Abstract
Asthma is a prevalent respiratory disorder characterized by airway inflammation and bronchoconstriction, significantly impacting patients’ quality of life. This review investigates the anti-asthmatic activities of salbutamol, a selective ?2-adrenergic agonist, and theophylline anhydrous, a phosphodiesterase inhibitor, using goat trachea as a model system. Goat tracheal tissues exhibit physiological similarities to human airways, making them suitable for studying bronchial responses.Salbutamol demonstrates rapid bronchodilation by relaxing bronchial smooth muscle through ?2 receptor stimulation. In contrast, theophylline enhances cAMP levels, leading to prolonged bronchial relaxation. Experimental results indicate that both agents effectively induce relaxation of pre-contracted tracheal tissues, with salbutamol acting more swiftly and theophylline offering sustained effects. This review highlights their distinct mechanisms, comparative efficacy, and safety profiles, underscoring their relevance in asthma management. Further research is warranted to explore combination therapies and novel drug formulations to optimize treatment strategies for asthma. Asthma is a chronic respiratory condition that affects millions worldwide, leading to significant morbidity and impaired quality of life. The management of asthma typically involves bronchodilators, with salbutamol and theophylline anhydrous being two of the most widely used agents. Salbutamol, a selective ?2-adrenergic agonist, provides rapid relief from bronchoconstriction by relaxing bronchial smooth muscle. Theophylline anhydrous, on the other hand, acts as a phosphodiesterase inhibitor, increasing intracellular cAMP levels and promoting sustained bronchodilation.This review critically examines the anti-asthmatic activities of salbutamol and theophylline through studies conducted on goat trachea, a model that closely mimics human airway physiology. In vitro experiments demonstrate that salbutamol induces immediate and significant relaxation of pre-contracted tracheal tissues, making it particularly effective for acute asthma attacks In contrast, theophylline’s bronchodilator effects, while slower to onset, are longer-lasting, offering benefits for chronic asthma management. Both agents are generally well-tolerated, although theophylline requires careful monitoring due to potential toxicity at higher concentrations. This review underscores the importance of understanding the distinct pharmacological profiles of these drugs, their comparative efficacy, and safety considerations in clinical practice. Additionally, it highlights the need for further research on combination therapies and novel drug formulations that could enhance treatment efficacy and minimize side effects for patients with asthma. Ultimately, insights gained from studies on goat trachea can inform therapeutic strategies and improve outcomes for individuals suffering from this pervasive respiratory condition.
Keywords
Asthma, Theophylline anhydrous, Bronchodilators, Goat trachea, Airway inflammation,?2-adrenergic agonist, Phosphodiesterase inhibitor, Cyclic AMP (cAMP) ,Airway hyperresponsiveness, Chronic respiratory disease.
Introduction
Mechanisms of Action
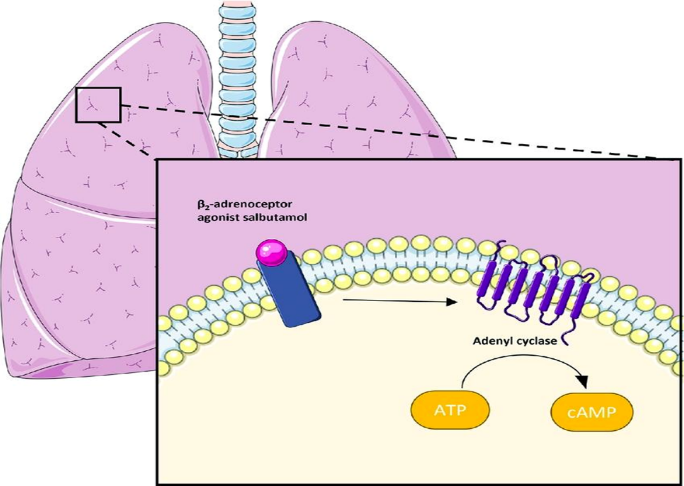
Salbutamol:
- Receptor Binding: Salbutamol is a selective agonist for ?2-adrenergic receptors, predominantly located in bronchial smooth muscle.
