 million. The most common form of artheritis is osterartheritis affecting an estimated 21 million aduld in the india. Other common artheritis condition include rheumatoid arthritis and gout. Arthritis is the inflammation of a joint, which can include infiltration of inflammatory cells (monocytes), synovial hyperplasia, bone erosion and formation, narrowing of the joint space, and ankylosis of the joint. The most common form of arthritis is osteoarthritis . osteoarthritis is a degenerative disease characterized by damage to the articular cartilage, changes in subchondral and marginal bone, synovitis and capsular thickening, typically affecting weight bearing joints (knee and hips). Pain in osteoarthritis is located and use-related, occurring during movement or weight bearing. Rheumatoid arthritis is an autoimmune disease of the synovium that leads to an inflammatory poly-arthritis. It is characterized pattern of affected joint and by morning stiffness, joint swelling and tenderness. Pain in rheumatoid arthritis improve with movement. Gout represent one of the most painful forms of arthritis. A metallic disorder with high blood levels of uric acid. The metatarsophalangeal joint (big toe) is typically affected, but other joints can be invoved as well, including the knee. A reduction in the normal amount of its cartilage tissue causes some forms of arthritis.[2]
- Osteoarthritis
- Rheumatoid arthritis (RA)
- Gout
- Septic arthritis
- Inflammatory mono-arthritis
Osteoarthritis:
Osteoarthritis is a chronic, degenerative disorder of unknown cause characterised by gradual loss articular cartilage. It is the most prevalent disease in our society, with a worldwide distribution. It ranks fourth in health impact in woman and eight in men in the western world.[3]
Symptoms:
- Mild Swelling
- Pain in Joints (Hipes, knee and Hands are most common)
- Stiffness
Rheumatoid Arthritis:
Rheumatoid Arthritis is a chronic, systemic, inflammatory autoimmune disorder causing symmetrical polyarthritis of large and small joints, typically presenting between the ages of 30 and 50 year. The most common inflammatory arthritis, it afflicts an estimated 25 men and 54 women per 100,000 population and is responsible for 250,000 hospitalizations and 9 million physician visits in the UA each year.[4]
Symptoms:
- Painfull
- Affects Joint Lining
Gout
Gout is a disease condition which often is considerd as a form of inflammatory arthritis. Unlike arthritis, gout is not a degenerative process. Its generally characterized by frequent attacks of swelling, redness, and a tender, warm and puffy expression of bone joint areas. (5)
Symptoms:
- Redness and swelling in joints
- Stiffness.
TRANSDERMAL PATCHES
Transdermal drug delivery systems (TDDS), also known as “patches,” are dosage forms designed to deliver a therapeutically effective amount of drug across a patient’s skin. In order to deliver therapeutic agents through the human skin for systemic effects, the comprehensive morphological, biophysical and physicochemical properties of the skin are to be considered. Transdermal delivery provides a leading edge over injectables and oral routes by increasing patient compliance and avoiding first pass metabolism respectively. Transdermal delivery not only provides controlled, constant administration of the drug, but also allows continuous input of drugs with short biological half-lives and eliminates pulsed entry into systemic circulation, which often causes undesirable side effects. The TDDS review articles provide valuable information regarding the transdermal drug delivery systems and its evaluation process details as a ready reference for the research scientist who is involved in TDDS. With the advancement in technology Pharma industries have trendified all its resources. Earlier we use convectional dosage form but now we use novel drug delivery system. One of greatest innovation of novel drug delivery is transdermal patch. The