Abstract
Proton pump inhibitors (PPIs) are widely prescribed for various gastrointestinal conditions, but their overutilization can lead to unnecessary healthcare costs and potential adverse effects. The objective of the present work is to assess the overutilization of PPIs among patients in a tertiary care hospital, examining the characteristics of PPI therapy and identifying factors associated with their overuse. A prospective study was conducted in a tertiary care hospital to analyze the prescription patterns of PPIs. Data were collected on the types of PPIs prescribed, patient demographics, and reasons for PPI use, with a focus on identifying instances of overuse. Pantoprazole was the most commonly prescribed PPI, accounting for 68.42% of total prescriptions, with the highest usage observed in the 18-60 year age group. Rabeprazole, Esomeprazole, Omeprazole, and Lansoprazole followed in decreasing order of prescription frequency. The majority of PPI prescriptions (78%) were for patients aged 18-60 years. Overuse of PPIs was found in 57.3% of cases, primarily due to co-prescription (59.40%) and among patients with peptic ulcer disease (PUD) (61.5%). Pantoprazole had the highest proportion of overuse when prescribed as a co-prescription (67.67%). In conclusion significant overutilization of PPIs, particularly due to co-prescription and extended durations beyond recommended guidelines. Addressing PPI overuse requires targeted interventions to optimize prescribing practices, including regular reassessment and education for healthcare providers on appropriate PPI use. Implementing these strategies can enhance patient safety, reduce unnecessary costs, and improve the overall quality of care
Keywords
PPI, NHS, Overutilization, Rational.
Introduction
Proton-pump inhibitors (PPIs) are a class of medications that cause a profound and prolonged reduction of stomach acid production. They do so by irreversibly inhibiting the stomach’s proton pump.[1] The primary mechanism of action of proton pump inhibitors is to act on the gastric parietal cells to lower down the stomach’s acidity. Gastric parietal cells are found in the gastric lining and are responsible for secreting hydrochloric acid. Proton pump inhibitors (PPIs) are currently favored over other gastric acid suppressive medications because of their high efficacy, good tolerance, safety profile, and affordable costs with both original and generic preparations.[2]Thus they have been adopted worldwide among primary care providers and their presence is ubiquitous within the armamentarium of the modern gastroenterologist.[3]PPIs as a class of medication also have a high prevalence of being prescribed for poorly defined reasons or for conditions where PPIs have not been shown to be beneficial. The Evidence suggests PPIs are often overused with 25– 70% of prescriptions having no appropriate indication.[4] PPI use is associated with several adverse consequences including Clostridium difficile infection, community acquired pneumonia, osteoporosis, hypomagnesaemia, and kidney injury3-8. Considering this, PPI prescription should be reserved for patients where there is a clear indication, and clinicians should consider stopping PPIs when the indication is unclear. [5]
Methodology
Study design: Prospective study and interventional study will be carried out to assess proton pump inhibitor utilization and analysis among in-patients in a tertiary care hospital. Individuals aged 18 years or above in in-patient service with at least one dispensing for PPIs were identified as PPI users and were included in the study. Data will be collected from samples using convenient sampling method between January- June 2023.
Study site: Srinivas Institute of Medical Science & Research Centre, Mukka
Study Duration: 6 months.
Sample Size: 1714
Ethical Clearance: Ethical clearance was obtained from the Institutional Ethics Committee: [IEC] of Srinivas Institute of Medical science and Research Centre [SIMS & RC], Mangalore.
- Inclusion Criteria: Individuals aged 18 years or above, New user (patient not on PPI past 1year) , ? Patients prescribed with oral PPI
- Exclusion Criteria: Patient with parenteral PPI,
Source of Data Collection: Patient and Medical records. The study period is divided into 3 phases.
Phase I:
(A) Preparation for the study: Preparation of Patient’s Data Collection form: Data collection form includes the patient’s demographic details and the list of PPI medicines that they take and duration of the PPI and even the Indication for which the PPI was been prescribed.
Phase II:
- Patient selection: The patients for the study was selected based on the inclusion and exclusion criteria.
- Obtaining inform consent: During the hospital visit, we explained the patients about the study and obtained the patient consent for collecting data. The data was collected by personal discussion with the patient.