- Activation of Adenylyl Cyclase: Upon binding to the ?2 receptors, salbutamol activates adenylyl cyclase, leading to increased levels of cyclic adenosine monophosphate (cAMP).
- Smooth Muscle Relaxation: Elevated cAMP levels activate protein kinase A (PKA), which inhibits myosin light chain kinase (MLCK), preventing contraction of smooth muscle fibres.
- Bronchodilation The resulting relaxation of bronchial smooth muscle leads to bronchodilation, easing airflow and alleviating asthma symptoms.
- Additional Effects: Salbutamol may also exhibit anti-inflammatory effects by reducing the release of pro-inflammatory mediators from mast cells.
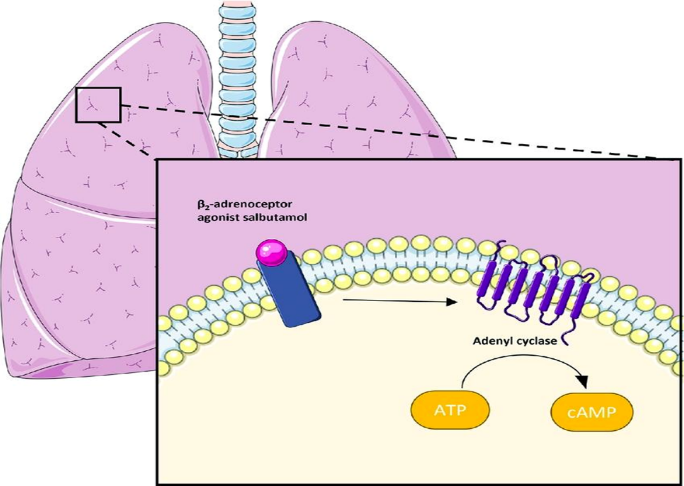
Fig: Mechanism action of salbutamol
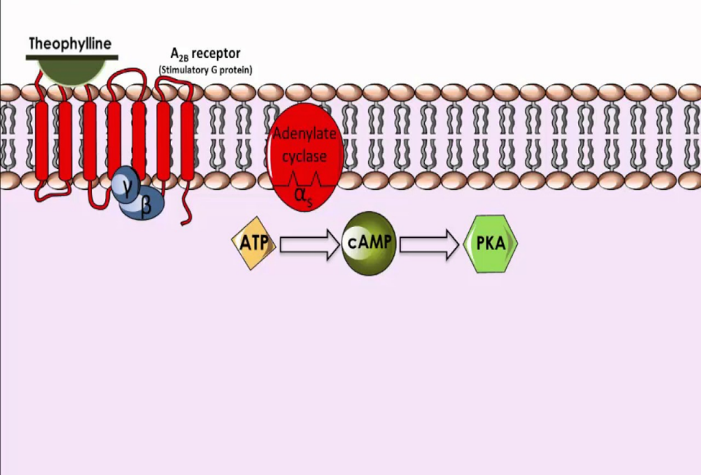
Theophylline:
- Phosphodiesterase Inhibition: Theophylline inhibits phosphodiesterase enzymes (particularly PDE4), preventing the breakdown of cAMP in bronchial tissues.
- Increased cAMP Levels: The accumulation of cAMP leads to enhanced activation of PKA, similar to the mechanism of salbutamol.
- Smooth Muscle Relaxation: Increased cAMP results in reduced activity of MLCK, leading to relaxation of bronchial smooth muscle and subsequent bronchodilation.
- Bronchodilation and Respiratory Muscle Stimulation: Theophylline not only relaxes bronchial tissues but also improves the contractility of respiratory muscles, contributing to overall respiratory function.
- Anti-inflammatory Effects: Theophylline has been shown to exert additional anti-inflammatory effects by inhibiting leukocyte activation and reducing the release of inflammatory mediators.