advantage of transdermal drug delivery system is that it is painless technique of administration of drugs. Transdermal patches are now widely used as cosmetic, topical and transdermal delivery systems. These patches represent a key outcome from the growth in skin science, technology and expertise developed through trial and error, clinical observation and evidence-based studies that date back to the first existing human records. This review begins with the earliest topical therapies and traces topical delivery to the present-day transdermal patches, describing along the way the initial trials, devices and drug delivery systems that underpin current transdermal patches and their actives. This is followed by consideration of the evolution in the various patch designs and their limitations as well as requirements for actives to be used for transdermal delivery. The properties of and issues associated with the use of currently marketed products, such as variability, safety and regulatory aspects, are then described. The review concludes by examining future prospects for transdermal patches and drug delivery systems, such as the combination of active delivery systems with patches, minimally invasive microneedle patches and cutaneous solutions, including metered-dose systems.[6]
Advantages
- First pass metabolisms of drug get avoided.
- Gastrointestinal incompatibilities get avoided.
- Self-medication is possible.
- Duration of action gets extended & predictable.
- Unwanted side effects get minimized.
- Number of doses get reduces which improve patient compliance.
Disadvantages
- Chances of allergic reactions at the site of application like- itching, rashes, local edema etc.
- Larger molecular size of drug (above 1000) creates difficulty in absorption.
- Barrier function of skin varies from site to site on the same or different person.
- Drug with hydrophilic character is less suitable as compare to drug with lipophilic character because of their low permeability.[7]
Types of transdermal patches
-
- Single-layer Drug-in-Adhesive:
The adhesive layer of this system also contains the drug. In this type of patch the adhesive layer not only serves to adhere the various layers together, along with the entire system to the skin, but is also responsible for the releasing of the drug. The adhesive layer is surrounded by a temporary liner and a backing.
-
- Multi-layer Drug-in-Adhesive:
The multi-layer drugin adhesive patch is similar to the single-layer system in that both adhesive layers are also responsible for the releasing of the drug. The multi-layer system is different however that it adds another layer of drug- inadhesive, usually separated by a membrane (but not in all cases). This patch also has a temporary liner-layer and a permanent backing.
-
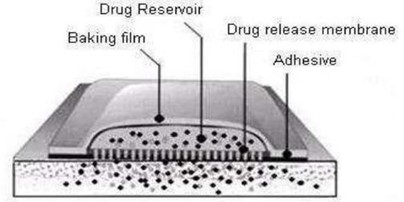
- Reservoir:
Unlike the Single-layer and Multi-layer Drug-inadhesive systems the reservoir transdermalsystem has a separate drug layer. The drug layer is a liquid compartment containing a drug solution or suspension separated by the adhesive layer. This patch is also backed by the backing layer. In this type of system the rate of release is zero order.
-
- Matrix:
The Matrix system has a drug layer of a semisolid matrix containing a drug solution or suspension. The adhesive layer in this patch surrounds the drug layer partially overlaying it.
-
- Vapour Patch:
In this type of patch the adhesive layer not only serves to adhere the various layers together but also to release vapour. The vapour patches are new on the market and they release essential oils for up to 6 hours. The vapours patches release essential oils and are used in cases of decongestion mainly. Other vapour patches on the market are controller vapour patches that improve the quality of sleep. Vapour patches that reduce the quantity of cigarettes that one smokes in a month are also available on the market.[6]
Fig.1 Types of Transdermal patch[8]