- Based on the data collected we categorized the patients
Phase III:
The data collected was analyzed using Microsoft Excel Data Analysis: Statistical Analysis involves collecting and scrutinizing every data sample in a set of items from which samples can be drawn and a suitable statistical test will be applied to analyze the data. ? the collected data will be analyzed using Microsoft Excel.
Results
- Characteristics Of Proton Pump Inhibitor (Ppi) Therapy
In the current study, Pantoprazole was the most widely prescribed PPI, accounting for 68.42% of total prescriptions (42.6% male, 57.3?male), primarily among the 18–60-year age group. Rabeprazole followed at 15.2% (53.8% male, 46.15?male), then Esomeprazole at 8.18% (57.14% male), Omeprazole at 7.01% (58.33% male), and Lansoprazole at 1% (100% male). The majority of PPI use (78%) was observed in the 18–60-year age group compared to 22% in those over 60. This data helps understand PPI usage patterns, assess age and gender disparities, and guide clinical decisions and treatment trends in a tertiary care hospital.
Table No:1 Characteristics Of Proton Pump Inhibitor (PPI) Therapy
|
PPI
|
Overall(n=171)
n(%)
|
18-60years
(n=135)n(%)
|
>60 years (n=36)n(%)
|
Newuser
|
Males
|
Females
|
|
Characteristics of PPI therapy
|
|
Pantoprazole
|
117(68.42)
|
M
|
F
|
Total
|
M
|
F
|
Total
|
42
|
24
|
18
|
|
57
|
35
|
92(78.63)
|
16
|
9
|
25(21.37)
|
|
Rabeprazole
|
26(15.2)
|
8
|
11
|
19(73.06)
|
6
|
1
|
7(26.94)
|
9
|
5
|
4
|
|
Esomeprazole
|
14(8.18)
|
6
|
7
|
13(92.85)
|
1
|
0
|
1(7.15)
|
6
|
2
|
4
|
|
Omeprazole
|
12(7.01)
|
5
|
5
|
10(83.33)
|
0
|
2
|
2(16.67)
|
2
|
0
|
2
|
|
Lansoprazole
|
2(1.16)
|
0
|
1
|
1(50)
|
0
|
1
|
1(50)
|
0
|
0
|
0
|
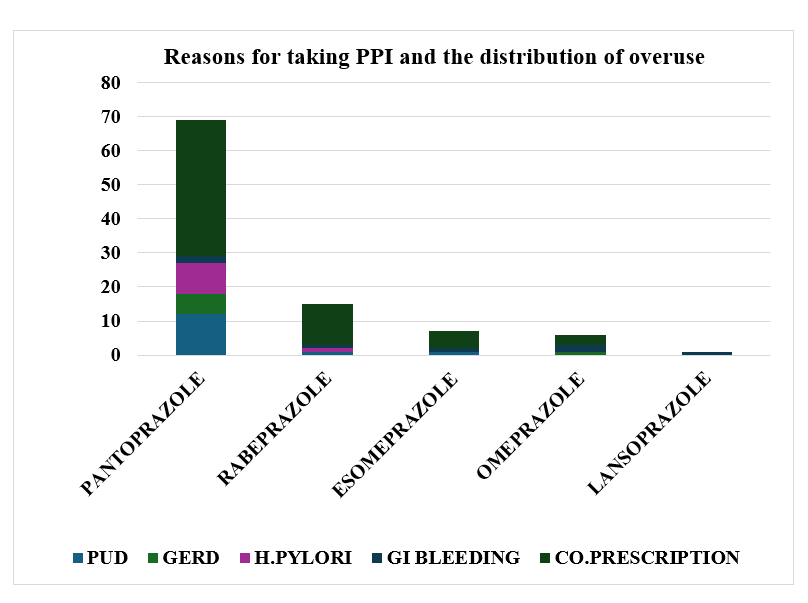
2] Reasons For Taking Ppi And The Distribution Of Overuse
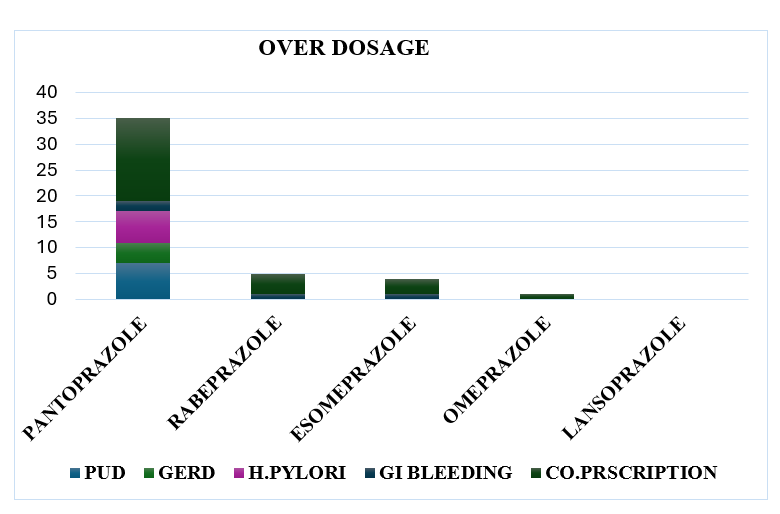