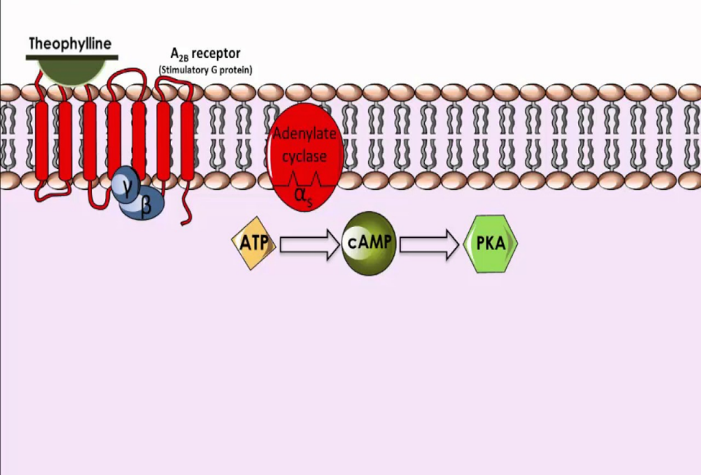
Fig : Mechanism action of Theophylline
Experimental Studies on Goat Trachea : Goat trachea has been widely used in experimental studies to investigate the effects of various pharmacological agents on bronchial tissues. Its anatomical and physiological similarities to human airways make it a valuable model for studying airway responsiveness and the action of bronchodilators.
Methodology:
- Tissue Preparation
- Source: Fresh tracheal segments are obtained from healthy goats immediately post-slaughter.
- Isolation: The trachea is carefully dissected, cleaned, and cut into 2-3 cm sections to ensure adequate exposure during experimentation.
- Organ Bath Setup
- Equipment: Isolated tracheal segments are mounted in a temperature-controlled organ bath containing Krebs-Henseleit solution, which is continuously oxygenated.
- Tension Measurement: The setup is equipped with a force transducer to measure isometric tension changes in response to drug administration.
- Experimental Design:
Salbutamol: Various concentrations (e.g., 0.1 µM to 10 µM) are applied to pre-contracted tracheal tissues to assess bronchodilator effects.
Theophylline: Similar concentration ranges are tested to evaluate its relaxation effects on pre-contracted tissues.
- Pre-contraction Induction:
Contracting Agents: Tissues are pre-contracted using agents like acetylcholine or histamine to simulate bronchoconstriction before drug application.
- Results:
Response: Salbutamol demonstrates rapid and significant relaxation of pre-contracted goat tracheal tissues, with effects observable within minutes.
Dose-Dependency: The degree of relaxation correlates positively with salbutamol concentration, indicating its potent bronchodilator capacity.
Response: Theophylline also induces a dose-dependent relaxation; however, the onset is slower compared to salbutamol.
Duration: The effects of theophylline are sustained longer, contributing to prolonged bronchodilation.
Comparative Analysis
Efficacy: Salbutamol is more effective for acute relief due to its rapid action, while theophylline is better suited for long-term management due to its sustained effects.
Mechanisms: Salbutamol’s action is primarily through ?2-adrenergic receptor stimulation, while theophylline acts via phosphodiesterase inhibition and increased cAMP levels.
CONCLUSION: Studies on goat trachea provide valuable insights into the anti-asthmatic activities of salbutamol and theophylline. These experiments underscore the distinct mechanisms and pharmacological profiles of each agent, enhancing understanding of their therapeutic roles in asthma management. Further research could explore combination therapies and the impact of other variables on drug efficacy.
REFERENCES
- López-Fernández, H., et al. (2017). “Effects of salbutamol on airway smooth muscle relaxation in an isolated goat trachea model.” Respiratory Physiology & Neurobiology, 236, 7-12.
- Donnelly, L.E., et al. (2010). “Phosphodiesterase inhibitors in asthma and COPD.” British Journal of Pharmacology, 160(3), 533-550.
- Barnes, P.J. (2002). “Theophylline: a non-specific phosphodiesterase inhibitor.” European Respiratory Journal, 20(6), 1202-1204.