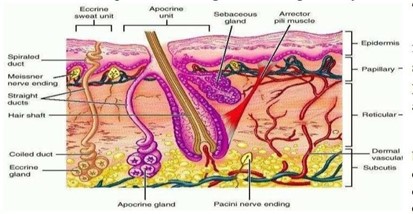
Anatomy and physiology of skin
Human skin comprises of three distinct but mutually dependent tissues: The stratified, vascular, cellular called as “epidermis” Underlying dermis of connective tissues, Hypodermis.
Epidermis
The multilayered epidermis varies in thickness, depending on cell size and number of cell layers of epidermis, ranging from 0.8 mm on palms and soles down to 0.06 mm on the eyelids. Stratum corneum. This is the outermost layer of skin also called as horny layer. It is approximately 10 mm thick when dry but swells to several times this thickness when fully hydrated. It contains 10 to 25 layers of dead, keratinized cells called corneocytes. It is flexible but relatively impermeable. The stratum corneum is the principal barrier for penetration of drug. The architecture of horny layer may be modeled as a walllike structure. In this model, the keratinized cells function as protein “bricks” embedded in lipid “mortar.” The lipids are arranged in multiple bilayers.
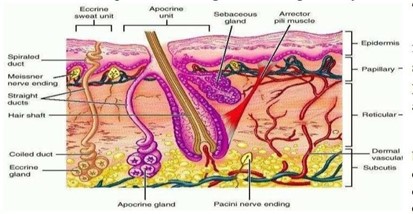
Fig2. Structure of human skin [9]
There is sufficient amphiphilic material in the lipid fraction, such as polar free fatty acids and cholesterol, to maintain a bilayer form. Viable epidermis is situated beneath the stratum corneum and varies in thickness from 0.06 mm on the eyelids to 0.8 mm on the palms. Going inwards, it consists of various layers as stratum lucidum, stratum granulosum, stratum spinosum and the stratum basal. In the basal layer, mitosis of the cells constantly renews the epidermis and this proliferation compensates the loss of dead horney cells from the skin surface. As the cells produced by the basal layer move outward, they alter morphologically and histochemical, undergoing keratinization to form the outermost layer of stratum corneum.
Dermis
Dermis is 3 to 5 mm thick layer and is composed of a matrix of connective tissue, which contains blood vessels, lymph vessels and nerves. The cutaneous blood supply has essential function in regulation of body temperature. It also providesnutrients and oxygen to the skin while removing toxins and waste products. Capillaries reach to within 0.2 mm of skin surface and provide sink conditions for most molecules penetrating the skin barrier. The blood supply thus keeps the dermal concentration of a permeate very low and the resulting concentration difference across the epidermis provides essential concentration gradient for transdermal permeation.
Hypodermis
The hypodermis or subcutaneous fat tissue supports the dermis and epidermis. It serves as a fat storage area. This layer helps to regulate temperature, provides nutritional support and mechanically protection. It carries principal blood vessels and nerves to skin and may contain sensory pressure organs. For transdermal drug delivery, drug has to penetrate through all these three layers and reach into systemic circulation while in case of topical drug delivery only penetration through stratum corneum is essential and then retention of drug in skin layers is desired.[6]
Components of transdermal patches
-
- Polymer Matrix
The polymer controls the release of the drug from the device. The following criteria should be satisfied for a polymer to be used in transdermal patches.
- Molecular weight, chemical functionality of the polymer should be such that the specific drug diffuses properly and gets released through it.
- The polymer should be stable.
- The polymer should be nontoxic
- The polymer should be easily of manufactured
- The polymer should be inexpensive
- The polymer and its degration product must be non-toxic or non- antagonistic to the host.
- large amounts of the active agent are incorporated into it.
Types of polymers: -
-
- Natural polymers: Cellulose derivative, Gelation, Waxes, Proteins, Gum, Shellac, Natural rubber,starch.
- Synthetic Elastomers: Hydrin rubber, silicone rubber, Nitrile, Acrylonitrile, Neoprene.
- Synthetic polymers: Polyvinyl alcohol, polyvinyl chloride, polyethylene, polypropylene, polyamiode, polyurea, epoxy.
-
- Drug: -
Drug solution in direct contact with release liner. Physiochemical properties: -
- The drug should have a molecular weight less than 1000 Daltons.
- The drug should have affinity for both lipophilic and hydrophilic phases.
- The drug should have a low melting point.
Biological properties
- The drug should be potent with a daily dose of the order of a mg/day.
- The half life (t½) of the drug should be short.
- The drug must not produce allergic response.
- Tolerance to the drug must not develop under the near zero-order release file of transdermal patches.
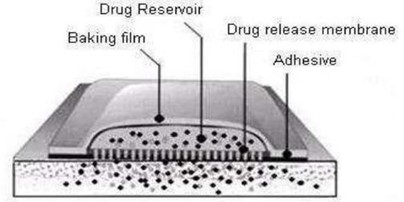
Fig.3 : Different parts of transdermal patch[10]
-
-
Permeation Enhancer: -
The flux J. of drug across the skin can be write
As J = D dc/dx
J = the Flux
D = diffusion coefficient
C = Concentration of the diffusing spectes X = Spatial coordinate
Solvent: -
These compounds increase penetrationpossibly by swelling the polar pathway. e.g.: Water alcohols–Methanol & ethanol, / Dimethyl acetemide Propylene glycol and Glycerol.