The study categorized reasons for PPI use and overuse (57.3%). The majority of overuse was observed in co-prescription scenarios (59.40%), with higher overuse in PUD indications (61.5%). Rabeprazole exhibited the highest abuse rate (61.5%), while Lansoprazole had the lowest (50%). Notably, Pantoprazole showed high overuse when co-prescribed (67.67%) and for GI bleeding (40%). Rabeprazole demonstrated high overuse in co-prescription (75%) and less in GI bleeding and H. Pylori eradication (50%). Esomeprazole had high overuse in co-prescription (55.55%) and less for GI bleeding. Omeprazole had high overuse in co-prescription and less in GERD. This data is crucial for understanding PPI usage patterns, identifying potential misuse, and refining prescription practices to align with guideline.
Table No.2: Reason for taking Proton Pump Inhibitor and their distribution of overuse
|
PPI
|
Drug Use
|
PUD
|
GERD
|
H. Pylori
|
GI
Bleeding
|
Co- prescription
|
|
Pantoprazole
|
Overuse n (%)
|
12(63.15)
|
6(54.5)
|
7(46.6)
|
2(40)
|
40((59.7)
|
|
Overuse % per total overusing sample
|
12.24
|
6.122
|
7.14
|
2.04
|
40.81
|
|
Total (117)
|
19
|
11
|
15
|
5
|
67
|
|
Rabeprazole
|
Overuse n (%)
|
2(50)
|
0(0)
|
1(50)
|
1(50)
|
12(75)
|
|
Overuse % per total overusing.
sample
|
2.04
|
0
|
1.02
|
1.02
|
12.24
|
|
Total (26)
|
4
|
2
|
2
|
2
|
16
|
|
Esomeprazole
|
Overuse n (%)
|
2(66.66)
|
0(0)
|
0(0)
|
1(100)
|
5(55.55)
|
|
Overuse % per total
overusing sample
|
2.04
|
0
|
0
|
1.02
|
5.10
|
|
Total (14)
|
3
|
0
|
1
|
1
|
9
|
|
Omeprazole
|
Overuse n (%)
|
0(0)
|
1(50)
|
0(0)
|
2(66.66)
|
3(42.85)
|
|
Overuse % per total overusing sample
|
0
|
1.02
|
0
|
2.04
|
3.06
|
|
Total (12)
|
0
|
2
|
0
|
3
|
7
|
|
Lansoprazole
|
Overuse n (%)
|
0(0)
|
0(0)
|
0(0)
|
1(50)
|
0(0)
|
|
Overuse % per total overusing.