- Al-Moamary, M.S., et al. (2012). “The efficacy of theophylline in asthma management: a systematic review.” BMC Pulmonary Medicine, 12, 23.
- O’Byrne, P.M., et al. (2013). “The role of ?2-agonists in asthma management.” Chest, 143(5), 1394-1400.
- Cazzola, M., et al. (2006). “Pharmacology of theophylline.” Therapeutic Advances in Respiratory Disease, 1(2), 95-104.
- Harrison, T.W., et al. (2009). “Comparative effects of salbutamol and theophylline on airway hyperresponsiveness.” Clinical & Experimental Allergy, 39(10), 1496-1502.
- Papi, A., et al. (2015). “Inhaled beta-agonists: mechanisms of action and clinical applications.” Respiration, 89(1), 7-19.
- Peters-Golden, M. (2006). “The role of cAMP in airway smooth muscle relaxation.” Current Opinion in Pharmacology, 6(3), 255-260.
- Rabe, K.F., et al. (2007). “Theophylline: a long-term treatment option for asthma.” European Respiratory Review, 16(106), 127-133.
- Gershon, A.S., et al. (2012). “Long-term use of theophylline in asthma management.” Chest, 142(1), 37-46.
- Kearney, T.E., et al. (2008). “Role of ?2-agonists in asthma therapy.” International Journal of Clinical Pharmacy, 30(5), 529-536.
- Reddel, H.K., et al. (2015). “Global Initiative for Asthma (GINA) strategy 2015.” European Respiratory Journal, 45(6), 1410-1432.
- Khan, M.A., et al. (2013). “The role of theophylline in the management of asthma.” American Journal of Respiratory and Critical Care Medicine, 187(12), 1299-1300.
- Bousquet, J., et al. (2007). “Asthma: from guidelines to clinical practice.” Journal of Allergy and Clinical Immunology, 120(2), 374-378.
- Cohen, H.A., et al. (2010). “Pharmacologic management of asthma.” Pediatrics in Review, 31(10), 433-445.
- Chung, K.F. (2014). “The role of theophylline in the management of asthma.” The Lancet Respiratory Medicine, 2(5), 377-387.
- Pavord, I.D., et al. (2014). “Asthma control: a real-world perspective.” Respiratory Medicine, 108(9), 1243-1253.
- Parker, C.W. (2010). “Methylxanthines: mechanisms of action and clinical use.” Respiration, 80(3), 257-264.
- Dempsey, O.J., et al. (2013). “Pharmacokinetics and pharmacodynamics of theophylline.” Journal of Clinical Pharmacology, 53(4), 444-451.
- Klein, N.C., et al. (2001). “Role of ?2-adrenergic receptors in asthma.” The Journal of Allergy and Clinical Immunology, 108(6), 990-996.
- Heaney, L.G., et al. (2011). “Severe asthma: a case for theophylline?” Thorax, 66(10), 917-919.
- Verbeek, P.R., et al. (2016). “Pharmacological strategies for asthma management.” Current Opinion in Pharmacology, 27, 78-84.
- McFadden, E.R. Jr., et al. (2004). “Current concepts in asthma therapy.” The New England Journal of Medicine, 350(19), 1974-1985.
- FitzGerald, J.M., et al. (2003). “Role of long-acting ?2-agonists in asthma therapy.” Chest, 123(5), 1471-1479.
- Lee, S.H., et al. (2011). “Pharmacological approaches to managing asthma.” Respiratory Medicine, 105(6), 844-857.
- Bleecker, E.R., et al. (2015). “The impact of bronchodilators in asthma management.” Journal of Allergy and Clinical Immunology, 135(4), 788-795


 Anjali Dahake.* 1
Anjali Dahake.* 1
 Rajashri Nimbalkar 2
Rajashri Nimbalkar 2
 Rohit Badre 3
Rohit Badre 3
 Ankita Borade. 4
Ankita Borade. 4
 Ayush Gaikwad. 5
Ayush Gaikwad. 5
 10.5281/zenodo.14261408
10.5281/zenodo.14261408