Surfactants: -
The ability of a surfactant to alter penetration is a function of the polar head group and the hydrocarbon chain length.
-
- Anionic surfactant:- Sodium lauryl sulphate Diacetyl sulphosuccinate
- Nonionic Surfactant:- Pluronic F127, Pluronic F68
- Bile Salt: - Sodium taurocholate, Sodium deoxycholate.
Miscellaneous Chemicals: -
These include urea, a hydrating and keratolytic agent; N, N dimethyl-mtoluamide; calcium thioglycolate; anticholinergic agents. Some potential permeation enhancers have recently been described but the available data on their effectiveness sparse. These include eucalyptol, di-omethyl-ß-cyclodextrin and soyabean casein
Enhance the permeation e.g. Urea, calcium thioglycolate. 7.4 Other excipients: -
Adhesives: -
The pressure sensitive adhesive can be positioned on the face of the device or in the back of the device.
-
-
- It should not be irritant
- It should be easily removed
- It should not leave an un washable residue on the skin
- It should have excellent contact with the skin.
- Physical & chemical compatibility with the drug
- Permeation of drug should not affected.
- Linear: -
Protect the patch during storage. The linear is removed prior to use.
-
- Backing: -
Protect the patch from the outer environment.
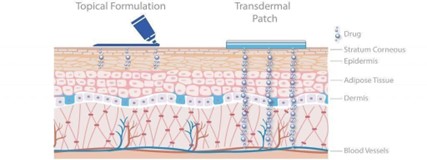
MECHANISM OF ACTION OF TRANSDERMAL PATCHES
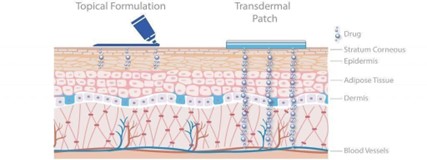
Fig: 4 Mechanism of Action of Transdermal Patches
Joint pain patches work in the best way in your body. The natural ingredients in these patches form a better formulation in these patches. When you place them, you can build healthy cartilage while giving instant relief. It contains several natural herbs, including dried ginger, menthol, camphor, and others, which are included in the knee patches. The herbs are combined with cream, which is then added to a hot melt knee adhesive. It was refined into a patch from that blend. A drug is applied in a relatively high dosage to the inside of a patch, which is worn on the skin for an extended period of time. Through the diffusion process the drug enters the bloodstream directly through the skin. Transdermal drug delivery (TDD) is one potential route for the systemic delivery of drugs that offers many advantages over the traditional drug- delivery systems with a small concentration of drugs for slow release and without passage through gastrointestinal tract. In contrast to widely accepted ointment medicinal forms, TDD allows drugs to be administered in an individual-dose regimen and provides prolonged treatment. Being able to release the drug in a timely manner, TDD is useful for controlled release (CR) action over an extended period of time. Polymeric membranes prepared from natural and synthetic origins are usually used for TDD, of which some arecommercially exploited. TDD has the advantage of no passage through the gastrointestinal tract, unlike the oral administration route, because the decomposition and hepatic first-pass biotransformation are easily circumvented, and drugs at lower dosages can be delivered for a longer time. Transdermal drug delivery systems (TDDSs) is a self-contained distinct dosage forms which delivers the drug by means of transdermal patch through the epidermis of the skin at a predetermined and sustained rate with low biological half-life. It provides systemic delivery of drug through increased bioavailability with reduced dosing frequency The skin has a number of considerable advantages over other routes of administration when used as a site of drug delivery, including increased patient compliance, the ability to avoid gastric irritation, no hepatic first-pass metabolism thus enhancing the bioavailability. minimize the risk of systemic side effects by reducing plasma concentrations contrast to oral therapy, provide a sustained release of drug at the site of application; rapid termination of therapy by removal of the patch, the reduction of fluctuations in plasma levels of drugs, and avoid pain associated with parenteral.[11]
Benefits of herbal joint pain patches
-
-
- Combats pain and inflammation
- Reduces the time it takes to heal from injuries
- Increases flexibility and mobility
Herbal ingredients which are used in formulation
- Kalonji Oil
Synonyms: -
Black cumin
Biological Source: -
Nigella Sativa (black caraway also known as black cumin, Nigella, kalonji,) is an annual flowering plant.
Family: -
Ranunculaceae.
Chemical constituents: -
Kalonji contain about 0.4 – 0.45% volatile oil. The volatile oil of the drug contains saturated fatty acid which include: nigellone that is the only component of the carbonyl fraction of the oil, thymoquinone (TQ) thymohydroquinone (THQ), Thymol, carvacrol, volatile oil of the seed
Uses :
-
- Kalonji seed have anti-inflammatory properties that can treat Various chronic inflammation.
- It is known for healing joint pains by proving lubrication between the joint
- Improve creaky joints.
- Reduce inflammation.
- Accelerate weight loss