sample
|
0
|
0
|
0
|
1.02
|
0
|
|
Total (2)
|
0
|
0
|
0
|
2
|
0
|
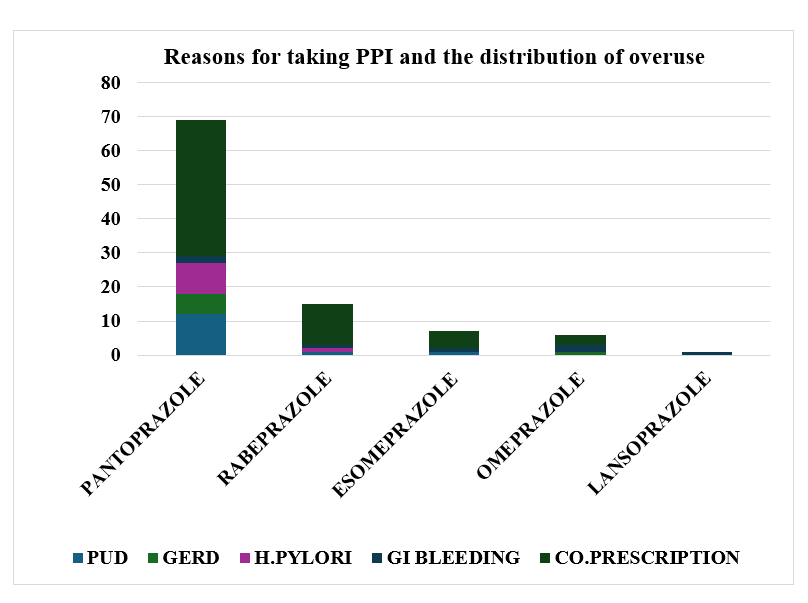
Fig.2: Reason for taking Proton Pump Inhibitor and their distribution of overuse.
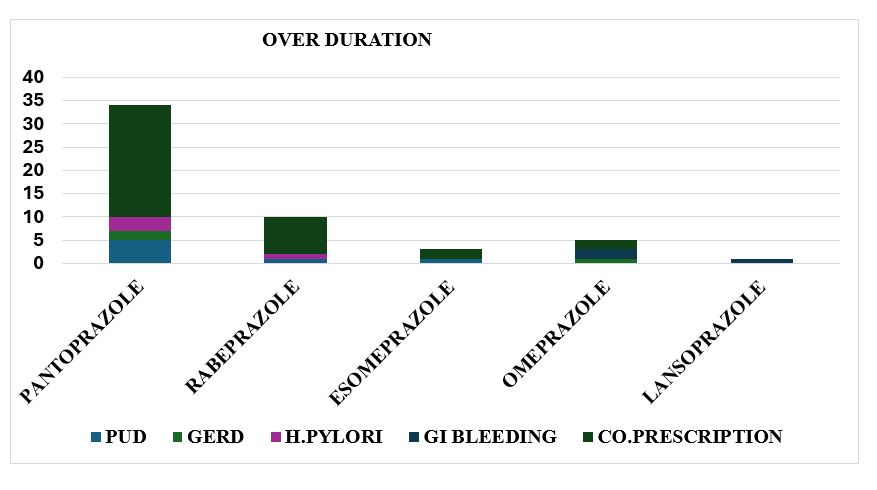
3] Overuse Of PPI Categories
The data revealed total overuse of PPIs to be 57.3%, categorized into overuse of duration (75.51%) and overuse of dosage (24.48%), regardless of sex or age group. Overuse was more prevalent among individuals using PPIs for gastro protection (co-prescription) (72.44%) compared to those diagnosed with gastro related disease (27.55%). This information can guide targeted interventions to prevent unnecessary PPI prescriptions, potentially reducing healthcare costs and improving patient care. Identifying overuse by specific types of PPIs helps pinpoint areas needing modification to mitigate potential harm and health concerns.