Fig 5 :- kalonji oil [15)
-
Clove oil
Synonyms: -
Eugenia cariophylata
Biological source: -
Cloves consist of dried flower buds of Eugenia caryophyllus, (Family: Myrtaceae).
Chemical constituents:
clove oil contain about 15 to 20 % of volatile oil, 10% to 13% of tannis, resins, chromosomes and eugenic. The volatile oil of the drug contain eugenol 89% and 5 to 15% eugenol acetate and beta- cairofileno.
Uses
- Relieves muscular pain.
- Promotes faster healing.
- Reduce irritability.[16]

Fig 6 : Clove oil
-
Mustard oil
Synonymes:
Vegetable oil
Biological source:
Musterd oil obtained from natural seed of Brassica nigra Koch or Brassica juncea L. czern
Chemical constituens :
Musterd oil ha about 60% monounsaturated fatty acid (42% erucic acid & 12% oleic acid ), it has about 21% polyunsaturated fats.
Uses :
Musterd oil use as a –
- Dental analgesic
- carminatives
- Stimulants
- Aromatic

Fig 7. Musterd oil[18]
-
EUCALYPTUS OIL
Synonyms:
Blue gum, genus eucalyptus, eucalyptus comphora
Biological source:
Eucalyptus oil is made from the fresh leaves and branch tops of the eucalyptus plant.
Chemical constituents :
eucalyptus oil has eucalyptol, pinene

Fig 8. Eucalyptus Flower and Fruit [19,20]
Uses
- Relieves stuffy nose.
- Clears respiratory complaints.
- Eases sore muscle and joint pain.
- Post-surgery pain reliever.
- Promotes oral health.
- Promotes scalp health and clear lice. 7: Boosts immunity.
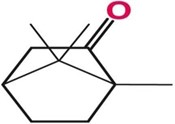
4.CAMPHOR
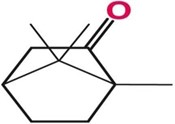
Fig:9. Structure of Camphor
IUPAC Name:
1,7,7-trimethylbicyclo [2.2.1] heptan-
2-one
Molecular Formula:
C10H160
Physical Appearance:
Colour :
colourless to white
Odour:
arrogating odour
Taste:
aromatic taste
Boiling Point:
399F at 760 mmHg
Melting point :
345F
Solubility:
Insoluble in water and Soluble in ethanol
Uses:
-
- Used as a plasticizer and chemical intermediate, also used as an additive to explosives, varnishes, lacquers, insecticides, fungicides, pharmaceuticals, cosmetics and flavourings.[12]
- It helps to heal muscular pains and aches as well as rheumatism.
- It also helps to decreases cholesterol levels in the body.[13]

Fig 10. Menthol Camphor

Fig 11. Thymol Camphor

Fig 12. Natural Camphor[14
MATRIALS AND METHOD
Material
Drugs chemicals used
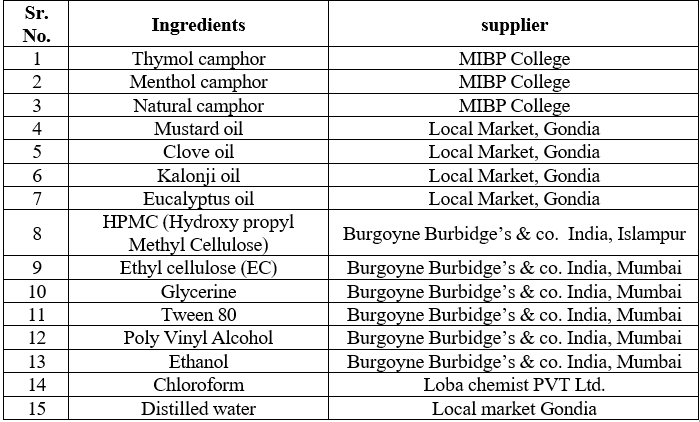
Table no. 5 list of ingredients used
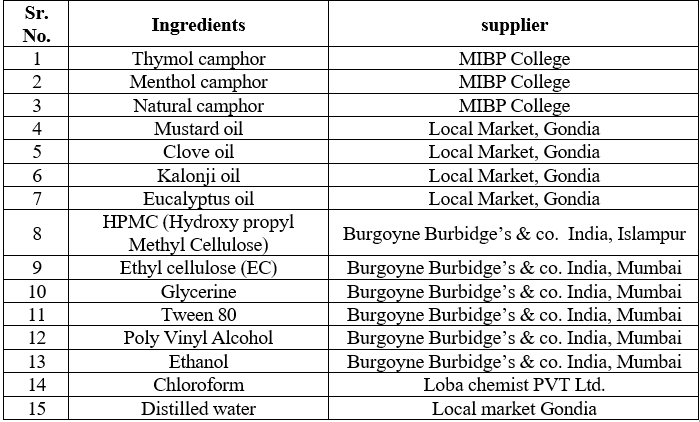
Composition of Herbal Pain Relief Patches
Table no.6 :- Batches prepared

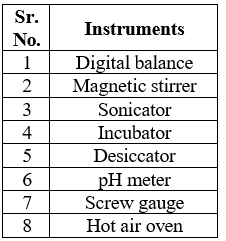
List of instruments used
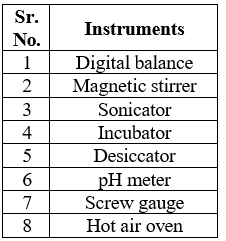
Table No.7 :- List of the Instruments used
Methods
Chemical Test Table no. 8

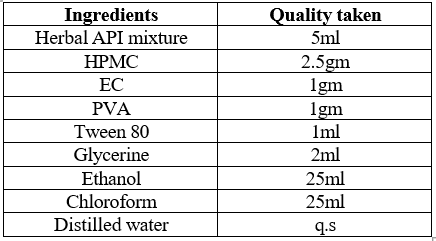
Formula:
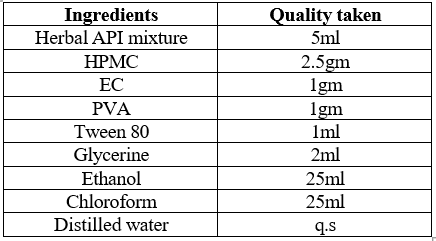
Table no.9: - formula for transdermal patches
Procedure for preparation of herbal joint pain relief patch
-
-
-
- The active pharmaceutical ingredients were prepared by combining requisite amount of camphor in Mustard oil, kalonji oil and 2-3 drops of clove oil and eucalyptus oil, is added and dissolve in ethanol.
- The drug matrix was prepared by dissolving HPMC and EC in methanol. To this solution Tween 80 was added and stirred.
- Dried at room temperature for 24hrs.
- The dry films were removed and wrapped in aluminium foil and kept in a desiccator until used.
- The so prepared films were stick to adhesive layer of bandage which was purchased from local market.
EVALUATION PARAMETERS
Physical appearance:
Physical appearance the formulated patches were found to be fear, smooth, uniform. flexible in their physical appearance and free from entrapment of air bubble
Thickness of the patch:
The thickness of the drug loaded patch is calculated in different prints by using a digital micrometre, or travelling microscope, dial gauges and determines the average thickness and standard deviation for the same to ensure the thickness of the prepared patch Paich will have an equal thickness of every points. The variation of thickness within the patch and patch to patch can be calculated.
Moisture content:
Individually weighed patches are kept in the desiccators having fused calcium chloride at room temperature for 24 hours After 24 Hours the patches are to be reweighed and percentage moisture content is calculated by the formula & Moisture content (Initial Weight-Final weight) X 100 initial weight
Moisture uptake.
The weighed films are to be kept in desiccators at room temperature for 24 hrs containing saturated solution of potassium chloride in instruct to maintain 84% RH, after 24 hrs the films are to be reweighed and determined the percentage moisture uptake from the mentioned Moisture uptake (Final weight Initial weight X 100)/Initial weight
Folding endurance:
This was determined by repeatedly folding the film at the same place until it broke the number of period the films could be folded at the same place without breaking/ cracking gave the value of folding endurance
Weight uniformity:
Weight variation is studied by individually weighing 10 randomly selected patches and calculating the average weight. The individual weight should not deviate significantly from the average weight.
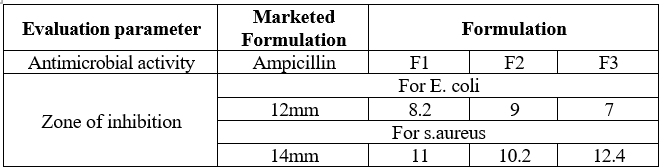
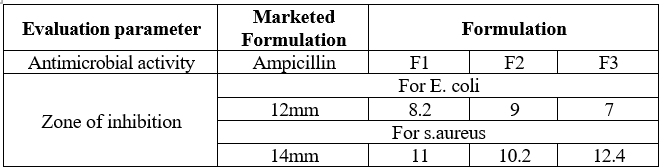
Antimicrobial activity :.
Cup plate of cylinder plate method
This method relies on the diffusion of an antibiotic from a vertical cavity or a cylinder through the solidified agar layer in a petri plate. The growth of test microorganism in observe to be inhibited in a circular area or zone around the cavity containing antibiotic solution.
Steps involved in cup plate method are given below,
-
-
-
- A liquefied assay medium (43–45-degree c.) is inoculated by the suspension of test microorganism.
- This inoculated test culture medium poured and spread on sterile petri or preprepared agar plates.
- Standard and test antibiotic solution of known concentration are prepared in appropriate solutions, which are then added to sterile cavities prepared on solid medium.
- Uniform volume of sodium should be added to each cavity to fill them sufficiently if paper discs are used, they should sterilize first, then dipped in standard or test Cup solution and finally placed on medium surface.
- The plates are allowed to stand at room temperature or at 4degree c. for 1-2 hours. This is the period of pre Incubation diffusion which minimises the effect of variation time between the applications of different solutions.
- All plates are then incubated at temperature 32–35-degree c. for 18-24 hours.
- The diameters or areas of circular inhibition zone produce by standard and antibiotic solution are accurately measured.
Flatness :
A transdermal patch should possess a smooth surface and should not constrict with time. This can be demonstrated with flatness study. For flatness determination, one strip is cut from the centre and two from each side of patches. The length of each strip is measured and variation in length is measured by determining percent constriction. Zero percent constriction is equivalent to 100 percent flatness.
L2 = Final length of each strip L1 = Initial length of each strip
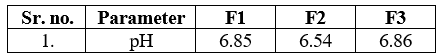
pH of the patch:
Apparatus baker, pH meter, stirrer, wash bottle.The pH meter was calibrated using standard buffer solution. About 1 patch dissolve in buffer solution and dissolved in 50ml of phosphate buffer and its pH was measured.
RESULT AND DISCUSSION
Chemical test