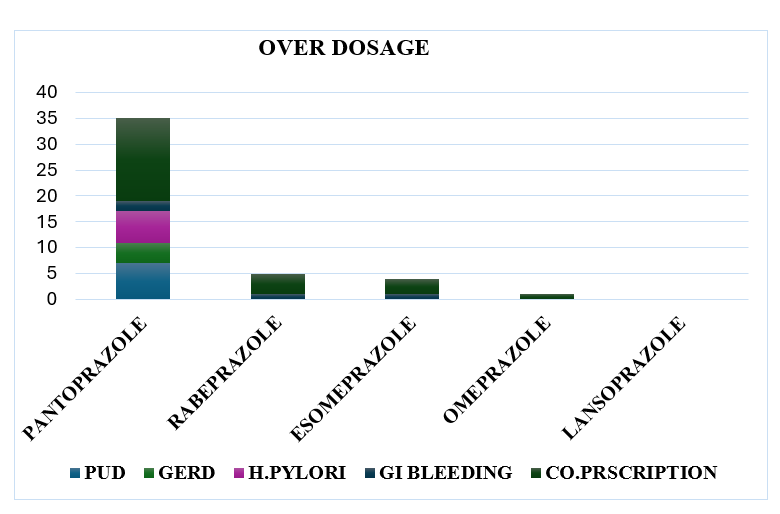
Fig no 3: Overuse of PPI categories (Dosage)
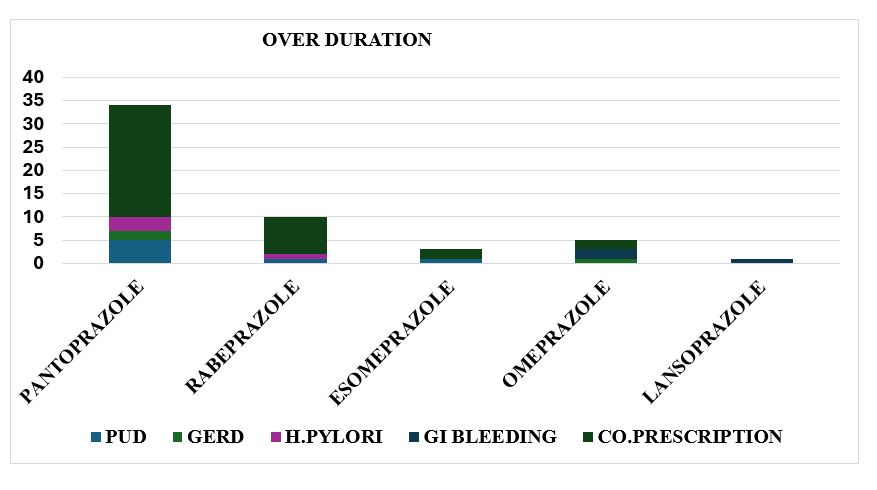
Fig no 4: Overuse of PPI categories (Duration)
DISCUSSIONS
PPIs are widely prescribed globally, with increasing concerns about their overuse. A 2017 US study noted a moderate number of outpatient visits with PPI prescriptions, a number that escalated by 2019. Our study offers insights into PPI utilization patterns, revealing that most long-term users fall within the 30-49 age group. This finding echoes Liu et al.'s research, which identified a similar trend among long-term PPI users aged 18-65 years. [1] Interestingly, the present study revealed high prevalence of PPI utilization among male patients, particularly those in middle age. This finding contradicts the results of the study by HoteitM etal., where utilization of PPI was observed more in Females.[11] The study analyzed specific proton pump inhibitors (PPIs) prescribed to patients, finding Pantoprazole to have the highest prescription rate, predominantly within the 18-60-year age range. Rabeprazole followed closely, with lower usage rates. Esomeprazole, Omeprazole, and Lansoprazole followed in sequence. PPI usage was predominantly observed in the 18-60-year age group, potentially due to a smaller representation of participants in the >60-year age group. The study revealed two main contributors to excessive PPI utilization: high-dosage regimens and prolonged treatment durations. A notable portion of individuals surpassed recommended treatment durations, while others were prescribed high-dosage therapies. These findings align with previous studies, such as [9], which also reported significant proportions exceeding recommended treatment durations set by NICE guidelines.[9] Among all Proton Pump Inhibitors (PPIs), Pantoprazole exhibited the highest incidence of excessive use. Moreover, individuals prescribed PPIs as part of co-prescription were more likely to over utilize them compared to those prescribed PPIs solely for clinical diagnostic purposes. These findings are consistent with those reported by Savarino et al. [10]which showed majority of PPI users had co-prescription with NSAIDS with standard and low-dose therapy (3.6 %), which was similar to the findings of the result Hendrix I et al in Australia in 2017[11]. Study also found small portion of PPI users were using long-term, and undoubtedly, majority of them could have been brought down to withdraw from this therapy.[11]
Despite numerous guidelines and extensive published reports highlighting the importance of appropriate use of PPIs and the potential disadvantages of inappropriate usage, the inappropriate prescribing of PPIs has persisted in clinical practice. For instance, Gianninietal.,[12]reported that PPIs were inappropriately prescribed for approximately high proportion of outpatients, and an even higher rate of inappropriate PPI use was observed in patients by the findings Thomas Y et al.,[13]In current study, PPIs were inappropriately prescribed in majority of cases. Although the indications for PPI usage have expanded, the prevalent inappropriate prescription of PPIs for non-indicated purposes is a widespread issue, a trend also evident in a study encompassing over 45 hospitals in China.[14]These observations raise growing concerns regarding both the economic costs and safety implications, particularly when considering long-term usage.