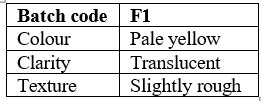
Physical appearance
Table No:-10.Physical appearance
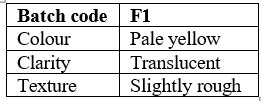
From the above observation, we can concluded that F3 has all the ide ideal physical characteristics.
Fig: 18. Physical appearance of transdermal patches

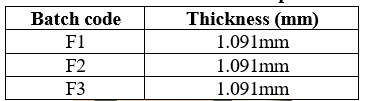
Thickness of patch
Table: no. 11:- Thickness of patch
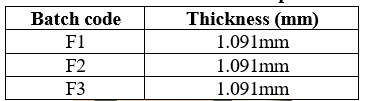
Fig 19. Thickness of patch

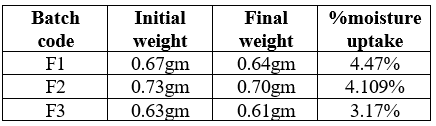
Moisture content
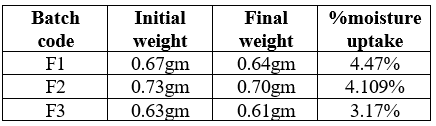
Table No.12:- Moisture Content
The moisture content was found to be higher in batches F1, F2,and F3, which might be due to HPMC. The lower moisture content in the formulations helps them to remain stable and become a completely dried and brittle film. Again, low moisture content protects the material from microbial contamination and bulkiness.
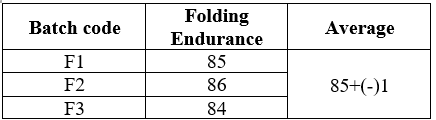
Folding endurance
Table no.13:- Folding endurance
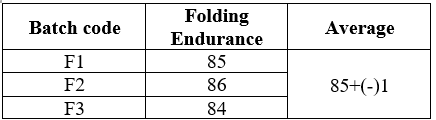
The folding endurance of F1 was measured and found to be 85+(-)1.The folding endurance values of all the patches were found satisfactory which indicates that the patches prepared using PEG 400 in a concentration of 30% w/w of polymer were having optimum flexibility and were not brittle.
Weight uniformity
Weight of patches=total weight of 10 patches/10
=0.67+0.55+1.35+0.73+0.46+0.37+0.38+1.56+0.37+0.78/ 10
= 7.81/10
=0.781
Antimicrobial testing: -
Fig 20. Zone of inhibition

Determination of pH:-
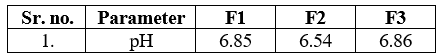

Fig 21. pH meter
The Ph test was performed for base formulation. The pH of the cream was found to be in the range of 5.6 to 6.8 which is good for skin.
CONCLUSION
Transdermal drug delivery system has been in existence for a long time. In the past, the most commonly applied systems were topically applied creams and ointments for dermatological disorders. Kalonji oil, eucalyptus oil, Mustard oil, Camphor and Clove Oil were used for its analgesic property. In the present investigation, herbal transdermal patches were formulated using HPMC and EC polymer by solvent evaporation technique. The developed formulation showed good physicochemical properties like thickness, weight variation, drug content, folding endurance, moisture content. As per the result of diffusion study we can conclude that the formulation exhibited significant analgesic activity and the promising analgesic effect may be attributed which seems to be responsible. The result indicates that maximum release shows satisfactory results. So, it can be concluded that such a medicated adhesive type patches of herbal ingredient could be a good carrier in transdermal drug delivery as well as topical route for joint pain relief.
REFERENCE
- Shayan Senthelal, et.al.,“ Arthritis” Published by National Library of Medicine, National for Biotechnology Information June 20, 2023.
- Neugebauer, V., Han, J.S., Adwanikar, H., Fu, Y. and ji, G., 2007. Techniques for assessing knee joint pain in arthritis. Molecular pain,3, pp.1744-8069
- Inam Haq, et al. “Osteoarthritis” Published by Article in Postgraduate Medical Journal 01/79-377-381
- Vikas Majithia, et al. “Rheumatoid Arthritis Diagnosis and Managements” Published by The American Journal of Medicine 2007 120, 936-939
- Narrottam Pal. “The Gout” Published by Bhaskar Pharmacy College, Hyderabad, India 2019
- Audumber Digamber Mali et al., “an updated review on transdermal drug delivery system” international journal in scientific research. ISSN No.2395- 3616-page no. 244, 254
- Nidhi Sharma, “Review on transdermal patches” Published by International Journal Review Article, Volume 7, Issue to June 05, 2018
- Nidhi Sharma a brief “review on transdermal patches” organic and medicinal chemistry internation journal (2018) Issn no.2474-7610 pg. no.001-005
- Rohit Tiwari et, al,. “Transdermal drug delivery system - Review”. International journal of therapeutic application.2013-14 Page No.22-38
- Rajesh N, et, al., “Formulation and Evaluation of Biopolymer based Transdermal drug delivery” International journal pharm science. 2010; 2(2): Page No. 142-147
- Mr. Joint knee pain patch reviews- Do This Knee Pain Relief Patch Really Works? Must Read Before You Buy! (outlookindia.com)
- Stankov, S.V., 2012. Definition of inflammation, cause of inflammation and possible anti- inflammation strategies. Open inflame J,5(1), ppt.1-9.
- Camphor | C10H160- PubChem (nih.gov)
- https://images.app.goo.gl/C4eUtK7QxT4Bi1nN9
- Shehla Nazir,et.al.,“Kalonji seeds in strenthing immune system”. Published by International Journal of Care Report and Studies in 2018. Page no.55-56.
- Urooj Khan, et al "A review on biological and therapeutical uses of syzygium aromaticum linn (Clove) Based on phytochemistry and pharmacological evidences” Published by International Journal of Botany Studies 2020.
- Vipin Kesharwani et.al.,“ A Review on Therapeutics Application of eucalyptus oil”International Journal of Herbal Medicine 2018; 6(6): 110-115
- https://www.google.com/imgres?imgurl=https://assets.cntravelle r.in/photos/60ba2326bfe773a828a46ef1/1:1/w_3465,h_346 5,c_limit/F4FJ4K.jpg&tbnid=6B2AqjVHgmjemM&vet=1&imgrefu rl=https://www.cntraveller.in/story/punjab-bengal-many- flavours-mustard-oil-plus-five recipes/&docid=0DykrgrpazAUSM&w=3465&h=3465&hl=en- US&source=sh/x/im/m1/4&kgs=c1fc1d56883ff038&shem=ab me,trie
- http:/www.lemis.com
- http:/www.Cambridgemask.com
- Ghosh B, Preethi Gb, Mishra R, Parcha V. Transdermal Delivery of Ibuprofen on Its Prodrugs by Passive Diffusion and Iontophoresis. Int J Pharm Pharm Sci. 2010; 2(1):79-85.
- Barry Bw., The Lpp Theory of Skin Penetration Enhancement. Maturitas. 1998; 29: 165–85.
- Ghafourian T, Zandasrar P, Hamishekar H, Nokhodchi A, the Effect of Penetration Enhancers on Drug Delivery Through Skin: A Qsar Study. J Control Release.2004; 99:
- Montia D, Saettone Mf, Giannaccini B, Angeli Dg, Enhancement OFTransdermal Penetration of Dapiprazole Through Hairless Mouse Skin. J Control Release.1995; 33: 71–7.
- Bharadwaj S, Gupta Gd, Sharma Vk. Topical Gel: AN Novel Approach for Drug Delivery. J Chem. Bio. Phy. Sci. 2012; 2(2): 856-867.
- Sharma N, Parashar B, Sharma S, Mahajan U. Blooming Pharma Industry With Transdermal Drug Delivery System. Indo Global J Pharm. Sci. 2012;2(3): 262-278.


 Poonam C. Rahangdale*
Poonam C. Rahangdale*














 10.5281/zenodo.11481456
10.5281/zenodo.11481456