CONCLUSION
In conclusion, this study highlights inappropriate PPI utilization, including unapproved indications and excessive dosages, often coupled with inappropriate co-prescription with antibiotics. To optimize PPI use, a "Step Down Therapy" approach is recommended once symptoms are alleviated. Efforts should focus on limiting PPI treatment to appropriate indications and selecting suitable options, supported by educational initiatives for healthcare practitioners. Regular monitoring and re-evaluation by physicians are essential to ensure continued necessity.
REFERENCES
-
-
-
- LiuY,ZhuX,LiR,ZhangJ,ZhangF.Protonpumpinhibitorutilizationandpotentiallyinappropriate prescribing analysis: insights from a single-centred retrospective study.BMJopen.2020;10(11)
- Strand DS, Kim D, Peura DA. 25 Years of Proton Pump Inhibitors: A ComprehensiveReview,GutLiver. 2017;11:27–37.
- HaroonM,YasinF,GardeziSK,AdeebF,WalkerF.Inappropriateuseofprotonpumpinhibitors among medical inpatients: a questionnaire-based observational study. JRSMshortreports.2013;4(8)
- BatuwitageBT, KinghamJGC,MorganNE.Inappropriateprescribingof protonpumpinhibitorsinprimarycare.PostgradMedJ.2007;83:66–68.
- NICE Clinical Knowledge Summary (last revised June 2020); Scenario: NSAID’s – prescribing issues:
- NICE Clinical Knowledge Summary (last revised June 2020); Corticosteroids - Oral
- NICE clinical knowledge summary - Antiplatelet treatment for secondary prevention of cardiovascular disease (CVD) (last revised August 2020); [cited 31 March 2021].
- Hoteit M, Mattar E, Allaw R, Abou Rached A. Epidemiological study assessing theoveruse of proton pump inhibitors in Lebanese population. Middle East Journal ofDigestive Diseases.2020;12(4):265.
- Kelly OB, Dillane C, Patchett SE. The inappropriate prescription of oral proton pumpinhibitorsinthehospitalsetting:aprospectivecross-sectionalstudy.DigDisSci.2015;60:2280–6
- Savarino V, Marabotto E, Zentilin P. Proton pump inhibitors: use and misuse in theclinicalsetting. ExpertRevClinPharmacol. 2018;11:1123–34
- Hendrix I, Page AT, Korhonen MJ. Patterns of high-dose and long-term proton pumpinhibitor use: a cross-sectional study in six South Australian residential aged careservices.Drugs RealWorldOutcomes.2019;6:105–13.
- Giannini EG, Crespi M, Djahandideh A. Appropriateness of proton pump inhibitorstreatment in clinical practice: prospective evaluation in outpatients and perspectiveassessmentofdrugoptimization.DigLiverDis.2020;52:862–8.
- Thomas L, Culley EJ, Gladowski P. Longitudinal analysis of the costs associated withinpatient initiation and subsequent outpatient continuation of proton pump inhibitortherapyforstressulcerprophylaxisinalargemanagedcareorganization.JManagCarePharm.2010;16:122–9.
- YingJ,LiL-C,WuC-Y.Thestatusofprotonpumpinhibitoruse:aprescriptionsurveyof45hospitalsinChina.RevEspEnfermDig.2019;111:738–43


 Riya Ann Reji*
Riya Ann Reji*
 Satish S.
Satish S.
 10.5281/zenodo.14307806
10.5281/zenodo.14307806